Assessment Of Similarity Between Trials
A key assumption of indirect treatment comparison meta-analysis is that trials across comparisons are similar with respect to their designs and enrolled patient populations. The similarity of trial designs was assessed with respect to enrolment procedure, patient eligibility criteria, and outcome definitions. The similarity of patient populations was assessed with respect to the extracted baseline characteristics. These assessments were all descriptive in nature. Heterogeneity between trials within each RCT informed comparison as valid and reliable estimation is not possible with a very small number of trials .
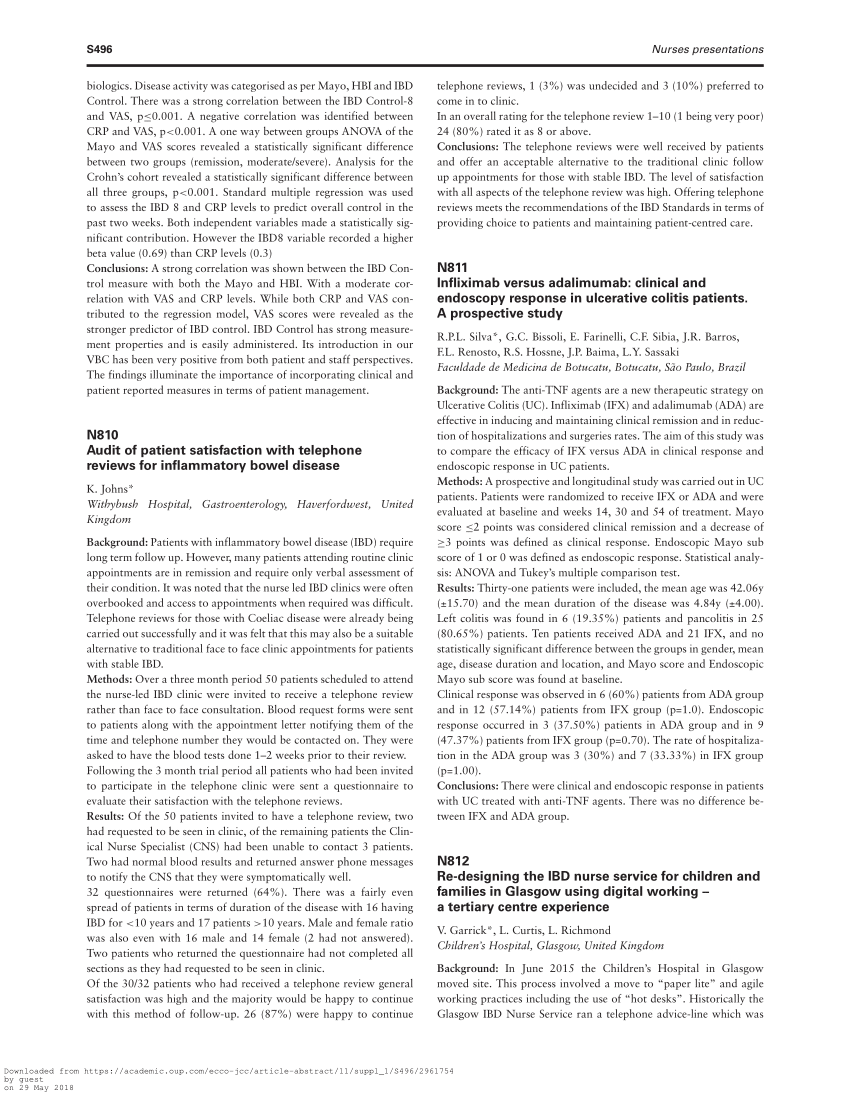
Infliximab Vs Adalimumab In Patients With Ulcerative Colitis
- Alimentary Pharmacology & Therapeutics
You’ve saved your first item
You can find your saved items on your dashboard, in the “saved” tab.
You’ve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
You’ve subscribed to your first topic alert
What does that mean?
Conditions Treated By Remicade And Humira
Remicade is approved for the treatment of:
- Moderate to severe Crohns disease in adults and children 6 years and older who have not adequately responded to conventional therapy
- Moderate to severe ulcerative colitis in adults and children 6 years and older who have not adequately responded to conventional therapy
- Rheumatoid arthritis
- Plaque psoriasis in adults with chronic, severe disease which is extensive and/or disabling
Humira is approved for the treatment of:
- Moderate to severe Crohns disease in adults and children 6 years and older who have not adequately responded to conventional therapy
- Moderate to severe ulcerative colitis in adults and children 5 years and older who have not adequately responded to conventional therapy
- Rheumatoid arthritis
- Psoriatic arthritis in adults
- Ankylosing spondylitis in adults
- Moderate to severe chronic plaque psoriasisin adults
- Juvenile idiopathic arthritis in adults and children ages 2 years and older with moderate to severely active JIA
- Hidradenitis suppurativa in moderate to severe cases in adults and children ages 12 years and older
- Uveitis in adults and children ages 2 years and older
| Condition |
| Yes |
Read Also: Foods For Acid Reflux And Ulcers
Coverage And Cost Comparison Of Remicade Vs Humira
Remicade is often billed through medical insurance or Medicare Part B as a medical cost through the location where you get the infusion, such as a doctors office, infusion center, or hospital. In some cases, Remicade may be filled at a specialty pharmacy.
Humira is often filled through a specialty pharmacy, and in some cases, it can be filled at your local pharmacy. If you fill Humira at your local pharmacy, the cost could be $6,800 or more. Using a free SingleCare card can bring the price down to about $5,600 for a box of 2 prefilled syringes.
| Remicade |
Crp Fecal Calprotectin Hemoglobin Neutrophil
A correlation between elevated C-reactive protein levels and primary and sustained response to anti-TNF drugs has also been found in CD patients for all approved anti-TNF agents . Analyses of the SONIC study have shown that elevated CRP levels were indicative of underlying inflammatory activity, thus predicting higher primary and long-term response rates than patients without inflammation . Nevertheless, not all CD patients with active disease exhibit elevated CRP-levels . In UC, higher anti-TNF induction and maintenance efficacy could be found in patients with low CRP-levels .
Fecal calprotectin measurements have established themselves as surrogate measure for inflammatory activity in IBD . However, there have so far not been any conclusive results in relation to an association between fecal calprotectin levels and response to therapy .
Higher hemoglobin levels at baseline have only been shown to be associated with short- and long-term response to anti-TNF therapy in UC , but not CD .
One study reported that a high baseline neutrophiltolymphocyte ratio predicts secondary loss of response to infliximab treatment in UC patients .
Several studies have indicated that pre-treatment albumin levels correlate with primary response to anti-TNF therapy in UC, with lower levels showing worse response . This might be due to diminished anti-TNF drug levels in hypoalbuminaemic patients .
Don’t Miss: Ulcerative Colitis And Anxiety Attacks
Warnings Of Remicade And Humira
Remicade and Humira have a black box warning, which is the strongest warning required by the FDA. The warning states:
- Because they suppress the immune system, Remicade or Humira can increase the risk of serious infections. These infections include tuberculosis , bacterial sepsis, and invasive fungal infections, and can lead to hospitalization or death.
- If a patient develops a serious infection, Remicade or Humira should be stopped.
- Before starting Remicade or Humira, a test for TB should be performed. If the test is positive, TB treatment should begin before starting Remicade or Humira. During treatment with Remicade or Humira, patients should be monitored for TB and other infections.
- Lymphoma and various other malignancies, some of which have been fatal, have occurred in children and adolescent patients treated with TNF blockers such as Remicade or Humira. Some cases of a rare type of T-cell lymphoma called hepatosplenic T-cell lymphoma have been reported in people taking TNF blockers. These cases have been aggressive and caused death. Most patients who had HSTCL were also being treated with azathioprine or mercaptopurine in addition to the TNF blocker. Most cases were in adolescent and young adult males with Crohns disease or ulcerative colitis.
Other warnings for both Remicade and Humira:
Additional Remicade warning:
Response Remission Mucosal Healing Steroid
The response, remission, mucosal healing, steroid-free, and steroid-free remission rates at week 14 are summarized in Table Table3.3. No patients had treatment failure of anti-TNF drug therapy at week 14. The response, remission, mucosal healing, steroid-free, and steroid-free remission rates at week 14 were 7 of 10 , 4 of 10 , 5 of 10 , 4 of 8 , and 2 of 8 , respectively, in the IFX group and were 11 of 15 , 6 of 15 , 7 of 15 , 8 of 12 , and 4 of 12 , respectively, in the ADA group. There were no statistical differences between IFX and ADA groups for each factor at week 14 .
