Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK
Treatment For Ulcerative Colitis
Changes in Lifestyle
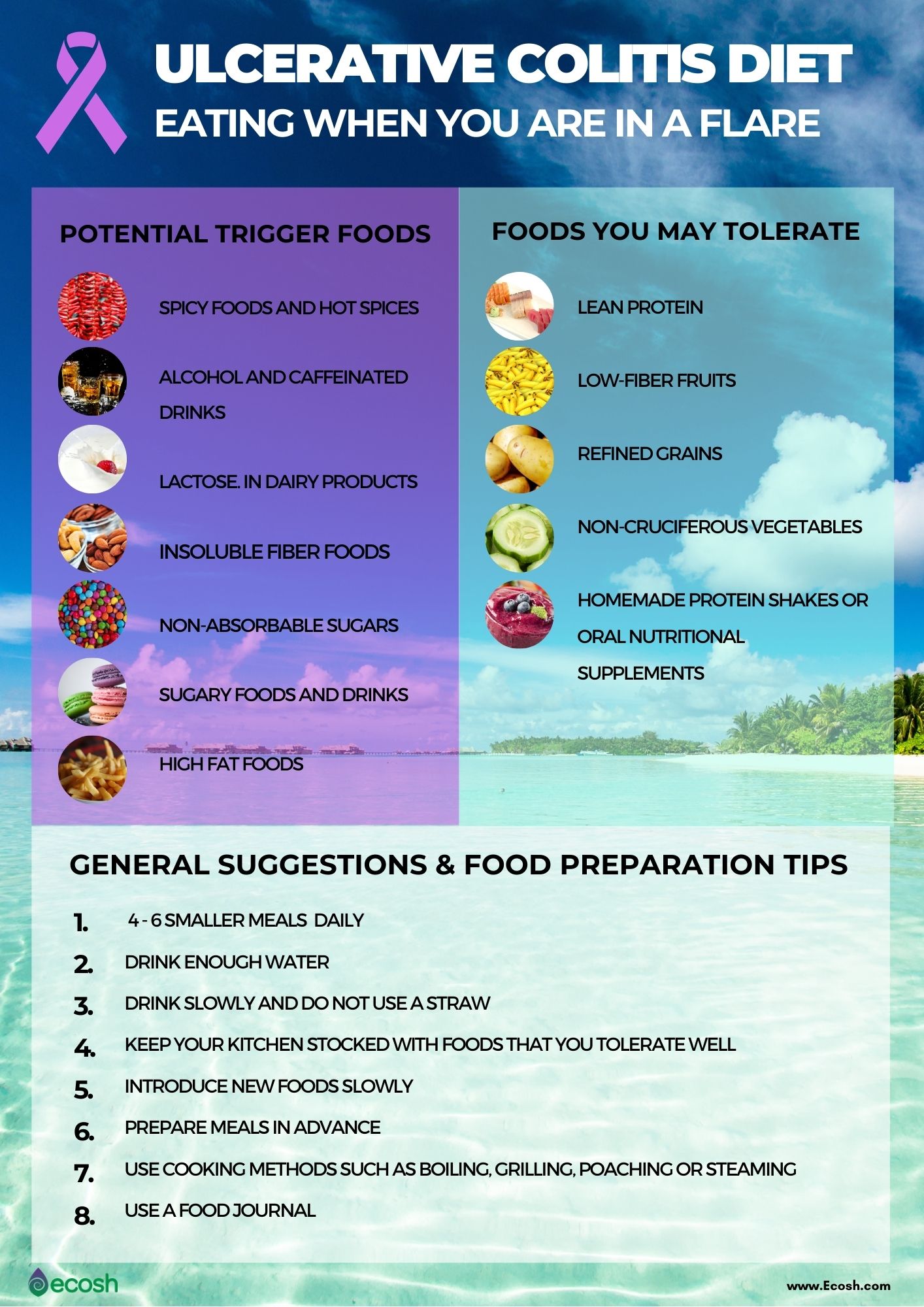
The first thing you need to do if you are suffering from a colitis infection or ulcerative colitis is getting rid of unhealthy habits and adopting healthy ones. You do not exactly need to follow a certain diet plan for your remission of ulcerative colitis, but not consuming foods that you think inflame your gut is the first step to adopting a healthy lifestyle.
For some people, keeping a food journal helps. This way, they can keep a track of their meals and figure out what causes them rectal cramps or bloody diarrhea. Skipping fatty and high fiber meals, and replacing them with small, frequent portions of food high in probiotics will greatly reduce inflammation.
People with ulcerative colitis or UC get dehydrated easily as their large intestine does not do the best job at reabsorbing water and nutrients. Set a goal to drink enough water each day so you can go through your day without feeling symptoms of dehydration. Try using an electrolyte replacement or a meal replacement drink to control your stool symptoms of ulcerative colitis immediately.
Articles On Ulcerative Colitis Overview
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
Don’t Miss: Foods That Irritate Stomach Ulcers
Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders. White blood cells that usually protect you attack the lining of your colon instead. They cause the inflammation and ulcers.
Doctors arenât sure why people get the condition. Your genes may play a role the disease sometimes runs in families. Other things in the world around you may make a difference, too.
Things that can affect your risk of getting ulcerative colitis include:
- Age. Itâs most likely if youâre between 15 and 30 years old or older than 60.
- Ethnicity. The risk is highest in people of Ashkenazi Jewish descent.
- Family history. Your risk could be up to 30% higher if you have a close relative with the condition.
Food and stress donât cause it, but they can trigger a flare of symptoms.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Recommended Reading: Foam Dressing For Diabetic Foot Ulcer
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Don’t Miss: Pressure Ulcer Root Cause Analysis
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Stool Ulcerative Colitis Symptoms
The severity of inflammation in a person with this disease determines the ulcerative colitis stool symptoms presented. While some patients may present some of these, others present most of them to a great degree. The more the severity of inflammation, the more predominant the persisting symptoms are. Some stool symptoms of ulcerative colitis may include:
- Abdominal pain and cramping
- Diarrhea, often with blood or pus in the stool
- Rectal bleeding, often when passing stool
With ulcerative colitis, many people notice flare-ups. They usually occur in a pattern where there comes a period with extreme or active ulcerative colitis and then one of dormancy or remission. During times of high or extreme activity of this inflammatory bowel disease, the ulcerative colitis stool symptoms are recurrent and noticeable. While in periods of dormancy, the person barely presents with any symptoms and may even think they have fully recovered from their condition.
Also Check: When Does Ulcerative Colitis Start
Layers Of The Bowel Wall
The walls of your bowel have layers. The inner layers take in nutrients from food. The outer layers help move food through the gut and waste out of the body.
In Colitis, theres inflammation and swelling of the inner layer of the bowel wall. This can cause bleeding. More mucus may be produced by the inner layer of the bowel wall. Ulcers develop on the inner layer as the condition gets worse, but they can also go as the condition gets better.
The inflammation in Colitis affects how your body digests food, absorbs nutrients and gets rid of waste.
Everyone experiences Colitis differently. When youre having symptoms, its known as active disease, a flare-up or relapse. Symptoms may be mild or severe and are likely to change over time.
Your symptoms may vary depending on where Colitis is active in your bowel and how severe it is. Find out more in the section Types of Colitis.
The most common symptoms are:
Andy
Living with Colitis
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you havent been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If youve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
Dont Miss: Air Mattress For Decubitus Ulcers
Read Also: Ulcer On Eye From Contact Lens
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Living With Ulcerative Colitis Symptoms
Your ulcerative colitis symptoms will likely come and go, with longer periods in between flares when you may not experience any discomfort at all. Those periods are called remission, and they can span months or even years. Because there is not yet a cure for ulcerative colitis, your symptoms will eventually return.
Ulcerative colitis is an unpredictable disease, and the length of periods of remission between flares can make it difficult for doctors to evaluate whether your course of treatment has been effective or not.
Recommended Reading: How To Cure A Bleeding Ulcer
Does Ulcerative Colitis Get Worse With Age
While many conditions do get increasingly worse with age, it appears as though new-onset ulcerative colitis diagnosed in older adults is usually milder than when its diagnosed in younger people.
Generally, older adults have more subtle symptoms of ulcerative colitis than their younger counterparts. But this milder presentation could contribute to delays in diagnosing the condition.
Older adults diagnosed with ulcerative colitis are more likely to experience other forms of inflammatory bowel disease and other non-gastrointestinal chronic health problems.
According to one report, it takes older adults about 6 years to get an accurate diagnosis of ulcerative colitis compared to the 2 years it takes younger adults.
What Are The Possible Complications Of Colitis
Complications usually result from severe, long-term, chronic colitis. They can include:
- Perforation. Chronic inflammation weakens your colon walls, making them more likely to rupture. An ulcer in your colon may wear a hole all the way through. This can cause bacteria from your colon to infect your abdominal cavity and possibly your bloodstream , which would be especially dangerous. Septicemia can lead to .
