What Are The Stages Of A Pressure Injury
There are four stages that describe the severity of the wound. These stages include:
- Stage 1: This stage is discolored skin. The skin appears red in those with lighter skin tones and blue/purple in those with darker skin tones. The skin does not blanch when pressed with a finger.
- Stage 2: This stage involves superficial damage of the skin. The top layer of skin is lost. It may also look like a blister. At this stage, the top layer of skin can repair itself.
- Stage 3: This stage is a deeper wound. The wound is open, extending to the fatty layer of the skin, though muscles and bone are not showing.
- Stage 4: This stage is the most severe. The wound extends down to the bone. The muscles and bone are prone to infection, which can be life-threatening.
Read Also: Ulcerative Colitis Joint Pain Treatment
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
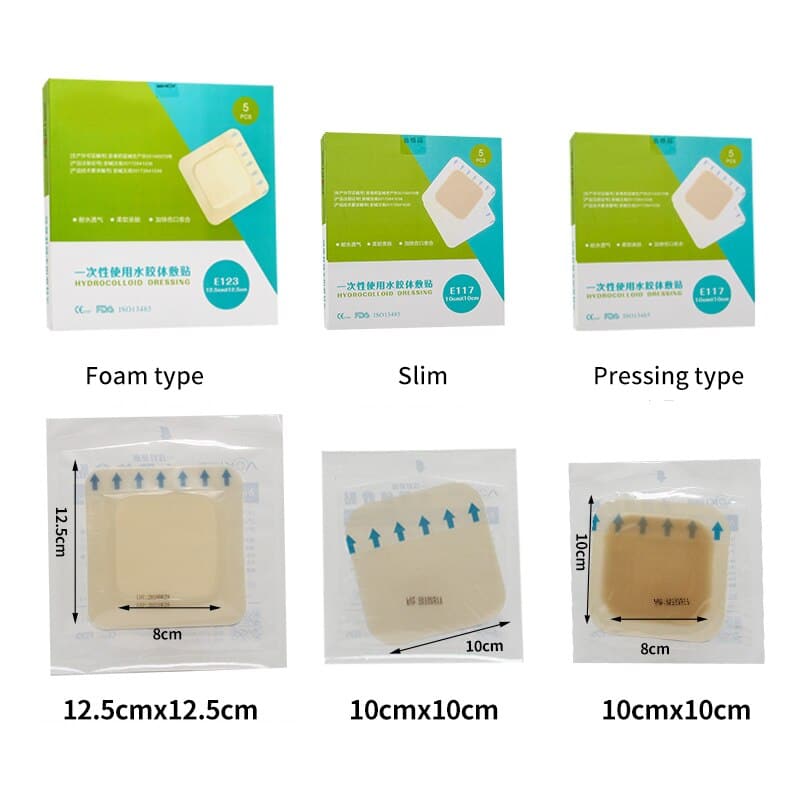
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Also Check: What Is The Medication For Ulcerative Colitis
Appendix 1 Pressure Ulcer Grading
One of the most widely recognised systems for categorising pressure ulcers is that of the National Pressure Ulcer Advisory Panel . Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury, in which wound depth and/or extent, or both, cannot be accurately determined unclassifiable pressure ulcers are generally severe and would be grouped clinically with Stage 3 or Stage 4 ulcers :
The two additional categories of unclassifiable wounds are:
- Unstageable/unclassified Obscured fullthickness skin and tissue loss: Fullthickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
Read Also: Can Ulcerative Colitis Cause Heart Problems
Cost And Quality Of Life Data
Cost and quality of life data used in the studies were also generally poor quality or lacking. When quality of life measures were reported they tended to be linear analogue scales or simple Likert-type scales. The inclusion of more sophisticated measures of quality of life when evaluating dressings is an area that needs to be tackled. This is particularly important as it may be one of the few ways to distinguish between dressings. The impact of venous ulcers on quality of life has been studied, but within randomised controlled trials quality of life data were very poor or omitted altogether.
The poor reporting of cost data was a particular concern. Where such data were collected,w7w14w29 the reporting did not conform to rigorous guidelines for economic evaluations. The trials simply totalled the monetary cost of the dressings and did not examine their cost effectiveness. This was illustrated in the hydrocolloid versus alginate comparison, where costs were reported for the interventions but insufficient detail was provided on their derivation.
Summary Of Findings For The Main Comparison

NMA evidence for individual network: proportion with complete healing interventions versus saline gauze
1Majority of evidence at high risk of bias imprecision: very wide CI .2Imprecision: very wide CI .3Majority of evidence at high risk of bias imprecision: wide CI and direct evidence on collagenase from three studies, 11 events .4Majority of evidence at high risk of bias : imprecision: wide CI and direct evidence on dextranomer from one study, seven participants and four events .5Majority of evidence at high risk of bias imprecision: wide CI .6Majority of evidence at high risk of bias inconsistency: heterogeneity in direct evidence imprecision: wide CI .7Majority of evidence at high risk of bias inconsistency: significant difference between direct and indirect estimates imprecision: very wide CI .8Imprecision: wide CI .9Majority of evidence at high risk of bias : imprecision: wide CI and direct evidence on tripeptide copper gel from one study, six participants and five events .