Read Also: How To Test For Stomach Ulcers
Public Versus Private Drug Insurance And Outcomes Of Patients Requiring Biologic Therapies For Inflammatory Bowel Disease
Geoffrey C. Nguyen
Abstract
Background. Antitumor necrosis factor therapy is a highly effective but costly treatment for inflammatory bowel disease . Methods. We conducted a retrospective cohort study of IBD patients who were prescribed anti-TNF therapy in Ontario. We assessed if the insurance type was a predictor of timely access to anti-TNF therapy and nonroutine health utilization . Results. There were 268 patients with IBD who were prescribed anti-TNF therapy. Public drug coverage was associated with longer median wait times to first dose than private one . After adjusting for confounders, publicly insured patients were less likely to receive timely access to anti-TNF therapy compared with those privately insured . After adjustment for demographic and clinical characteristics, publicly funded subjects were more than 2-fold more likely to require hospitalization and ED visits related to IBD.. IBD patients in Ontario with public drug coverage experienced greater delays in access to anti-TNF therapy than privately insured patients and have a higher rate of hospitalizations and ED visits related to IBD.
1. Introduction
2. Methods
2.1. Patients and Design
2.2. Data Collection
2.3. Statistical Analysis
All analyses were performed with Stata version 14.0 . Categorical data were compared using the chi-square statistic. Ordinal and continuous variables with skewed distribution were compared using Wilcoxon rank sum test.
2.4. Multivariable Analysis
2.5. Ethics
3. Results
Clinical Response To Therapy
In the low titre group, 45, 31, and 234 patients had no, partial, or complete response to therapy, respectively. In the intermediate titre group, six, zero, and eight patients had no, partial, or complete response, respectively and in the high titre group, three, one, and three patients had no, partial, or complete response, respectively. The remaining patients with high titres did not have data at 1 year. The difference in the distribution of patients who showed no, partial, and complete responses was significantly different between the patients with low titres and intermediate titres , but not significantly different between patients with intermediate titres and high titres . There was a trend towards higher response rates in the patients with low titres compared with the high titres . In addition to patients who did not have a full 1 year of follow-up, 18 out of 328 patients with low titres, one out of 15 patients with intermediate titres, and three out of 10 patients with high titres were excluded from the analysis because they did not have data for their clinical response at 1 year.
Table 2: Responses to anti-TNF therapy at 1 year in patients with inflammatory bowel disease who were treated with infliximab or adalimumab between 2016 and 2019 at the University of Maryland Medical Centers Inflammatory Bowel Disease Program.Note: Patients with missing data for this outcome were excluded from analysis.
Don’t Miss: What Kind Of Yogurt Is Good For Stomach Ulcer
Can I Use Remicade Or Humira With Alcohol
Remicade and Humira do not interact with alcohol. However, alcohol can worsen many of the conditions that Remicade or Humira treat, or aggravate the side effects that they may cause. Alcohol can also interact with other medications taken for these conditions. Check with your healthcare provider regarding alcohol use.
Infliximab Versus Adalimumab Which One Is Better For Ulcerative Colitis
Corresponding AuthorEun Soo KimORCIDE-mailCopyrightComparison of Long-term Outcomes of Infliximab versus Adalimumab Treatment in Biologic-Naïve Patients with Ulcerative Colitis
Since the introduction in the mid-2000s, anti-tumor necrosis factor have been considered as paradigm-changing treatment in the management of patients with ulcerative colitis . In the pivotal clinical trials of anti-TNF agents for the management of UC, the rates of clinical remission and clinical response in anti-TNF treated group were significantly higher than in the placebo group during induction and maintenance phase. Use of these agents reduces the risk of poor clinical outcomes including hospitalization,1 cumulative corticosteroid exposure,2 and early phase surgery in patients with UC.3 In addition, they also improve health related quality of life which is an important patient-reported outcome.4
As phenotype of UC is different in various ethnic groups which may be linked to different genetic backgrounds, it is crucial to have data of specific drug efficacy in diverse populations. In line with this notion, the study by Lee et al. is clinically relevant in that it was conducted in Korea where inflammatory bowel disease incidence has been rapidly rising. The real-world study from other Asian countries is warranted to confirm the result of the current study.
Read Also: How To Soothe Mouth Ulcers
Disease Duration And Location
In patients with CD, shorter disease duration has been repeatedly described to predict higher responsiveness to anti-TNF drugs. In post hoc analyses of phase 3 clinical trials, patients with disease duration below 2 years had significantly better primary response rates to adalimumab and certolizumab pegol than those with long-standing disease. In UC, available data could not find a similar association .
