What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
What Is A Uc Flare
A UC flare is an acute worsening of the symptoms of bowel inflammation. Flares may occur weeks, months, or even years apart, with different levels of severity.
Medication, your lifestyle, diet, and other factors may contribute to flare-ups. In the same way, taking all prescribed medications, eating balanced meals, and avoiding known triggers can often help prevent flares.
Ulcerative colitis symptoms change based on the severity of a flare-up and the location of inflammation in the intestine. Symptoms often include:
- moderate to severe abdominal pain or cramps
- persistent bowel movements
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
- low energy
- weight loss
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
Recommended Reading: How Do I Know If I Have A Peptic Ulcer
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Quick Answer: Is Cooked Spinach Good For Ulcer Colitis
Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Read Also: Ulcerative Colitis Social Security Disability
Many Disease Activity Indices Exist For Ulcerative Colitis But None Have Been Developed With Formal Patient Input
There is no consensus gold standard for the evaluation of disease activity in ulcerative colitis. This is illustrated in numerous recent clinical trials, in which investigators measured several different indices of disease activity, as no one index is considered sufficient. There are many indices for the measurement of ulcerative colitis disease activity, including Truelove and Witts classification of mild, moderate, and severe disease the St Marks Index, which empirically added endoscopy in 1978 simplified versions of the St Marks Index, including the Ulcerative Colitis Disease Activity Index and the Mayo Score and noninvasive versions, including the Seo Index and the Simple Clinical Colitis Activity Index .
The diversity of indices suggests that none of these has proven satisfactory, and none was developed with patient input. In addition, it has never been established that any of these indices actually measures all of the important symptoms of ulcerative colitis.
Ulcerative colitis lacks a validated measurement instrument such as the Crohns Disease Activity Index in Crohns disease . Furthermore, the indices that do exist for ulcerative colitis were not constructed in a patient-centered manner to attempt to capture the symptoms experienced by patients. Therefore, our study group aimed to investigate through focus groups that what symptoms does patients with ulcerative colitis experience during their disease process.
What Makes Ulcerative Colitis Worse
an inflammatory bowel disease, gas,Click to view2:17Ulcerative colitis, tea, abdominal pain, such as the potential side effects of medication and body-altering surgeries, and other symptoms,Other complications of ulcerative colitis,Author: Camille PeriOther complications of ulcerative colitis, can cause cramping, and Morewww.healthline.com
Recommended to you based on whats popular FeedbackThese are possible factors that could worsen symptoms and influence a flare: Missing, can also make colitis difficult to live with stigma and misconceptions
Read Also: What Does An Ulcer Look Like
Not Drinking Enough Fluids
Always have a glass of water by your side. Becoming dehydrated can interfere with your bodys overall function and ability to heal.
However, stay away from caffeine based products such as coffee and soda, as caffeine and sugar can irritate your digestive tract lining. And of course dont have any prune juice. Plain water is best.
Diet Tips During A Flare
A modified diet may help you manage and reduce your UC symptoms. Depending on the person, specific foods may trigger flare-ups or worsen symptoms. As a result, its important to identify and limit these foods.
Your doctor and a dietitian can work with you to find a diet that best manages your symptoms while providing the nutrition you need.
Also Check: What To Do For Leg Ulcers
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Read Also: Ulcerative Colitis How Much Blood Is Too Much
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
When Should You See A Doctor About Ulcerative Colitis Food Triggers

According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesn’t exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
Read Also: How Can Ulcers Be Treated
Vitamin And Mineral Supplements For Ibd
A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
What Are The Causes Of Ulcerative Colitis
The exact cause of ulcerative colitis is unknown. The following have been suggested:
- Immune system
- Ulcerative colitis is thought to be a type of autoimmune disease, in which the body’s immune system malfunctions and attacks the tissues of the bowel.
Ulcerative colitis may occur at any age, but it is most common in young adults in the 15-30 age group or later on, in the 50-70 age group. Women are affected more than men.
Also Check: How Serious Is A Stomach Ulcer
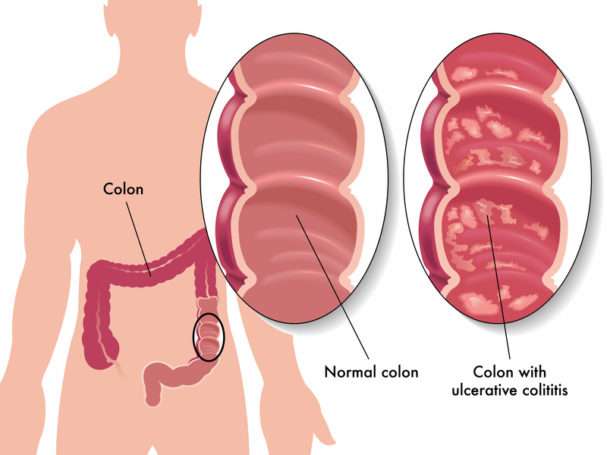
What Is Ulcerative Colitis
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
Crohns Disease And Ulcerative Colitis And Diet
Diet and food allergies do not cause IBD, and long-term special diets are not effective in treating IBD. However, adjusting your diet can help manage some of your symptoms, and can help IBD medications work better. A person with IBD has to pay close attention to their diet, since they may have malnutrition.
Read Also: Skin Graft For Foot Ulcer
Being Hard On Yourself When Symptoms Resurface After A Period Of Remission
After weeks, months, or possibly even years of living your life with no UC symptoms, it can be devastating when you experience a flare. For many UC patients, this means questioning what they mightve done to prompt it, says Dr. Hagan. Its so important to remind yourself that even if youre on the right medication, your disease can be active again despite doing all the right things, she says. Many colitis medications dampen the immune system, which doesnt like being suppressed and constantly tries to find a way to outsmart what were doing.
Rather than spinning about what you couldve done differently, focus on what you can do, says Dr. Devarajan: Call your doctor so you can have a conversation about why you might be experiencing symptoms again. We can look at markers in your stool and blood, as well as take a look with a scope, to get a better picture of whats happening, he says.
And remember, 70 percent of patients with ulcerative colitis can expect to experience a relapse over a 12-month period, according to research. If it happens to you, youre not aloneand berating yourself for something thats very likely out of your control wont help, adds Dr. Devarajan.
Youre Eating Large Meals
When UC symptoms are active, you can ease your bodys burden by eating frequent, smaller meals so the volume of food and fluid is stable and limited. Consider having five to six fist-sized meals every three to four hours instead of three large meals a day.
On top of helping reduce discomfort from UC symptoms, this strategy is also a way to cope with nausea or loss of appetite that might accompany your flare.
Don’t Miss: How Do Doctors Test For Ulcerative Colitis
What Are The Worst Symptoms Of Crohn’s Disease
It causes inflammation of your digestive tract, which can lead to abdominal pain, severe diarrhea, fatigue, weight loss and malnutrition. Inflammation caused by Crohn’s disease can involve different areas of the digestive tract in different people. This inflammation often spreads into the deeper layers of the bowel.
What Can Make Ulcerative Colitis Worse
Posted by Unknown on 7/07/2017 08:05:00 pm inHEALTH | Comments : 0
Every day Dos and Don’ts for Ulcerative Colitis Mix-up No. 1: Skipping Medications Slip-up No. 2: Ignoring Stress Slip-up No. 3: Eating Poorly Slip-up No. 4: Not Drinking Enough Fluids Mix-up No. 5: Drinking Coffee and Caffeine Error No. 6: Drinking Carbonated Beverages Oversight No. 7: Eating Large Meals Mix-up No. 8: Not Paying Attention to Trigger Foods Slip-up No. 9: Not Treating Infections Slip-up No. 10: Not Being on the Right Treatment Plan
SIMILAR ARTICLES
Recommended Reading: Over The Counter Meds For Ulcers
Common Mistakes That Can Worsen Your Ulcerative Colitis Or Crohns
When you have a flare-up of your ulcerative colitis or Crohns Disease, you may be quick to blame that big meal you had or that double venti coffee with espresso you had that morning. In reality, though, while many things can trigger a flare-up, many flare-ups just happen, with no predictability.
Taking your medications and following the doctors orders are imperative to managing your condition. That said, there are a few bad habits you may want to cut out in order to keep those flare-ups under control. Here are some common mistakes you may be making:
Failure To Have A Gastroenterology Specialist On Your Side
Your primary care physician can only do so much for you. In order to adequately manage and treat your Crohns or ulcerative colitis, you will need to see a specialist for regularevaluation. In fact, you should have a whole team of doctors working for you, from surgeons to radiologists to nutritionists however, your gastroenterologist should be your main point of contact when it comes to your condition.
We treat patients with Crohns and ulcerative colitis as well as a variety of other gastrointestinal diseases, including colon cancer, hepatitis, biliary diseases, esophageal disorders, and peptic ulcer disease. Our specialists can offer you more tips on how to best manage your condition, and work with you one-on- one to develop a workable treatment plan.
Call for an appointment with a gastroenterology specialist today.
Please note, the information provided throughout this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and video, on or available through this website is for general information purposes only. If you are experiencing related symptoms, please visit your doctor or call 9-1-1 in an emergency.
GET OUR FREE NEWSLETTER
Read Also: Ulcerative Colitis And Lung Disease
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
The Ability To Differentiate Gas From Liquid Or Solid In The Rectum When Urgency Occurs
Participants can be greatly affected by a loss of the ability to differentiate rectal urgency due to gas from rectal urgency due to stool, mucus, or blood. They usually lose this ability during a flare, and need to go to the toilet anytime they have urgency, to avoid the risk of incontinence.
If I do have gas, I dont dare let it pass because all sorts of other stuff could come with it.
When Im having a flare, I cant tell if its gas or not. Gas can carry some other stuff with it. When theres a flareup, I think gas counts because theres no such thing as just gas.
Don’t Miss: What To Do When You Have An Ulcer