In this section, we present the results for the individual NMA. Results for the group network are given in Appendix 5.
Interventions and comparisons
The individual network comprised 21 interventions: 13 eligible dressings six topical agents and two supplementary linking interventions .
Risk of bias for the individual network
We report risk of bias in three ways :
Network metaanalysis results
Ranking of treatments
Rankograms for each intervention individual network
Don’t Miss: Can Ulcerative Colitis Make You Vomit
Wound Care Best Practices And The Evolving Role Of Gauze Dressings
Modern dressings are generally non-adherent and ensure appropriate healing through maintaining a moist wound healing environment and maximizing patient comfort.5 Implementing advanced dressings and alternative debridement methods as best practices for wound care will help clinicians maintain a moist healing environment.Impregnated gauze, such as gauze containing substances such as petroleum, honey, hydrogel, iodine, bismuth, and zinc, can decrease trauma and prevent desiccation during dressing changes. It can also decrease moisture loss from the wound, thereby preventing local cooling and its adverse effects.3 It has also been demonstrated that the use of advanced dressings can be more cost-effective than the use of gauze because of the massive decrease in clinician time required for the application of the dressings, even though gauze is generally a far less expensive material.2 When selecting the optimal wound dressing, it should6:
- Maintain a moist wound healing environment.
- Facilitate gas exchange.
- Protect the wound from further trauma.
- Enable easy removal and dressing change frequency.
- Be biocompatible, biodegradable, elastic, and nontoxic.
- Be cost-acceptable.
The idea of scrubbing a wound with gauze has been in practice since the 2000s and was inspired by the effectiveness of brush scrubbing for contaminated injuries. When subcutaneous scrubbing occurs in conjunction with high-pressure washing following surgery, it can be effective at lowering the risk of infection.8
Box : Comparisons Of Dressing Types
Hydrocolloids
-
Versus simple/non-adherent dressings
-
Versus other hydrogel dressings
The primary outcome measure was time to complete ulcer healing or proportion of ulcers completely healed. We excluded composite outcome measures such as ânumber of ulcers healed or improved.â
We identified randomised controlled trials by searching Medline, Embase, and CINAHL, as well as the Cochrane Wounds Group specialised trials register up to April 2006. Box 2 shows details of all the databases searched and search terms used. We also sought grey literature by examining conference proceedings. We placed no restrictions in terms of language or year of publication. We also hand searched key journals, checked citations, and contacted experts in the field of wound care to enquire about ongoing and recently published trials.
Read Also: Ulcerative Colitis Flare Up Treatment Guidelines
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
Wound Care: Pressure Ulcer Best Practices
Pressure ulcers, otherwise known as decubitus ulcers, comprise a significant portion of wounds requiring specialized care and presenting additional costs, so prevention is critically important. A pressure ulcer is any lesion caused by unrelieved pressure resulting in damage of underlying tissue. Pressure ulcers usually occur over bony prominences and are graded or staged to classify the degree of tissue damage observed. Stage 1 pressure ulcers are defined as nonblanchable erythema of intact skin the heralding lesion of skin ulceration. Stage 2 is defined as partial thickness skin loss involving epidermis and/or dermis Stage 3 as full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia and Stage 4 as full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone or supporting structures.
The Wound, Ostomy and Continence Nurses Society says that pressure ulcer prevention is best accomplished by identifying patients who are at risk for the development of pressure ulcers and initiating early preventive measures. According to the WOCN, This requires an understanding of risk factors, the utilization of research-based risk assessment tools, knowledge of appropriate preventive strategies and access to essential medical equipment such as therapeutic support surfaces.
Related Content:
Recommended Reading: Compression Stockings For Leg Ulcers
Also Check: How To Prevent Pressure Ulcers In Wheelchairs
What Causes Sacral Pressure Ulcers
Pressure ulcers occur when there is prolonged pressure to the skin, usually over bony areas such as the elbows, spine, or sacral area .
Compression of the soft tissue causes blood vessels to collapse and reduces blood flow and oxygen delivery. This localized tissue damage usually happens when a person sits or lays for long periods of time in a chair, wheelchair, or bed.
Pressure ulcers begin forming under the skin, making them difficult to catch before a wound is actually visible. So its important to take these steps to help prevent sacral pressure ulcers from happening.
Read Also: Nursing Care Plan For Pressure Ulcer Prevention
Who Is Most At Risk For Bedsores
Since the occurrence of bedsores requires prolonged pressure to a particular area of the skin, they are most common for those who remain in bed or on bedrest for an extended period of time. Typically, those with certain medical conditions that limit their ability to move or change positions are the most likely to be affected. However, bedsores can also occur when individuals spend the majority of their time in bed or even in a chair.