Regarding disease location, differences between isolated ileal and colonic disease manifestation have been described. Post-hoc analysis of a placebo-controlled trial with certolizumab pegol showed higher probability of patients with colonic compared to isolated ileal disease to achieve clinical remission at week 6 of induction therapy . Several cohort studies also indicated better short-term and sustained clinical response to anti-TNF therapy in isolated colonic than in ileal CD . Endoscopic and histologic healing were also more frequent in colon that the ileum after 1 year of adalimumab therapy in the EXTEND trial . For UC, there was no association between disease extend and probability of therapeutic induction and maintenance response to anti-TNF treatment .
Vedolizumab Vs Adalimumab For Ulcerative Colitis
The significance of conducting future head-to-head trials of therapies used to treat inflammatory bowel disease and implications for treating ulcerative colitis with vedolizumab based on recent data demonstrated when the drug was tested in a first-ever head-to-head biologic clinical study in UC.
Stephen Hanauer, MD: One of the problems that weve had to date is that all of our drugs, for regulatory approval, are tested vs placebo. Its an efficient way of demonstrating a safe and effective drug, at least short term. But it doesnt allow us to compare agents. I mentioned the network meta-analyses before. Most recently, however, we have had a head-to-head trial in the setting of ulcerative colitis that compared vedolizumab to adalimumab. Whats your perspective of that trial and how has that impacted your practice?
Transcript Edited for Clarity
Also Check: How Can You Tell If Your Horse Has Ulcers
What Are Biologics For Ulcerative Colitis
Biologics are medications that doctors use to treat chronic inflammatory conditions such as inflammatory bowel disease . Ulcerative colitis is one type of IBD.
These laboratory-made antibodies are targeted to block specific proteins responsible for the inflammation that drives ulcerative colitis. This makes biologics different from medications such as corticosteroids, which may cause more severe side effects.
The Food and Drug Administration has approved the following biologics to treat moderate-to-severe ulcerative colitis:
- anti-tumor necrosis factor agents, including:
- infliximab
- adalimumab
The FDA approved the biosimilars of infliximab and adalimumab. As their name suggests, biosimilars are very similar to the originally approved biologics but may be more cost effective.
A person may receive biologics as an injection, as an infusion through an intravenous line, or by mouth.
The method of use, dosage, and frequency varies from one type of biologic to another.
Doctors typically prescribe an anti-TNF agent before they prescribe other types of biologics for moderate-to-severe ulcerative colitis. This is because anti-TNF medications are the most studied treatments.
Doctors may prescribe another type of biologic or a JAK inhibitor if the anti-TNF agent:
JAK inhibitors can include
Derivation Of Transition Probabilities And Costs
Transition probabilities were derived from each drug’s published RCTs and adjusted for comparison based on the assumption of a universally equivalent placebo group and a composite placebo treatment effect. Costs estimates were derived from the 2014 Medicare Physician Reimbursement Rates and Red Book wholesale prices , with drug costs calculated for an adult patient with UC at the base case weight of 70kg. outlines the probabilities and costs used in the model.
Model schematic of competing strategies. *Notes: number of weeks to 1year. ADA, adalimumab EOW, every other week IFX, infliximab VDZ, vedolizumab.
Don’t Miss: Is Oatmeal Ok To Eat With Ulcerative Colitis
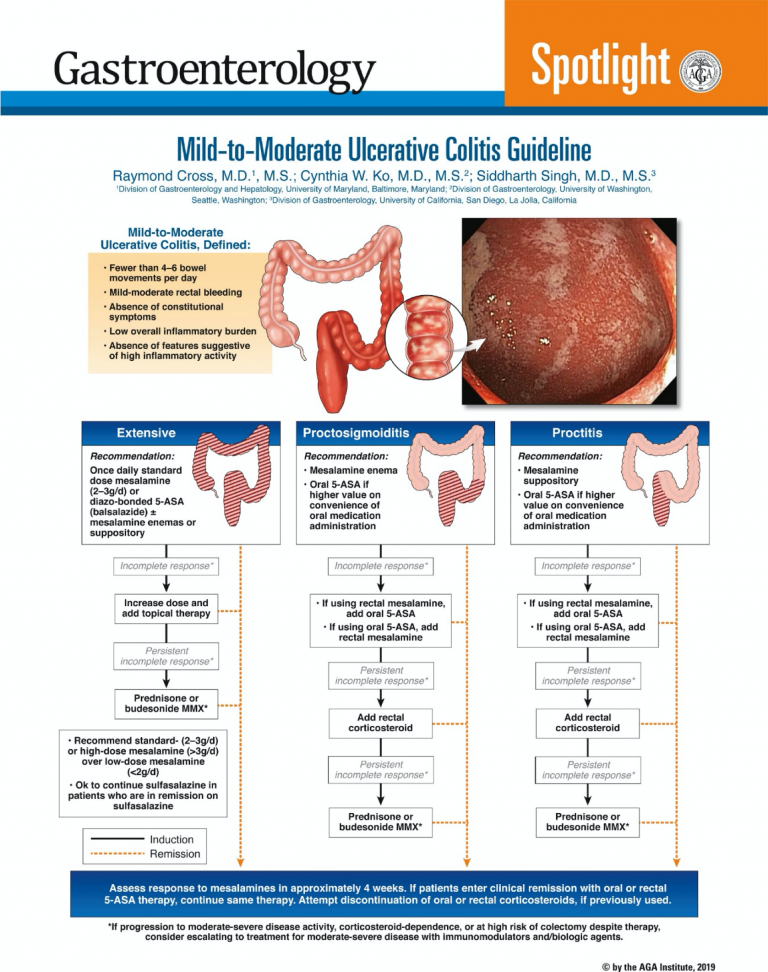
Clinical Remission And Mucosal Healing As A Primary Outcome Measure
We built a decision analytic tree in TreeAge Pro 2015 to compare the cost-effectiveness of first-line treatment with adalimumab, infliximab or vedolizumab for inducing MH at 1year in biological-naïve patients with moderate-to-severe UC. The model was based on a third party’s perspective in the USA. The primary outcome was clinical remission and MH achieved after 1year of treatment. In today’s era of biologics, achieving MH in the first year of biological treatment has become a top clinical priority in inflammatory bowel disease practice, and it is now a standard outcome measure of interest for phase 3 FDA drug trials. In keeping with the data from published randomised clinical trials for IBD biological therapies, we defined MH as a Mayo Clinic endoscopic subscore of 0 or 1.
Comparative Effectiveness Of Vedolizumab Vs Infliximab In Ulcerative Colitis
Lead Investigator: Neeraj Narula, Hamilton Health SciencesTitle of Proposal Research: Comparative Effectiveness of Vedolizumab vs. Infliximab in Ulcerative ColitisVivli Data Request: 6064Potential Conflicts of Interest: None
Summary of the Proposed Research:
Ulcerative colitis is an inflammatory bowel disease that affects the large intestine and is characterized by diarrhea, rectal bleeding, abdominal pain, urgency, and tenesmus . Patients with severe UC and/or corticosteroid-refractory disease are candidates for biologic monoclonal antibody treatments.
Vedolizumab and infliximab are two biologic therapies that have demonstrated efficacy in achieving and maintaining remission through several pivotal placebo-controlled trials, including ACT 1 , ACT 2 , and GEMINI 1 . Recently, the VARSITY trial used an active-comparator approach to demonstrate the superiority of vedolizumab to adalimumab among patients with moderate to severe UC. However, network meta-analyses have suggested superiority of infliximab over adalimumab as a first-line biologic treatment in UC patients. There are no head-to-head trials comparing vedolizumab and infliximab.
Given the routine use of vedolizumab and infliximab as a treatment for UC, head-to-head comparisons are needed to better understand the positioning of vedolizumab as a treatment for biologic-naïve UC patients.
Statistical Analysis Plan
Requested Studies:
You May Like: Is Ibs And Ulcerative Colitis The Same
Risk Of Developing High
In this study, six out of 324 patients with low titres developed high ATA/ATI titres, compared with three out of 15 patients with intermediate titres . In addition to patients who did not have a full 1 year of follow-up, four out of 328 patients with low titres were excluded from the analysis because they did not have data for the development of high-titre antibodies at 1 year.
Of the 13 patients with intermediate titres who had subsequent drug levels, five patients had their original anti-TNF dose increased in response to their initial measurement. Of these five patients, three went into remission and saw a drop in ATA/ATI titre from intermediate to low, while two showed no change or worsening of symptoms. Moreover, four of the 13 patients had their original anti-TNF dose increased and were started on an immunosuppressant in response to their initial measurement. Of these four patients, three went into remission and saw a drop in ATA/ATI titre from intermediate to low, while one showed improvement in symptoms. However, three of these 13 patients had no change to their therapy in response to their initial measurement. Of these, two went into remission and one showed no change or worsening of symptoms and saw an increase in ATA/ATI titre from intermediate to high. One of the 13 patients was switched to a different anti-TNF treatment in response to their initial measurement but was lost to follow-up.