Prognosis Of Helicobacter Pylori
The natural history of idiopathic ulcers is poorly documented because of the rarity, but it seems that H. pylori-negative ulcers are characterized by a longer duration of initial ulcers, a higher number of ulcers in the duodenum, more ulcer recurrences and more severe dyspepsia compared with H. pylori-positive ulcers., , , Helicobacter pylori-negative ulcers may have an aggressive clinical course, are more susceptible to complications and are more refractory to treatment., , , , As an example, McColl et al. showed that these H. pylori-negative ulcer patients had longstanding recurrent dyspepsia, four patients failed to heal their ulcers despite 3months on H2-receptor antagonists, two were subsequently treated with omeprazole and one required highly selective vagotomy. In addition, two patients had ulcer bleeding, requiring transfusion. Furthermore, bleeding occurred in one patient despite maintenance H2-receptor antagonist therapy. Chu et al. assessed the clinical characteristics of DU patients depending on the H. pylori status and found that in terms of clinical manifestation, patients with H. pylori-negative DU were more likely to present with bleeding. Finally, Bytzer et al. demonstrated that H. pylori-negative DUs were associated with a poorer prognosis mainly because of a higher rate of ulcer and symptom relapse thus, the main reasons for the poorer prognosis in H. pylori-negative patients were ulcer, not healed or relapse of ulcer.
Time Trends Of Helicobacter Pylori
Some studies have evaluated the time trends of H. pylori prevalence in patients with DU disease and have concluded that the prevalence of H. pylori-negative ulcer or idiopathic peptic ulcer is increasing with time. As an example, Konturek et al. published in 2003 that the prevalence of H. pylori infection in DU patients had decreased during the 5-year of follow-up while, at the same time, the ratio of idiopathic ulcers to total number of ulcers had risen. This same year , in Peru, Ramirez-Ramos et al. determined the changes in the prevalence of H. pylori in DU patients from 1985 to 2002 and confirmed a decrease from 90% to 72%. Later, in 2005, Chu et al. reported that the annual proportion of patients with H. pylori-negative DUs had increased progressively from 1996 to 2002. More recently, in 2008, Jang et al. investigated the changing trend of idiopathic peptic ulcer disease and the prevalence of H. pylori infection during the last decade and found that the proportion of DU had significantly decreased compared with 10years ago most importantly, they also found a changing trend in the prevalence of H. pylori infection in DU: a decrease from 79% to 68%.
However, a limitation of these evolution in time studies is that comparing results from several years ago may be inappropriate, as the prevalence of H. pylori infection depends on several factors which might have changed during this lapse of time.
Covariates Associated With Cu
According to results of univariable analysis , female sex, comorbid allergic rhinitis, asthma, renal disease, diabetes, rheumatic disease, malignant tumor, and atopic dermatitis appeared to be associated with increased risk of CU, but all the associations were not statistically significant .
|
Table 2 Univariable Analysis of Covariates Associated with Chronic Urticaria |
Don’t Miss: Best Medicine For Stomach Ulcer Pain
Isolated Helicobacter Pylori Duodenal Colonization
A recent study has suggested that in some patients with DU, the infection is confined to the duodenal mucosa and eradicating it cures the ulcer disease. In fact, according to the accepted model for the development of DU, duodenal colonization is the last step in this process. However, as H. pylori search in the duodenum is not usually performed, if the organism disappears from the stomach, but still colonizes the duodenum and causes an ulcer, this will be erroneously classified as idiopathic . In the study by Pietroiusti et al., 7% of the 608 DU patients evaluated were classified as idiopathic however, a substantial proportion of DU patients who were classified as H. pylori-negative on the basis of the findings of gastric biopsies carried the organism in the duodenum, and H. pylori eradication treatment induced persistent healing of the ulcer in the vast majority of them. In contrast, the same antibiotic therapy was ineffective in those patients testing negative for the presence of the organism in both gastric and duodenal biopsies. Given the very low incidence of isolated duodenal H. pylori colonization among DU patients , systematic testing of duodenal biopsies would be rather impractical. However, in patients with DU and no evidence of H. pylori in the stomach, taking biopsies from the duodenum may be considered.
How Is H Pylori Treated
If you dont have symptoms, you dont need to be treated. If youve been diagnosed with H. pylori, avoid taking nonsteroidal anti-inflammatory drugs. These drugs can increase your risk of developing an ulcer.
H. pylori-caused ulcers are treated with a combination of antibiotics and an acid-reducing proton pump inhibitor.
- Antibiotics: Usually two antibiotics are prescribed. Among the common choices are amoxicillin, clarithromycin , metronidazole and tetracycline.
- Proton pump inhibitor: Commonly used proton pump inhibitors include lansoprazole , omeprazole , pantoprazole , rabeprazole or esomeprazole .
- Bismuth subsalicylate: Sometimes this drug is added to the antibiotics plus proton pump inhibitor combinations mentioned above. This drug protects the stomach lining.
Combination treatment is usually taken for 14 days.
One newer medication, Talicia®, combines two antibiotics with a proton pump inhibitor into a single capsule.
Also Check: Mouth Ulcers Treatment Home Remedies
Characteristics Of The Study Participants
We included 40 patients with PUD as the PUD cohort and 80 patients without PUD as the control cohort . The mean age of the PUD cohort was 53.40±18.78 years, which was similar in the control cohort . There were no significant differences in other patient characteristics, including age, sex, and several comorbidities .
|
Table 1 Characteristics of the Study Participants |
Is Empirical Helicobacter Pylori Eradication Therapy In Duodenal Ulcer Patients Advisable
Some authors have suggested that as DU is almost always associated with H. pylori infection, a practical policy, once a DU is diagnosed, may be administering H. pylori eradication therapy without confirmation of the infection., – In this way, it has been emphasized that routine testing for H. pylori is very expensive: the charge for documenting the infection by endoscopic biopsy in all patients with DUs is almost 10 times that of empirical H. pylori therapy. Furthermore, it has been suggested that biopsy results do not provide clinically useful information in most patients with DU and may be misleading if falsely negative. Obviously, empirical eradication therapy without H. pylori testing may be reasonable only when the prevalence of H. pylori infection is high and when there is no history of NSAID use., ,
A further argument supporting this simplified strategy is that, as some authors have pointed out, a negative test result may not confidently exclude infection., For example, if 95% of DU patients are actually infected and if the sensitivity and the specificity of diagnostic tests are 95%, the negative predictive value will be only 50%. When performing methods having a lower than 95% sensitivity, the predictive value of a negative test will be even lower than 50%. On the other hand, if the prevalence of H. pylori were as high as 99% , a negative diagnostic result would have a negative predictive value as low as 15%.
You May Like: Hospital Acquired Pressure Ulcer Statistics Cdc
Management Of H Pylorinegative Patients
Figure shows a hypothetical algorithm for the management of uninvestigated dyspepsia. Factors other than H pylori status should initially guide clinical decisions. Patients with late onset of symptoms and/or associated alarm features should be investigated immediately. The remainder, with a low probability of having an organic disease, should be treated symptomatically. In those who fail to respond or have frequent relapses, H pylori testing followed by eradication in infected cases may be considered. If patients do not think that a serious diseasefor example, cancer, is the cause of their symptoms, non-invasive diagnostic tests should performed.
Management of uninvestigated dyspepsia. Short courses of medical treatment tailored to the predominant symptom should be prescribed initially. H pylori investigation and treatment of infected individuals should be considered for non-responders or in the case of frequent recurrences. UBT, urea breath test.
Three different types of H pylori negative dyspeptic patients can therefore be encounteredin clinical practice:
-
dyspeptic patients with no evidence ofH pylori infection on non-invasive testing
-
dyspeptic patients with no evidence ofH pylori infection at endoscopy and
-
dyspeptic patients with no evidence ofH pylori infection after successful eradication.
Diagnostic Strategy In Helicobacter Pylori
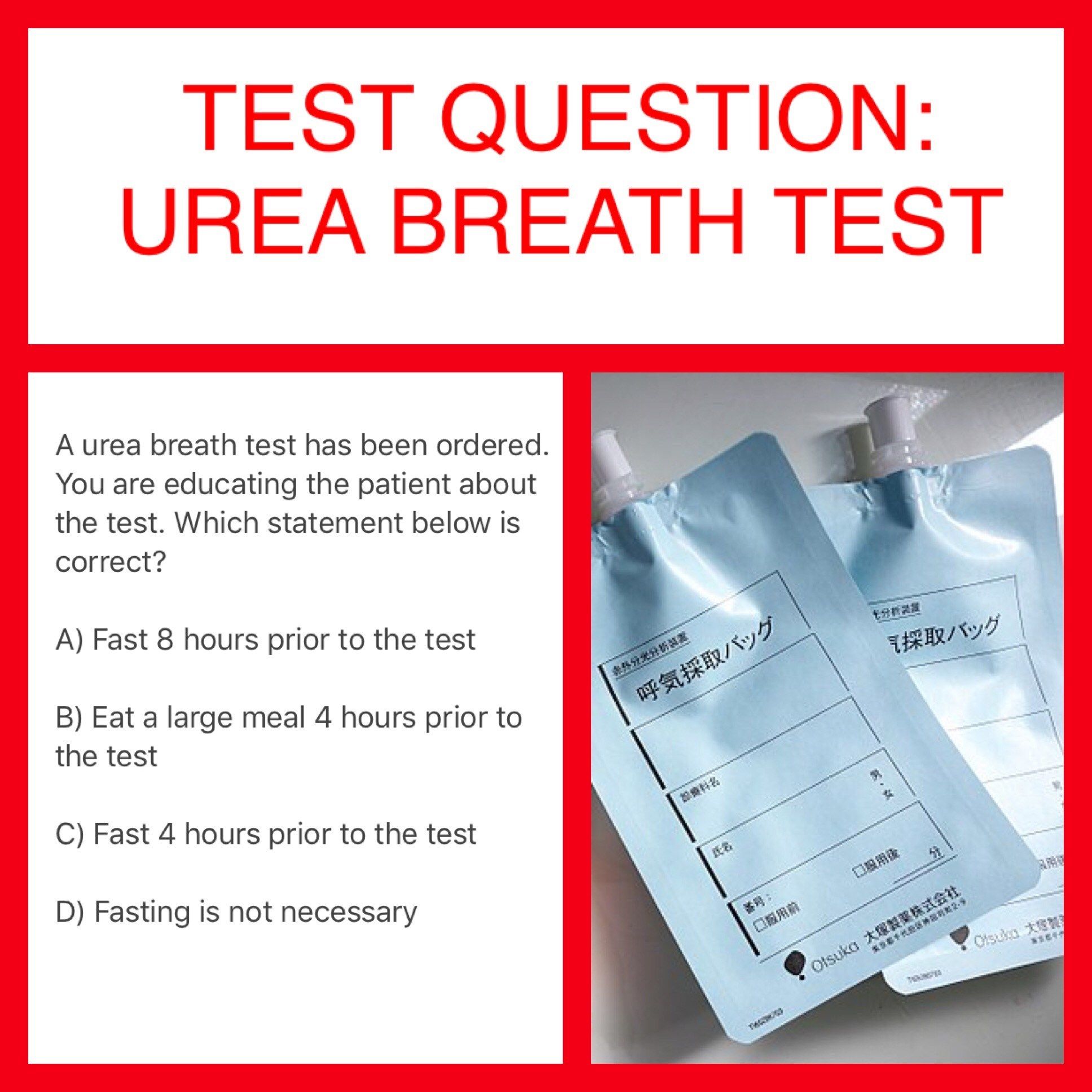
As reviewed, there may be several causes of H. pylori-negative DUs . Accordingly, the first and most important action on encountering a patient with unexplained DU is to double check that he/she is truly H. pylori-negative, trying to rule out false negatives of H. pylori diagnostic methods. This may be done by using more than one H. pylori diagnostic test, by taking biopsies from several gastric sites and by testing H. pylori after stopping PPIs and antibiotic treatments. If biopsy-based tests are negative, consider performing non-invasive tests, such as C-urea breath test or serology. DU patients truly H. pylori-negative, the second most important step would be to exclude NSAID use. If this risk factor is not easily recognized by the patient, the unrecognized or surreptitious NSAID use should be intentionally and carefully searched and the measurement of serum and urine salicylate levels may be considered. If surreptitious NSAID use is ruled out , biopsies from the duodenum should be obtained to discard isolated H. pylori duodenal colonization and also diseases of the duodenal mucosa . If the aetiology of the ulceration remains unexplained, serum gastrin levels should be measured to rule out ZollingerEllison syndrome. Obviously, a careful clinical history should always be obtained and the habits and the concomitant diseases of the patient determined. The recommended diagnostic strategy for the patient with H. pylori-negative DU is summarized in .
Helicobacter pylori
Recommended Reading: Natural Remedies To Heal Stomach Ulcers
How Is H Pylori Infection Treated
H. pylori bacteria can be treated by taking 2 antibiotics and another type of medicine called a proton pump inhibitor . The antibiotics kill the bacteria and the PPIs reduce your stomach acid so the antibiotics can work well. This combination of medicines is often called eradication therapy.
- Antibiotics used to clear H. pylori areclarithromycin and either amoxicillin or metronidazole.
- Proton pump inhibitors are omeprazole, lansoprazole and pantoprazole.
You will need to take eradication therapy for 14 days. It is important to take all the medication exactly as directed and to finish the course. Eradication therapy clears H. pylori for 9 out of 10 people if it is taken correctly for the full course. If you dont take the full course of medication, then it will not work so well. A second course of eradication therapy, using different antibiotics, will usually work if the first course hasnt cleared the infection. Smoking reduces the chance of successful treatment, so it is very important to stop smoking.
Dont Miss: How Do Doctors Test For Ulcerative Colitis
The Benefits You Will Get After H Pylori Treatment
In 1994, The NIH consensus conference recognized H. pylori as a cause of gastric and duodenal ulcers. In the same year, International Agency for Research on Cancer Identified H. pylori as a risk factor for gastric adenocarcinoma .
Later on, h. pylori have been identified as a risk factor for a variety of diseases.
After successful treatment of H. pylori, you should expect:
- Improvement in chronic gastritis.
- Healing of gastric or duodenal h. pylori-induced ulcers.
- Lower risk of gastric cancer.
- Your risk of getting gastric MALT lymphoma will be lower. MALT lymphoma is a type of gastric lymphoma that is strongly associated with h. pylori).
- In people who already have MALT lymphoma, H. pylori treatment helps the resolution of the disease.
- h. pylori treatment may lead to improvement in some diseases beyond your gut. Examples are iron deficiency anemia, immune thrombocytopenic purpura , coronary artery disease, asthma, insulin resistance, chronic urticaria, and others .
Also Check: What Are The Signs Of A Bleeding Stomach Ulcer
What Can I Do To Prevent H Pylori
Health experts dont know for sure how the bacteria passes from person to person. But having good health habits can help keep you safe. These habits include:
-
Washing your hands with soap and water. It is very important to do this after using the bathroom and before eating.
-
Making sure all food you eat has been cleaned and cooked safely
-
Making sure that your drinking water is safe and clean
Read Also: Black Tarry Stools Ulcerative Colitis
History Of Peptic Ulcer
It might be possible that new ulcer patients are different from those who had already been diagnosed years before. Patients with a short history of DU are more likely to be H. pylori-negative than those with a longer history.- As an example, some authors have assessed the presence of H. pylori in patients undergoing endoscopy for dyspepsia with respect to the duration of their symptoms. Patients were categorized as having a history longer or shorter than 6months. Thirty-two DU patients with a history > 6months were all H. pylori-positive however, the five with a shorter history were H. pylori-negative.
Recommended Reading: Suggested Diet For Ulcerative Colitis
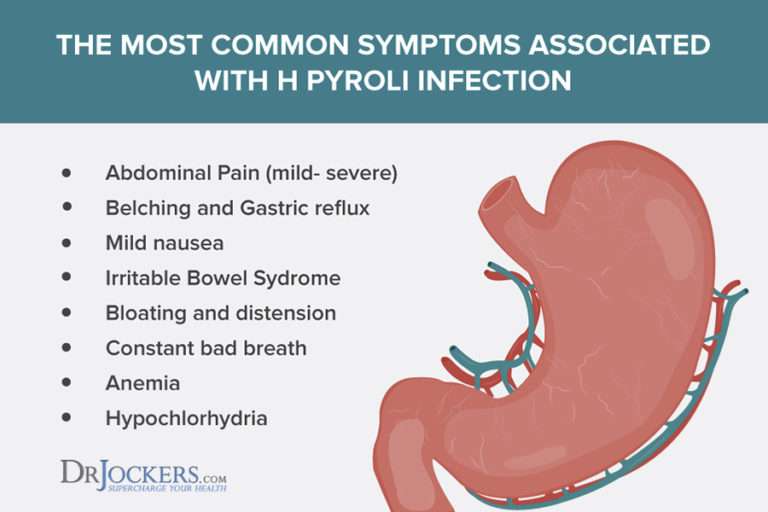
What Are The Complications Of H Pylori Infections
H. pylori infections can lead to peptic ulcers, but the infection or the ulcer itself can lead to more serious complications. These include:
- internal bleeding, which can happen when a peptic ulcer breaks through your blood vessel and is associated with iron deficiency anemia
- obstruction, which can happen when something like a tumor blocks the food from leaving your stomach
- perforation, which can happen when an ulcer breaks through your stomach wall
- peritonitis, which is an infection of the peritoneum, or the lining of the abdominal cavity
H. pylori can also increase the risk of gastric adenocarcinoma, a type of stomach cancer. This risk is higher among smokers, as well as Black people/African Americans, Latinos and Hispanics, and Asians, according to a large 2019 cohort study.