Unfortunately, bedsores can occur quite quickly. While there are several treatments and wound care treatment options available to address bedsores once they occur, its always best to try and prevent them from occurring in the first place. If bedrest is required or if motion is limited, try to change positions as much as possible and pay close attention to the skin and take note of any changes to its coloring or texture.
Dont Miss: Is Okra Good For Ulcerative Colitis
Read Also: Aloe Vera Enema Ulcerative Colitis
What To Do If You Have A Stage 3 Pressure Ulcer
You must seek immediate medical treatment if you have a stage 3 pressure ulcer. These sores need special attention. Your doctor may prescribe antibiotic therapy and remove any dead tissue to promote healing and to prevent or treat infection.
How long does it take for Stage 4 pressure ulcer to heal?
If you are immobilized, your doctor may recommend a special mattress or bed to relieve pressure from the affected areas. Ulcers in this stage usually need at least one to four months to heal. Stage 4 ulcers are the most serious. These sores extend below the subcutaneous fat into your deep tissues like muscle, tendons, and ligaments.
Nursing Home Abuse & Neglect Resources
Common Cases:
Client Reviews
Nursing Home Law Center, LLC is not a law firm. It is an organization that concentrates solely on helping provide nursing home patients and their families the legal help they need. NHLC LLC has a network of recognized attorneys located across the country who have experience representing clients in all types of nursing home injury cases. References to “NHLC attorneys” or “our attorneys” are references to attorneys within NHLC’s network, and not employees, agents, or partners of NHLC. Please consult the disclaimer page for further information concerning NHLC. All information on this site shall be considered ‘attorney advertising’ and not construed as legal advice. Prior case results should not be relied on when retaining a lawyer.
Read Also: How To Get Rid Of A Ulcer In The Mouth
Nma Of Treatments For Healing Pressure Ulcers
We found 51 randomized trials, and 39 could be linked to form a network joining 21 treatments in about 3000 participants . There were 13 different dressings and 6 topical agents and 2 other linking interventions .
We got results for 210 comparisons covering every pair of treatments and were also able to obtain the rank order of treatments .
To make interpretation easier, we focused on the results for the 20 comparisons with saline gauze, and the rank order of all the treatments in the network for healing.
Description Of The Intervention
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
- absorb and contain exudate without leakage or strikethrough, in order to maintain a wound that is moist but not macerated
- achieve freedom from particulate contaminants or toxic chemicals left in the wound
- provide thermal insulation, in order to maintain the optimum temperature for healing
- allow permeability to water, but not bacteria
- optimise the pH of the wound
- minimise wound infection and avoid excessive slough
- avoid wound trauma on dressing removal
- accommodate the need for frequent dressing changes
- provide pain relief and
- be comfortable.
There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.
Absorbent dressings are applied directly to the wound and may be used as secondary absorbent layers in the management of heavily exuding wounds. Examples include Primapore , Mepore and absorbent cotton gauze .
Topical agents
Read Also: Dr Reckeweg Medicine For Ulcerative Colitis
When To Use Mepilex Border Sacrum
Treatment
Use Mepilex Border Sacrum for medium-to-high exuding sacral wounds, such as pressure ulcers or surgical excision of pilonidal cysts. The dressing maintains a moist wound environment, which supports debridement, so you might see an initial increase in the wound size. This is normal and to be expected.
Pressure ulcer prevention
A recent randomised controlled trial in the USA revealed a statistically significant effect of Mepilex Border Sacrum in reducing the incidence of hospital acquired pressure ulcers by 88% You can apply the dressing prophylactically for at risk patients , such as the immobile, those with poor skin perfusion and impaired skin condition, in emergency rooms, in intensive care, or before and during long surgical interventions. Scientific studies have demonstrated that Mepilex Border Sacrum has the ability to impact on four extrinsic factors that can contribute to developing pressure ulcers: by minimising and redistributing shear, redistributing pressure, reducing friction, and maintaining an optimal microclimate .
Note: the use of dressings as part of a prophylactic therapy does not preclude the need to continue to develop and follow a comprehensive pressure ulcer prevention protocol.
Also Check: Compression Therapy For Venous Leg Ulcers
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Dont Miss: Food To Avoid For Ulcer Patient
You May Like: Turning Patients To Prevent Pressure Ulcers
Is This Guidance Up To Date
Next review: 2022
NICE medical technologies guidance addresses specific technologies notified to NICE by sponsors. The case for adoption is based on the claimed advantages of introducing the specific technology compared with current management of the condition. This case is reviewed against the evidence submitted and expert advice. If the case for adopting the technology is supported, then the technology has been found to offer advantages to patients and the NHS. The specific recommendations on individual technologies are not intended to limit use of other relevant technologies which may offer similar advantages.
This guidance replaces NICE medtech innovation briefing on Mepilex Border dressings for preventing pressure ulcers .
Your responsibility
This guidance represents the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, healthcare professionals are expected to take this guidance fully into account, and specifically any special arrangements relating to the introduction of new interventional procedures. The guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer.