Taking Care Of Yourself
Its natural that living with ulcerative colitis can make you feel stressed at times. Stress can sometimes trigger flare-ups so you may find it helpful to try some relaxation techniques. These may include deep breathing, meditation, yoga and mindfulness.
Regular exercise can also help to give you a boost and make you feel better. It can also improve your general health and help to keep your bones and muscles strong. This is important because some medicines for ulcerative colitis may affect your bone health.
Read Also: Can I Eat Oatmeal With Ulcerative Colitis
Ulcerative Colitis Treatment: Medication
The most common medication option is anti-inflammatory drugs. These can be used orally or topically to reduce inflammation of the colon and rectum.
Treating ulcerative colitis is a highly individualized process. At Johns Hopkins, we tailor your treatment to your specific needs and alter the medication as necessary. Your specific medication regimen will depend largely on the severity of your condition.
Other medications include:
-
Immunosuppressive medications: These drugs slow your immune system to stop the immune response that is causing the colon and rectum to swell.
-
Biologics: Like immunosuppressive medications, biologics target the immune system, but biologics act on specific immune system proteins that encourage inflammation.
Ulcerative Colitis Surgery Cost
As surgery for ulcerative colitis requires at least one and possibly three hospital stays, it comes at a higher cost than procedures that can be done as outpatient surgery. Ileostomy surgery may cost approximately $39,000, while j-pouch surgery may cost $50,000.
Check with your insurance provider to find out how much will be covered and what co-pays may be required. Using a hospital and surgical team in your plan’s network is key to preventing any unexpected charges.
Don’t Miss: Best Pain Relief For Leg Ulcers
What Is Surgery For Ulcerative Colitis
Surgery for ulcerative colitis means removing the large intestine, or colon . After the large intestine is gone, there needs to be another way for stool to leave the body. The two most common ways of achieving this are either by placing an ileostomy or creating a j-pouch.
In an ileostomy, a part of the small intestine is brought through the abdomen. This is called a stoma. Stool leaves the small intestine through the stoma and collects in an appliance . The ileostomy appliance is emptied into the toilet several times a day.
In an IPAA, or a j-pouch, the end of the small intestine is attached to the rectum. This is usually achieved through a series of two or three surgeries, although some surgeons will do it in a single operation. When done in more than one surgery, the first surgery is always a colectomy with placement of a temporary ileostomy.
These surgeries can be done through an open incision, or, as is more often the case now, laparoscopically . Ideally, the surgery is scheduled but is sometimes an emergency operation.
Baseline Serological Fecal And Genetic Markers
Elevated C-reactive protein, elevated fecal calprotectin, and decreased albumin levels have been associated with colectomy. Other serological markers, such as perinuclear antineutrophilic cytoplasmic and anti Saccharomyces cerevisiae antibodies have not been associated with long-term colectomy risk.
Genetic variations in HLA, MDR1 and MEKK1 have also been associated with colectomy risk in UC, but are lacking confirmation.
You May Like: What Foods Should I Avoid With A Stomach Ulcer
Recommended Reading: What Is An Ulcer In Your Mouth
Ulcerative Colitis Surgery Risks Complications
If you have any of these symptoms, get medical help right away:
- Infection or pouch inflammation . Signs: Diarrhea, frequent bowel movements, stomach cramps and pain, fever, joint pain. Treatment: Antibiotics.
- Blockage or bowel obstruction. Signs: Cramping, nausea, vomiting. Treatment: IV fluids and fasting, sometimes surgery.
- Pouch failure. Signs: Fever, swelling, pain. Treatment: Surgery and permanent ileostomy.
Scheduled And Emergency Uc Surgery
Most UC surgery can be arranged at time that’s convenient for you. Try scheduling it while your symptoms are calm to cut the chances of complications.
The risks are higher when you have emergency surgery. You may need it if you get toxic megacolon — a life-threatening condition when your colon rapidly swells and gas and bacteria build up inside. Get medical help right away if you have fever, belly pain, constipation, or swelling.
Also Check: Best Dog Food For Dogs With Stomach Ulcers
Challenge : Identifying Patients At Risk Remains A Problem In Clinical Practise
Early diagnosis of ASUC is historically based on the Truelove and Witts criteria consisting of the presence of bloody stools 6 times a day and at least one of the following signs of systemic toxicity: pulse rate > 90 bpm, temperature > 37.8, haemoglobin < 10.5 g/dl or erythrocyte sedimentation rate > 30 mm/h. Despite being 60 years old, they still remain the most sensitive criteria to define ASUC, although they must always be applied and considered in view of the circumstances and setting.7 Other indices like the clinical partial Mayo clinic score and the Montreal classification are less frequently used in clinical practise, however comparative studies for diagnosis of ASUC are not available.3,8
|
Table 1 Truelove and Witts Criteria for Acute Severe Ulcerative Colitis |
Predicting which patients are likely to fail initial treatment with corticosteroids is essential in the management of ASUC. This allows for early and multidisciplinary planning of medical and/or surgical rescue therapy.3,8 Several predictive indices have been developed but are infrequently used in clinical practise.
|
Table 2 Predictive Indices for Corticosteroid Failure in Acute Severe Ulcerative Colitis |
Lastly, plain abdominal radiography can also provide prognostic information. The presence of visible mucosal islands or a colonic diameter of > 5.5 cm predicts corticosteroid failure in 75% of patients.10 Additionally, small bowel distention conveys an increased risk for colectomy during the same admission.19
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Read Also: Safe Desserts For Ulcerative Colitis
What Types Of Surgery Can Treat Ulcerative Colitis
There are different procedures. All are major surgery on your digestive system. Talk with your doctor about which one they recommend for you.
Hemicolectomy. This is an operation that removes part of your colon. There are two types, depending on where your problem area is:
- Right hemicolectomy: Removes the right, or ascending, part of your colon. The surgeon may also take out some other areas, like your appendix and part or all of your middle large intestine. Theyll connect whats left of your colon to your small intestine.
- Left hemicolectomy: Removes the left, or descending, part of your colon. The surgeon will attach the right and middle parts to your rectum. This is the last place your bowel movements pass through on their way out.
Colectomy. This is surgery to remove the entire colon.
Proctocolectomy. This procedure removes both the colon and rectum.
Proctocolectomy is considered the standard treatment when surgery for ulcerative colitis is needed.
If the entire colon is removed, the surgeon may create an opening, or stoma, in the abdominal wall. The tip of the lower small intestine is brought through the stoma. An external bag, or pouch, is attached to the stoma. This is called a permanent ileostomy. Stools pass through this opening and collect in the pouch. The pouch must be worn at all times.
Time Trends In Colectomy Rates:
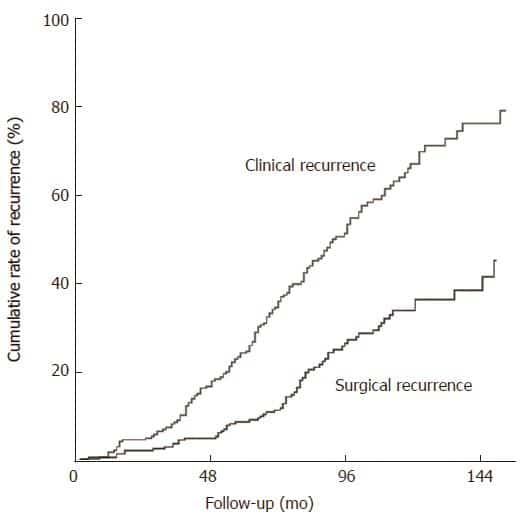
We observed a decrease in colectomy rates over time, with evident nominal decrease in absolute numbers of annual colectomies performed after 2010 . In an unadjusted crude prediction of yearly colectomy rates, we found a significantly decreasing linear trend already after 2005 . For this entire period of time, when adjusting for disease duration, age at diagnosis, gender, and previous use of anti-TNF, a statistically highly significant linear diminishing trend with year on the logistic level for colectomy rates was found . Importantly, by far the lowest colectomy rates observed in our follow-up time were detected in the last 3 years of observation, i.e. 20132015. The observed survival rate without colectomy, analysed in a time-to-event fashion and stratified by patients diagnosed before and after 2003 , indicated that colectomy was performed significantly earlier during the individual course of disease in recently diagnosed patients . Cumulative proportions of colectomy at 2, 5, or 10 years after diagnosis were roughly twice as high in the more recently diagnosed subgroup of cohort patients, with 2.50%, 5.96%, and 8.64% versus 1.09%, 2.65%, and 4.71% in patients diagnosed after and before 2003, respectively.
Predicted and observed incidence rates of colectomy over 20052015. The observed incidence rate of colectomy over time is depicted in conjunction with a crude, unadjusted predicted yearly rate .
Recommended Reading: What To Eat With An Ulcerative Colitis Flare Up
Elective Surgical Management Of Ulcerative Colitis
Surgical options for elective management of ulcerative colitis include total proctocolectomy with creation of an end ileostomy, total proctocolectomy with continent ileostomy, total proctocolectomy with IPAA, and total abdominal colectomy with ileorectal anastomosis. Among these, a creation of an IPAA is currently considered the preferred standard of care. Patients who are not suitable candidates for IPAA can be treated with laparoscopic total proctocolectomy and end ileostomy. On the other hand, laparoscopic surgery in the creation of an ileorectal anastomosis following total abdominal colectomy is technically feasible, but is rarely indicated. Similarly, total proctocolectomy and creation of a continent ileostomy is generally performed on patients who had previous surgical procedures for ulcerative colitis and is therefore typically performed using open technique. Ileorectal anastomosis and continent ileostomy will therefore not be further discussed in this review.
What Can Be Expected After Ileal Pouch Surgery
In most cases after ileal pouch surgery, quality of life improves over time. Patients can usually resume normal work and activities about 4-8 weeks after surgery. What ulcerative colitis patients like most about having any kind of pouch is that they no longer have the severe urgency or need to run to the bathroom.
After ileal pouch surgery, the patient must have an examination of the inside of the pouch with an instrument called an endoscope every year or every other year for the rest of his or her life to watch for the development of precancerous cells. In addition, all types of pouches can develop pouchitis, an irritation and inflammation of the inner lining of the pouch. Pouchitis is very common, but usually responds to oral antibiotics within 24 hours.
Overall, the long-term success rate of the pouch procedure is approximately 95%. However, there is a 5-10% chance of failure after pouch surgery. Most failures are due to the wrong diagnosis , persistent severe pouchitis, or complications of surgery.
In some cases, the pouch may need to be repaired or removed and replaced with a new pouch. Another option is to convert the pouch to a permanent ileostomy .
You May Like: L Glutamine Ulcerative Colitis Dosage
Recommended Reading: Best Meds For Ulcerative Colitis
What You Should Know About J
-
This surgical procedure can be performed in up to three stages, but is usually done in two.
-
A temporary ileostomy is typically created to give your newly formed pouch a chance to heal. A loop of your small intestine will be pulled through an opening in your abdomen, called a stoma, to allow waste to exit your body into an ostomy bag.
-
During this time, you will need to wear an ostomy bag at all times and it will need to be emptied several times a day.
-
You will have your second surgery eight to 12 weeks later, once the pouch has healed.
-
A three-stage procedure may be recommended for patients who are in poor physical health, on high doses of steroids, or if they are required to undergo emergency surgery to repair bleeding or toxic megacolon.
Are There Any Risks Or Complications To Be Aware Of
Despite the potential benefits, the J-pouch procedure is still considered major surgery. As with any major surgery, you may be at risk for infections, bleeding, and side effects from general anesthesia.
Sometimes its possible for the newly formed J-pouch to become infected. However, such risks are higher in one-stage procedures.
Other potential complications from this procedure include:
Overall, the outlook for J-pouch surgery is positive, with few people experiencing pouch failure.
However, one study published in 2015 reported a J-pouch failure rate of between 3.5 and 15 percent. Pouch failures have also been found to be more common in men than women.