With that said, most people infected with H. pylori never develop stomach cancer.
Stool Monoclonal Antigen Tests
Stool antigen tests using monoclonal antibodies are as accurate as urea breath tests if a validated laboratory-based monoclonal test is used.1,11 They are cheaper and require less equipment than urea breath tests. Like urea breath tests, stool antigen tests detect only active infection and can be used as a test of cure. PPIs should be stopped for two weeks before testing, but stool antigen tests are not as affected by PPI use as are urea breath tests.
You May Like: What Does A Stomach Ulcer Feel Like
How Are H Pylori Infections Treated
If you have an H. pylori infection that isnt causing you any problems and you arent at increased risk of stomach cancer, treatment may not offer any benefits.
Stomach cancer, along with duodenal and stomach ulcers, is associated with H. pylori infection. If you have close relatives with stomach cancer or a problem like a stomach or duodenal ulcer, a healthcare professional may recommend treating an H. pylori infection.
Treatment can cure an ulcer, and it may reduce your risk of developing stomach cancer.
Recommended Reading: Ulcerative Colitis Versus Crohns Disease
The Next Step After The H Pylori Treatment Course
After you complete the 7-14 day course of h. pylori treatment, your doctor usually prescribes a proton pump inhibitor for another 4-8 weeks.
In small uncomplicated h. pylori ulcers, The 14-day treatment course can be sufficient if your symptoms have improved. However, if symptoms persist, Your doctor may prescribe a PPI .
In large or complicated ulcers , your doctor may prescribe the PPIs for up to 12 weeks .
After the period of PPI therapy, Your doctor may re-test for h. pylori to confirm its eradication.
Treatment resistance rates are high nowadays. Re-testing is becoming a routine of practice because of the resistance.
Recommended Reading: Diet For People With Ulcers
When And How Your Doctor Will Confirm The Eradication
Your doctor will confirm the eradication fro H. pylori after at least four weeks after the end of the treatment course .
Your doctor will confirm the eradication using one of:
It is vital to stop PPIs one or two weeks before the test. PPI may affect the results of h. pylori eradication .
Also, h. pylori blood tests are not accurate in assessing the eradication. Antibodies persist in your blood. Hence theyre not able to differentiate between current and prior infection .
What Causes H Pylori Infections
Its still not known exactly how H. pylori infections spread. The bacteria has coexisted with humans for many thousands of years. The infections are thought to spread from one persons mouth to another, like by kissing.
The bacteria may also be transferred through contact with vomit or stool. This can happen when a person does not wash their hands thoroughly after using the bathroom. H. pylori can also spread through contact with contaminated water or food.
Don’t Miss: Stomach Ulcer Treatment Over The Counter
What To Expect After H Pylori Treatment Gastroenterologist Explains
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
What you need to know:
The standard h. pylori treatment course eradicates it in most cases. However, you have a 20% chance of treatment failure. Your doctor often needs to re-test for h. pylori to confirm its eradication.
Treatment of H. pylori improves your symptoms and decreases the risk of ulcers, gastric cancers, and others.
Persistence or recurrence of your symptoms may indicate h. pylori treatment failure.
However, symptoms are not an accurate assessment of treatment failure. Testing is a must.
This Factsheet Is About Helicobacter Pylori
Helicobacter pylori are bacteria, a type of germ, which lives in the sticky mucus that lines the stomach. About 40% of people in the UK have Helicobacter pylori in their stomach so it is very common and in the approximately 8 to 9 out of 10 people who have it, does not cause any problems.
However about 15% of people with the condition get ulcers either in the stomach or in the duodenum . Although ulcers tend to cause indigestion, occasionally they become much more serious as they can bleed or even burst , which happens if the ulcer burrows deep enough into the stomach lining to make a hole. People with ulcers should therefore be treated with the aim of getting rid of Helicobacter pylori.
Because there are millions of people who have both Helicobacter pylori and severe indigestion, it can be tempting to draw the conclusion that one leads to the other. However indigestion is very common and there are many other reasons from suffering from it other than ulcers. The vast majority of people suffering from indigestion will not have ulcers. Helicobacter pylori was only discovered in 1983 so there is still a lot to learn about it.
- Infection: Helicobacter pylori infects the lower part of the stomach .
- Inflammation: Helicobacter pylori causes inflammation of the gastric mucosa . This often does not cause symptoms .
- Ulcer: gastric inflammation may lead to duodenal or gastric ulcer. Severe complications include bleeding ulcer and perforated ulcer.
Read Also: What Is Good For Ulcer Pain