When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Basics Of Inflammatory Bowel Disease
Arthritis means inflammation of joints. Inflammation is a body process that can result in pain, swelling, warmth, redness and stiffness. Sometimes inflammation can also affect the bowel. When it does that process is called inflammatory bowel disease . IBD is actually two separate diseases: Crohns disease and ulcerative colitis.
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.
Recommended Reading: Best Probiotic For Ulcerative Colitis
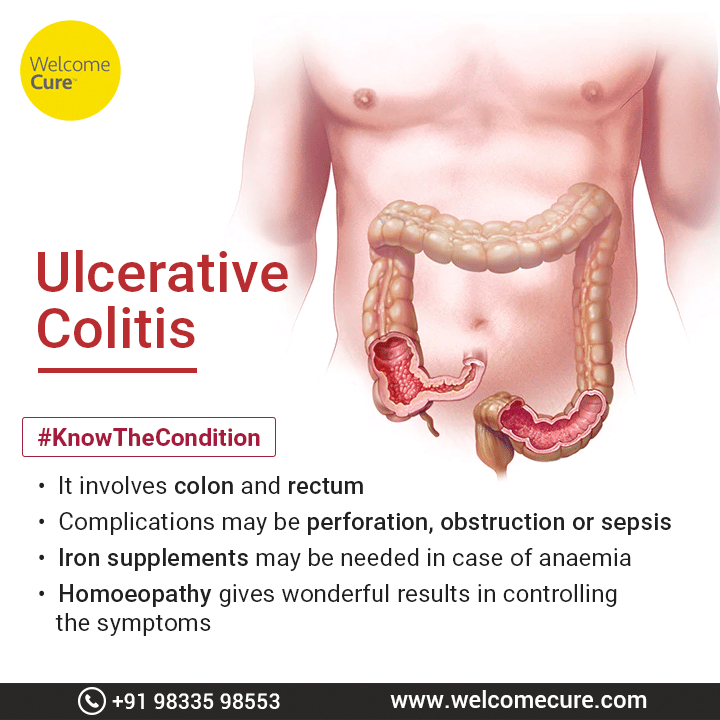
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
What Is Uc Cramping
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.
Recommended Reading: Home Remedies For Vaginal Ulcers
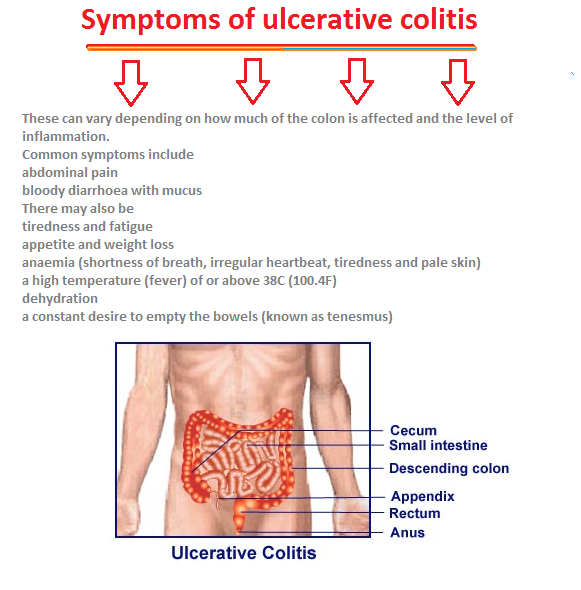
Ulcerative Colitis Symptoms You Should Never Ignore
Ulcerative colitis is an autoimmune disease in which the immune system attacks the colon and causes a range of symptoms, both in the GI tract and around the body.
Symptoms of ulcerative colitis, a type of inflammatory bowel disease , can vary widely depending on how much inflammation a person has and where the inflammation is located.
Abdominal pain and bloody diarrhea are the most common warning signs of UC, and can range from mild and intermittent to severe and chronic. The pain of UC is quite common and can significantly impact quality of life. Ulcerative colitis symptoms tend to come and go, often with extended periods of time in between flares. These are called remission periods.
The disease tends to develop gradually over time, so you might not automatically think of ulcerative colitis or IBD if you have occasional abdominal pain or digestive distress.
Ongoing inflammation along with ulcers and abscesses in the intestines are additional common causes of pain. Scarring in the lining of the intestinal tract can lead to painful obstructions. Pain may occur in different areas such as the abdomen or rectal area, depending where the inflammation is located. For example, people may experience moderate to severe pain on the left side of the abdomen if the UC affects the rectum and the lower segment of colon.
UC symptoms might ebb and flow, but they wont go away unless you see a gastroenterologist and start treatment.
What Causes Uc Cramping
Common causes of UC cramping, according to Ha, are flare-ups, lack of sufficient control of the condition , eating foods that are high in saturated fat or sugar, and adverse reactions to medication.
Cramping due to gas and bloating can also be caused by irritable bowel syndrome , a separate condition from ulcerative colitis that can cause symptoms even when your disease is in remission. IBS can be linked to certain gas-causing foods, including dairy if youre lactose intolerant.
Don’t Miss: What Are The Signs And Symptoms Of Ulcer
Tylenol And Heat Therapy
Doctors frequently prescribe nonsteroidal anti-inflammatory drugs such as ibuprofen or aspirin to help manage back pain. However, NSAIDs arent typically a viable solution for people with UC, as the medication can cause symptoms to flare.
Those with ulcerative colitis can generally take the pain reliever acetaminophen which is not an NSAID for minor aches and pains without side effects. Applying moist heat to affected areas may also reduce pain.
What Is Ankylosing Spondylitis
Ankylosing spondylitis is a type of arthritis that mainly affects the back, by causing inflammation in the spine. This can make your back, rib cage and neck stiff and painful.
It often starts in people who are in their late teens or 20s.
In response to the inflammation, the body produces extra calcium around the bones of the spine. This can make extra bits of bone grow and cause your back and neck to be more stiff.
In rare cases some of the bones of the spine may link up, or fuse together because of the extra calcium. In serious cases this can make the spine curve forward more. You can reduce the risk of this happening, if you:
Read Also: Best Foods To Eat With A Peptic Ulcer
What Are The Complications Of Ulcerative Colitis
Colon Cancer
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Skin
Other Complications
The Link Between Ulcerative Colitis And Joint Pain
UC is a type of inflammatory bowel disease . Arthritis is the most common non-GI complication of IBD. The reason for the link may lie in genes that make people with IBD more susceptible to arthritis.
Two types of conditions can affect the joints of people with UC. Arthritis is joint pain with inflammation . Arthralgia is pain in the joints without any inflammation.
Arthritis that occurs with UC is a bit different than regular arthritis. For one thing, it typically starts at a younger age.
In addition, arthritis in people with UC doesnt usually cause long-term joint damage. The joints swell up and become painful, but they return to normal once intestinal inflammation is under control.
A few types of arthritis can affect people with UC:
Read Also: Foods That Cause Stomach Ulcers
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
How Do You Know If Youre Not Receiving The Right Treatment
Anyone with a chronic condition such as ulcerative colitis should keep records of their care and closely monitor their symptoms. In particular, Bonthala recommends keeping an eye on your bowel movements, including the frequency, whether they are loose, if theres blood or mucus present, and if you suddenly experience constipation all of which could be signs that you need to change your treatment regimen.
If you suddenly develop intolerances to foods you used to stomach just fine, thats another sign that you may be undertreated.
Bonthala says your doctor should monitor your inflammation levels by testing for high levels of C-reactive protein in your blood. Your doctor can also test your stool for fecal calprotectin, a substance that your body produces when your intestines are inflamed.
You May Like: What Are The Symptoms Of Stomach Ulcers In Humans
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Also Check: What To Take For An Ulcer Over The Counter
What To Look For When You Have Ulcerative Colitis Pain
Attacks from this condition vary greatly depending on the person, so it is important to know what a flare-up is to you. It can also affected by the severity of the inflammation as well as where in the large intestine it is.
Ulcerative colitis symptoms can be anywhere from mild to severe. They can slowly build or come on suddenly without warning. It is important to monitor this condition periodically as it can get worse over time even with treatment.
Some of the most common symptoms of ulcerative colitis are:
- Blood or pus in stool
- Frequent, uncontrollable bowel movements
There are other difficulties that can happen with this chronic condition. Some of these complications include rupture of the bowel, profuse bleeding, vitamin and mineral deficiencies, severe dehydration, and inflammation of the skin, joints, and eyes. The risk of colon cancer increases as well as the possibility for blood clots in veins and arteries.
Pain As A Tool For Diagnosis
Pain can come from different sources, and pain in the abdomen is particularly difficult to pinpoint. This means that it is not a symptom that is normally used to diagnose IBD or a specific form of IBD.
Rather, the type and location of pain may be used together with other signs and symptoms. The pain serves to help a healthcare provider begin a diagnosis of IBD or other conditions. Keep in mind that it’s only a starting point.
Don’t Miss: Best Over The Counter Medicine For Ulcer Pain
Ankylosing Spondylitis And Ulcerative Colitis
When bone fusion occurs, axial spondyloarthritis progresses into ankylosing spondylitis. AS is a specific type of axial arthritis that causes inflammatory back pain and limits range of motion. If a person has AS that causes significant fusing in their vertebral column and affects their rib movement, they may also struggle to take deep breaths.
According to the University of Washington, ankylosing spondylitis symptoms generally dont present alongside gastrointestinal symptoms in people with UC. Although doctors arent entirely sure what causes AS, some research suggests a genetic component contributes to the diseases development. Bowel or urinary tract infections are also believed to trigger the onset of AS in genetically susceptible people.
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your . Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
You May Like: Do Enemas Help Ulcerative Colitis
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
How Uc Affects The Entire Body

Medically reviewed by Matthew J. Hamilton, MD
Ulcerative colitis is a type of inflammatory bowel disease, or IBD, that causes chronic inflammation in the large intestine. This can lead to gastrointestinal symptoms ranging from abdominal pain and cramping to frequent bowel movements.
However, inflammation and associated symptoms can go beyond your gutits estimated that up to 40 percent of people with IBD experience one or more non-GI symptoms.
Ulcerative colitis can be more systemic in the way it affects the body, explains David T. Rubin, MD, professor of medicine and chief of gastroenterology at the University of Chicago, and chair-elect of the national scientific advisory committee for the Crohns and Colitis Foundation. Meaning, ulcerative colitis can affect the entire body. Find out what you should watch for, plus ways to take control of your health.
You May Like: Foods To Avoid With Ulcers Mayo Clinic
When Symptoms Get Severe
In some cases, UC can in some cases cause life-threatening complications including severe bleeding, perforated colon, and severe dehydration. If any of these conditions are present, its a medical emergency and the person should get immediate medical attention. UC can also cause an increased risk of colon cancer and blood clots in the veins and arteries.
Is Pain Normal In Ulcerative Colitis
While less of a central feature than in Crohns disease, a common symptom of this condition is abdominal pain. While there may be specific triggers for the onset of this pain or stomachache, it is often resolved by a bowel movement.
It is more common for the abdominal pain in Ulcerative Colitis to be more extreme in those with a type of Colitis termed pancolitis. This is where the entire large intestine is inflamed.
If this pain becomes more acute in nature and the individual has a raised temperature testing may be required. A CT scan of the stomach/ abdomen may be used to rule out any of the complications of this disease.
Ulcerative Colitis can be classified into 3 main groups. Mild, moderate and severe. This is based on the Truelove-Witts criteria.
- Phase 1 Soft, well-cooked or cooked then pureed foods, no seeds
- Phase 2 Soft Textures: well-cooked or pureed foods, no seeds, choose floppy or tender foods
- Phase 3 May still need to avoid stems, choose floppy greens or other greens depending on individual tolerance
- Phase 4 If in remission with no strictures
Once inflamed, the gut lining becomes very sensitive. This leads to high fibre foods being too rough for the gut. This dietary approach takes this into consideration. Phase 1 is low in fibre with all foods pureed and as symptoms calm the stages are worked through, gradually relaxing and expanding the diet .
Also Check: How To Calm Down An Ulcer