Number 4 Use Supplements If Necessary
As per the introduction earlier, supplements should not be your only strategy.
You should work out what is triggering you, and remove it.
However, some of the following supplements can be useful.
Ive included links in each section to the specific supplements that I generally recommend.
Note the doses Ive recommended are for these specific supplements only.
- Vitamin D low levels of Vitamin D will pose issues for achieving a well-functioning immune system.
Recommended dose: 5,000-10,000 IUs daily, unless your blood work has shown your Vitamin D levels to be adequate.
- Bentonite Clay can help slow down intestinal motility, and bind toxins and bacteria to help you have a well formed poop.
Recommended dose: over the course of 1 week, work up to 2 tbsp daily, taken in 1 tbsp serving sizes in 12oz of water.
Take at separate times of the day away from meals.
Do not take 2 tbsp daily for more than 2 weeks.
- Probiotics / Fermented Foods can help crowd out bad bacteria and other pathogens and help to restore microbial balance in your gut.
Note for people with inflamed guts, Ive occasionally seen probiotics and fermented foods being troublesome.
This is likely due either to the acidity or to an intense Herxheimer reaction, which is why I recommend starting slow.
Probiotics recommended dose: up to 8 capsules daily, taken with or without food.
Start with 2 capsules and work your way up gradually to 8 capsules over the course of several weeks or until your symptoms improve.
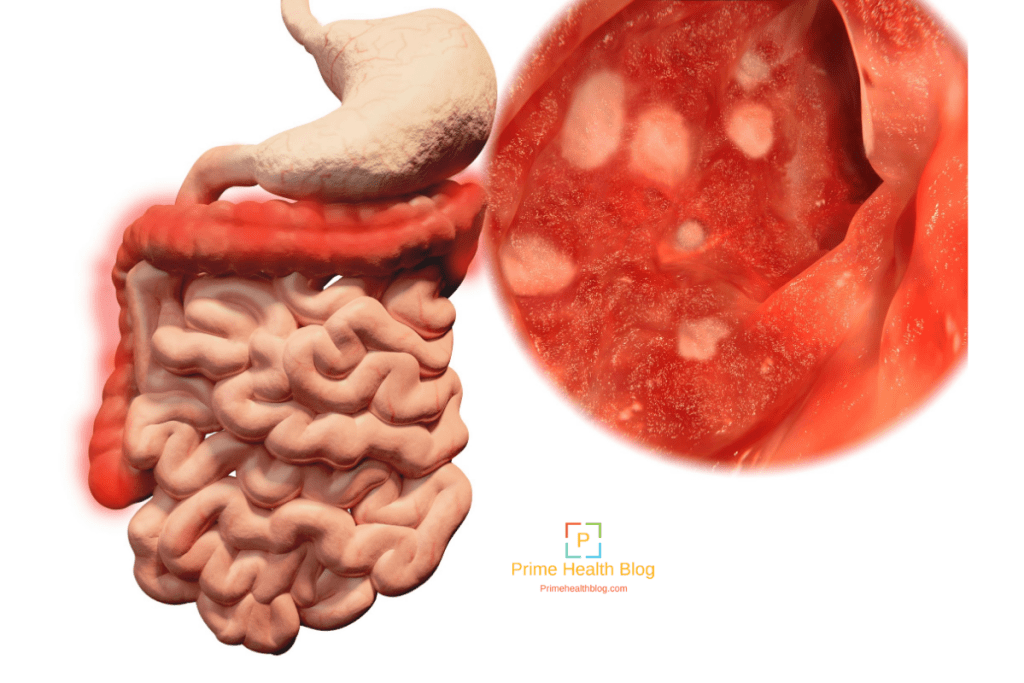
The Difference Between Ulcerative Colitis And Crohn’s Disease
Crohn’s disease is also an inflammatory bowel disease . The 2 diseases affect the digestive tract differently:
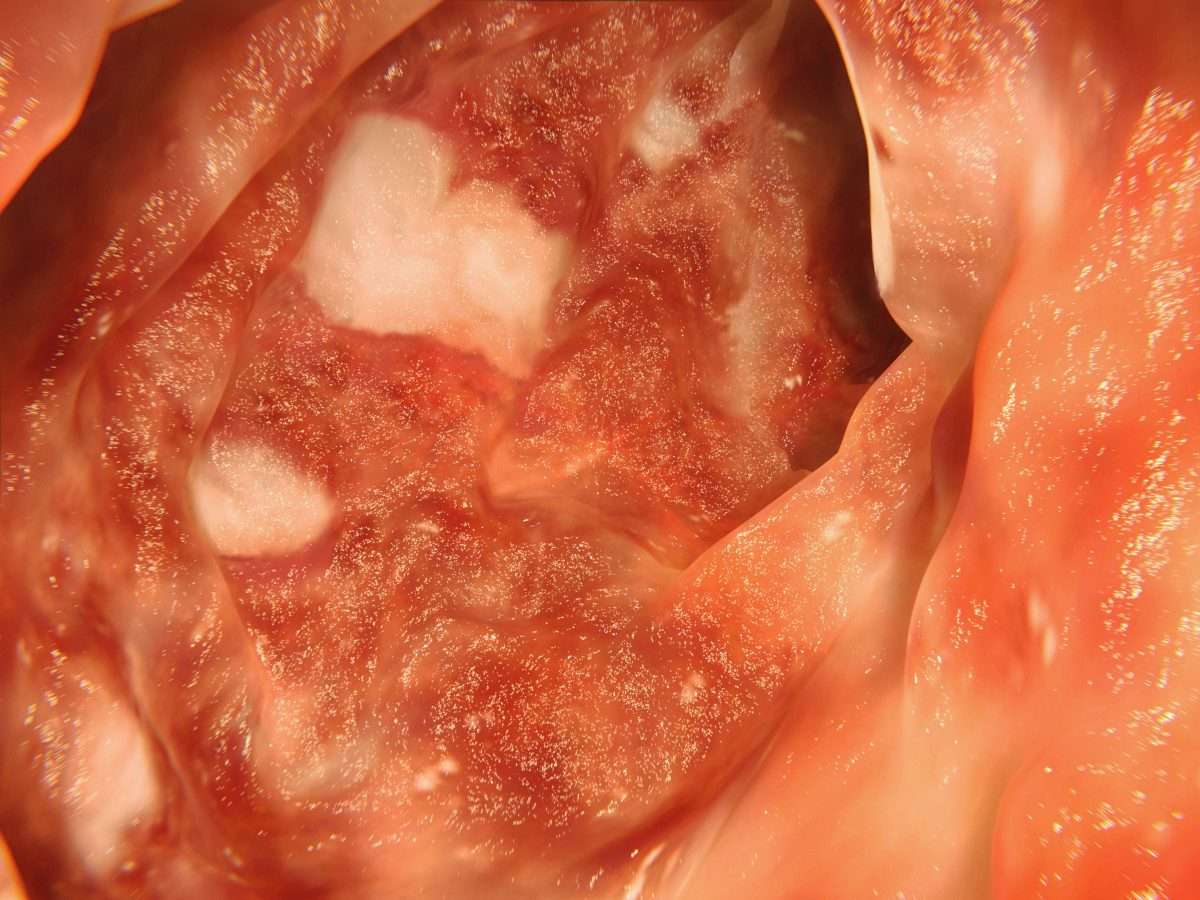
- Ulcerative colitis only affects the large bowel , and inflammation is only in the surface layers of the bowel lining. It causes ulcers to form in the lining of the bowel.
- Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus , but usually just the last section of the small bowel and/or the colon. Inflammation can extend into the entire thickness of the bowel wall.
Rectal Bleeding And Inflammatory Bowel Disease
One of the many symptoms of inflammatory bowel disease is bleeding. Blood in or on the stool can be frightening. While it can be a sign of an emergency, it’s sometimes part of an IBD flare-up.
IBD is a term for two gastrointestinal conditions with chronic inflammationulcerative colitis and Crohn’s disease. With either condition, blood might appear in or on the stool. Some people may pass no stool at all at times and just pass blood.
Bleeding from the rectum and large intestine from IBD is typically red or bright red. Blood coming from higher up in the digestive tract could appear as darker or black stools. In most cases, this bleeding is slow and steady.
This article discusses how bleeding may occur with ulcerative colitis and Crohn’s disease. It covers symptoms to watch for and how it’s usually treated.
You May Like: Good Foods To Eat With Stomach Ulcer
Visiting A Doctor For Bloody Stools
If you have rectal bleeding, you should make plans to see a healthcare provider. If you have black or extremely dark red stools, feel dizzy, collapse, or generally feel worse than normal, you should take immediate action and visit an emergency room or call an ambulance. These are signs of heavy, serious bleeding.
When you see a healthcare provider for less serious gastrointestinal bleeding, they will likely perform tests to find out what is causing the issue and to establish the right treatment. You wont know how to stop the blood in your stool until your healthcare provider gives you an accurate diagnosis.
What Is Rectal Bleeding
Although its alarming to find blood in the toilet bowl or on your toilet paper, you probably dont need to worry. Bloody stools should be addressed, but there are many reasons for rectal bleeding that dont warrant an emergency visit to the doctor.
Rectal bleeding is a blanket term that healthcare providers use to talk about any blood that leaves your body from your rectum. This doesnt mean that your rectum is the source of your bleeding the blood could be coming from anywhere in your gut. Another term for this condition is gastrointestinal tract bleeding.
Recommended Reading: Can You Eat Oatmeal With Ulcerative Colitis
Treatment By Disease Severity And Location
Mild-moderate distal colitis
- Oral aminosalicylates, topical mesalamine, or topical steroids
- Combination of oral and topical aminosalicylates is better than either alone
For refractory cases, oral steroids or IV infliximab can be used
Mild-moderate extensive colitis
- Oral sulfasalazine 4-6 g/day or alternative aminosalicylate 4.8 g/day
- Oral steroids for patients refractory to above therapy + topical therapy
- 6-MP or azathioprine for patients refractory to oral steroids, but not so severe as to require IV therapy
- Infliximab in patients who are steroid refractory/dependent on adequate doses of 6-MP/thiopurine or who are intolerant to these medications
Severe colitis
- Infliximab if urgent hospitalization is not needed
- If a patient is toxic, should be admitted to the hospital for IV steroids
- Failure to improve in 3-5 days is indication for colectomy or IV cyclosporine
Indications for Surgery
- Absolute: Hemorrhage, perforation, documented or strongly suspected cancer
Also, surgery is recommended for severe colitis refractory to medical therapy
What Causes Ulcerative Colitis
In some cases, bleeding from ulcerative colitis can lead to significant blood loss. The ultimate goal of treatment will be to calm the inflammation and stop the bleeding. Treating the loss of blood may also be necessary.
Blood loss from ulcerative colitis can cause anemia, which is a low red blood cell count. Mild cases of anemia can be treated by supplementing with iron, folic acid, and vitamin B12 to help form new blood cells. In more serious cases of blood loss, a blood transfusion to receive blood from a donor might be needed.
The most severe bleeding caused by ulcerative colitis could be life-threatening. This isn’t common, but if the bleeding can’t be stopped, surgery may be needed. This surgery involves removing the colon and creating an ileostomy, an opening in the abdomen for waste to exit.
During ileostomy surgery, the large intestine is removed. An opening, or stoma, is created so waste can pass outside the body into a bag worn on the abdomen.
Another surgery might be done at a later date to create a J-pouch. The J-pouch uses part of your small intestine to form a pouch to connect to the anal canal. This creates a way for you to pass stool the usual way, through the rectum, instead of through the stoma.
You May Like: Good Foods To Eat With An Ulcer
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
How Is It Evaluated And Diagnosed
Your health care provider will evaluate rectal bleeding by asking questions, performing a physical exam, and doing some tests.
Your provider may ask questions such as:3,4,8
- What are your bowel movements like?
- Have you had any recent changes in bowel habits?
- Are your stools black or bloody? How often does this happen?
- Have you noticed blood on the toilet paper?
- Have you vomited recently? What did it look like?
- Have you had a recent colonoscopy?
- Have you had any recent trauma to the abdomen or rectum?
- What medications are you taking?
- Do you have a history of digestive or blood diseases?
- Have you been treated for prostate or pelvic cancer?
- Has anyone in your family had colon cancer?
- Have you experienced changes in weight recently?
Your health care provider may want to look at your stool.4 If you are in the hospital, you may be asked to use a special toilet or bedpan. If you are at home, your provider will instruct you on how to collect a sample.
Also Check: Signs Of Ulcerative Colitis Flare Up
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohn’s disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Rice Water To Fight Ulcerative Colitis
One cup of rice water as soon as you wake up and another before bed will help control ulcerative colitis and its symptoms.
Ingredients
Preparing this drink is very simple.
You May Like: Foam Boots For Pressure Ulcers
Don’t Miss: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
Consult The Gastroenterologist Regularly:
During your treatment, your gastroenterologist needs to see you for regular checkups and if you have any concerns or need help to manage Ulcerative Colitis flare-up, you should consult the physician. Establish a good relationship with your doctor and be honest about your symptoms and condition as how they are affecting you because this all helps the gastroenterologist to determine an appropriate treatment plan for you or makes changes in the prescribed treatment plan.
Number : Follow An Elimination Diet & Test Each New Food
This should be where you start.
The food list should be small initially.
It should comprise no more than 3-5 foods and should also be very minimal on the supplement front.
Yes, 3-5 foods is very limited, but thats the whole point.
This is so that your immune system does not have many potential triggers to react to.
And so that as you gradually introduce foods, you can work out what your triggers are.
Pick nutrient dense foods and/or add a multi-vitamin in the beginning to avoid any nutrient deficiencies.
There are many types of elimination diet.
Some of the main ones that people will use to stop an ulcerative colitis flare up are:
- A carnivore diet
Ive used all of these with my clients with good success.
There are others, of course, but these are the main ones.
As far as which specific foods to consume, stating the obvious, I cannot be more specific without knowing the dependences listed in the section above.
That being said, for the testing:
1. Consume 1 x serving of the new food you are testing once per day for 4 days.
Only test 1 new food at a time.
Be sensible with serving sizes if you are unclear on what a sensible serving size is, eat 0.5-0.75 cups of the specific food.
You can increase the serving size over time.
The new food can be consumed with other foods that youve already tested and marked as safe.
Which foods to test and in which order is dependent on your
- dietary preferences
3. If you do not experience any symptoms, then you can continue eating the food.
Recommended Reading: Do Ulcers Make You Bloated
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
What Is Ulcerative Colitis
Colitis is a bowel disease , resulting in pain, loose bowel movements or diarrhea, loss of bowel control, and intestinal bleeding . There are over ten types of colitis, with the most common being ulcerative colitis, ischemic colitis, microscopic colitis, and infectious colitis. Causes of colitis include food allergies, infections, poor blood supply, and autoimmune reactions.
After healing myself of serious gastrointestinal disease, consulting with people with all types of colon and bowel conditions for over ten years, and answering thousands of questions on my online forum, I have become internationally recognized as an expert on natural remedies for colitis, Crohns and diverticulitis. Even if you have tried every colitis treatment available without success, dont give up hope my natural remedies for colitis have helped tens of thousands of people worldwide, and my books are sold in over 80 countries.
N.P., London, UK
My daughter had her check up with her Paediatrician yesterday he was amazed at her histology and also her Colonoscopy results. He took notes to see what I have been doing. He was so skeptical in August but was astounded at how minimal her inflammation is and he is taking everything from your book seriously he has ordered a copy of Listen To Your Gut and has asked me to give him a breakdown of everything. I will keep shouting your name from the rooftops thank you so much!
Read Also: Early Stage Venous Leg Ulcer
Limit Intake Of Animal Products
Especially meats/red meats. I have read in many articles that because many people have low stomach acidity and poor digestion, meats tend to rot in our guts, thus producing pus and contributing to inflammation . This rotting can produce more intestinal gas and overall slower digestion. I personally try to limit my meat intake to 1-2 meals per week !
Killing Off The Bad Bugs
To get rid of disease-causing bacteria, viruses, yeast, mycobacteria and parasites in your gut, use Jinis Wild Oregano Oil Protocol . If you have a mycobacterial infection, you will need to cycle on and off this wild oregano oil protocol for 2 to 3 years to get rid of all the mycobacteria as they have an inactive/active lifecycle.
People generally start with Jinis Wild Oregano Oil Protocol and then after completing the first round of treatment, move to high dose, therapeutic probiotic supplementation. Remember, they have already begun probiotic supplementation with my Wild Oregano Oil Protocol, so their system doesnt usually have much difficulty making the change to high dose probiotics.
You May Like: What Foods To Eat When You Have An Ulcer
Identifying And Healing Emotional Causes Of Colitis
Over 60% of your bodys neurotransmitters are not in your brain, but in your gut! . There is now an entire field dedicated to this emerging knowledge about the interrelation of the mind, emotions and the digestive system, called neurogastroenterology.
This is not airy-fairy stuff this is hard science. Consider blushing a purely emotional event that instantly produces a marked physical reaction. Thats just one example of how the mind/emotions and body are inextricably linked. If you dont heal the psychological and emotional causes of colitis, then you will not have long-term vibrant health. Its really that simple.
In my experience, the most effective mind/body therapies to treat colitis and other colon and bowel disorders are , hypnotherapy and craniosacral therapy . You need to work with a skilled therapist, at least initially, to really see good results. And its best if you can use a therapist who is experienced with chronic illness like ulcerative colitis which is more complex than regular illness.
What Causes Rectal Bleeding
In general, hemorrhoids and diverticular disease are the most common causes of rectal bleeding.2,5 Other common causes include:
- Angiodysplasia of the colon
- Colon inflammation from many causes
- Polyps
- Stomach ulcers
- Colorectal cancer
Bleeding in the lower digestive tract has been linked to taking non-steroidal anti-inflammatory drugs , such as Aleve, Advil, and Motrin.4 Once you have been diagnosed with IBD, NSAIDs are not recommended.6
However, research about the link between NSAIDs and IBD is ongoing and so far, inconclusive. No studies have shown that taking these medications is a cause of IBD.7
Recommended Reading: Can A Bleeding Ulcer Cause Blood In Urine
What Pain Relief Medicines Are Used In Inflammatory Bowel Disease
There are a variety of pain relief medicines available which can help to control pain in Crohns disease and ulcerative colitis.
Paracetamol
Paracetamol is a commonly used over-the-counter painkiller you can buy without a prescription. It can be used to help with mild to moderate pain, and can also help to control a high temperature. Paracetamol can be used by adults and children and is available in a variety of forms, including:
- Tablets, capsules and caplets
- Oral suspension
- Suppositories
Paracetamol works by blocking the production of chemicals in your body called prostaglandins, making your body less aware of any pain. It also reduces your temperature by acting on the part of your brain responsible for controlling it.
Paracetamol is often combined with other medicines, including other types of painkillers. Always check any additional medicines are also safe for you to use.
It is generally considered safe to take paracetamol if you have inflammatory bowel disease, however if you need to take paracetamol for longer than three days, or have a new pain, you should speak to your IBD team.
Two paracetamol tablets every four hours, up to four times a day is considered a safe dose for adults. Side effects are uncommon with paracetamol.
You should read the patient information leaflet in your medicine packet to check if paracetamol is suitable for you. Do not take more than the maximum dose in a 24 hour period as an overdose of paracetamol can be very dangerous.
Ways To Manage Symptoms And Flares Of Ulcerative Colitis
A flare of ulcerative colitis can be painful and embarrassing not only for you, but for those around you. Once you have one flare, are you going to have more? That anxiety can make you feel even worse and trigger one. Lets investigate 6 ways to manage symptoms and flares of ulcerative colitis.
Don’t Miss: Best Treatment For Diabetic Ulcers