If you do develop pouch failure, your doctor may recommend either an ostomy or another type of colorectal procedure called a K-pouch surgery.
Pouchitis is the most common problem following J-pouch surgery and other pouch surgeries. This is a treatable condition and does not necessarily mean youll develop pouch failure. However, chronic pouchitis has been linked to possible failure of the J-pouch.
Recommended Reading: What Foods To Avoid With Peptic Ulcer
Purpose Of Ileostomy Or J
Surgery is used to treat ulcerative colitis for a few different reasons.
The first reason to have a colectomy for ulcerative colitis is that the condition is no longer treatable with medications. There are many different drugs that are used to treat the condition. However,the available drugs may not significantly reduce inflammation.
Some of the medications used to treat ulcerative colitis may need time to work to get the disease under control. It can also occur that the disease becomes severe enough that theres not enough time for the drugs to work.
While not common, ulcerative colitis is also associated with colon cancer. The risk of colon cancer increases after having the disease for about eight to 10 years. If there are changes in the colon that might lead to colon cancer, surgery to remove the colon might be the best option.
Surgery might also be done to treat complications. Two of those include toxic megacolon and a perforation in the intestine. These are rare emergencies, but they would be a reason for a colectomy surgery.
Another reason to have surgery for ulcerative colitis is to improve quality of life. A patient might decide that the symptoms of the disease are keeping them from living a full, happy life, and surgery offers an opportunity for improvement.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Recommended Reading: Is Oatmeal Good For Ulcerative Colitis
Don’t Miss: What Can You Do For An Ulcer In Your Stomach
Surgery For Ulcerative Colitis: Before And After
Many people with ulcerative colitis end up needing surgery, sometimes sooner rather than later. Heres what to expect if youre considering or preparing for surgery.
When medications fail to manage symptoms of ulcerative colitis, you may need surgery. In fact, a surgical procedure is currently the only method that can cure someone of this condition.
Ulcerative colitis is an inflammatory disease that affects your colon and rectum, and treatment usually begins with medications to control inflammation and other symptoms. However, 23 percent to 45 percent of people with ulcerative colitis will need surgery.
New drugs are starting to reduce the number of people who need surgery, but when drugs cant control ulcerative colitis symptoms, surgery can be a solution, says Thomas Ullman, MD, an associate professor of gastroenterology at the Icahn School of Medicine at Mount Sinai Hospital in New York City.
But when is surgery the best choice for ulcerative colitis? For some people, surgery could be necessary sooner rather than later possibly even during a first attack, especially with the onset of sudden and severe symptoms. If an ulcerative colitis flare causes serious symptoms such as severe bleeding or a rapid enlargement of the colon called toxic megacolon, emergency surgery may be required. About 15 percent of people with ulcerative colitis may experience this type of flare.
Surgery Can Truly Help
While surgery is always a major step and not without risks and complications, UC is principally surgically curable when the large intestine is removed because its limited to the colon and rectum, according to a study in Viszeralmedizin. While chronic pouchitis is one of the main factors limiting surgical success in curing UC, theres still a long-term pouch success rate of > 90%, 10 and 20 years later, researchers found. For most patients, when they get the surgery, there is actually a sense of relief, says Dr. Bedford. No more bloody stools. And typically no more abdominal pain and steroids.
Don’t Miss: Alternative Medicine For Ulcerative Colitis
How To Take Tablets And Granules
You will either take the tablets or granules once a day, or as 2 or 3 smaller doses throughout the day.
Swallow the tablets whole with a drink of water or juice. Do not break, chew or crush them. This is because some tablets have a special coating to delay when they start to work, or to protect the medicine from the acids in your stomach.
For granules, open the sachet and tip the granules onto your tongue. Swallow them whole with a drink of water or juice. Do not chew them, as some granules have a special coating.
You can take some brands with food. Check the leaflet that comes with your medicine.
If youre also taking indigestion medicines or remedies, leave a 2 hour gap before and after taking mesalazine. Indigestion treatments can affect how well the medicine works.