- Toxic megacolon. Severe inflammation can cause the walls of your colon to dilate and interfere with its natural muscle contractions . This can trap food and gas in your colon . Obstruction leads to painful abdominal distension and an increased risk of rupture.
- Increased risk of colon cancer. Long-term inflammation is associated with cellular changes in your colon wall that can sometimes progress to cancerous changes. The risk increases rapidly after the first decade of chronic colitis.
- Increased risk of other inflammatory diseases. People with inflammatory bowel diseases are more likely to have other inflammatory diseases in other parts of their bodies. Some examples include osteoarthritis and primary sclerosing cholangitis . It appears that uncontrolled inflammation in one area may trigger a similar process somewhere else.
Also Check: Pressure Ulcer Wound Care Dressings
What Is Ulcerative Colitis Symptoms Causes Diagnosis And Treatment
Ulcerative colitis is a type of inflammatory bowel disease in which the lining of the large intestine becomes inflamed.
The colon then develops ulcers that produce blood, pus, and mucus.
The small intestine is rarely affected.
There are several subtypes of ulcerative colitis, which are named according to the part of the colon affected:
- Ulcerative proctitis, which affects only the rectum
- Proctosigmoiditis, which affects the rectum and lower segment of the colon
- Left-sided colitis, which affects the rectum, sigmoid colon, and descending colon up to the sharp bend near the spleen
- Pan-ulcerative or total colitis, which affects the entire colon
How Long Will Ulcerative Colitis Symptoms Last
Ulcerative colitis is a chronic disease with intermittent flares. A flare, or flare-up, is a period of time in which symptoms of ulcerative colitis are severe. Generally speaking, flares can last for weeks or even months, although ulcerative colitis is experienced differently from person to person, and the duration of symptoms varies greatly for each individual.
People living with ulcerative colitis typically experience periods of both active disease and remission.
The goal of treatment is to achieve remission.
Don’t Miss: Magnesium For Horses With Ulcers
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your . Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Read Also: What Not To Eat When You Have Ulcerative Colitis
Rectal Bleeding And Discharge
UC often causes bleeding or mucus discharge from your rectum. You may find spots of blood or mucus in your toilet or on your clothing. Your stool may also become very soft and bloody or contain red streaks or mucus. You may also experience pain in your rectal area, as well as a persistent feeling of needing to have a bowel movement.
Also Check: High Calorie Diet For Ulcerative Colitis
Don’t Miss: Can I Join The Military With Ulcerative Colitis
Outlook For People With Ulcerative Colitis
If you have UC, a doctor will need to monitor your condition, and youll need to carefully follow your treatment plan throughout your life.
The only true cure for UC is removal of the entire colon and rectum. Your doctor will usually begin with medical therapy unless you have a severe complication that requires surgery. Some people will eventually require surgery, but most do well with nonsurgical therapy and care.
When To See A Doctor
For people with ulcerative colitis, it can be challenging to know which symptoms are an emergency, which should prompt a call to the gastroenterologist, and which can wait.
After doing well and having few or no symptoms, when symptoms begin again, it is a reason to call the doctor and get evaluated for a potential flare-up. It may be necessary to change treatments or adjust the current care plan in order to get any inflammation under control quickly.
Ulcerative Colitis Doctor Discussion Guide
Get our printable guide for your next doctors appointment to help you ask the right questions.
In general, symptoms such as severe abdominal pain, excessive bleeding, and signs of dehydration are a reason to seek medical care right away. When possible, calling the gastroenterologist before going to the hospital might help in deciding what level of care is needed.
However, if treatment is needed right away, going to the emergency department may be the best choice. If a serious condition such as a bowel perforation or toxic megacolon is suspected, it may be necessary to call 911, because these are medical emergencies.
Don’t Miss: Is Ulcerative Colitis And Colitis The Same Thing
Signs And Symptoms Of Ulcerative Colitis
Recognizing the symptoms of ulcerative colitis is your first step toward knowing when your disease is in a flare and when to seek medical attention.
The symptoms of ulcerative colitis vary from person to person and about half of all ulcerative colitis patients experience mild symptoms. If you experience any of these symptoms, consult your healthcare provider.
-
Loose and urgent bowel movements
-
Persistent diarrhea accompanied by abdominal pain and blood in the stool
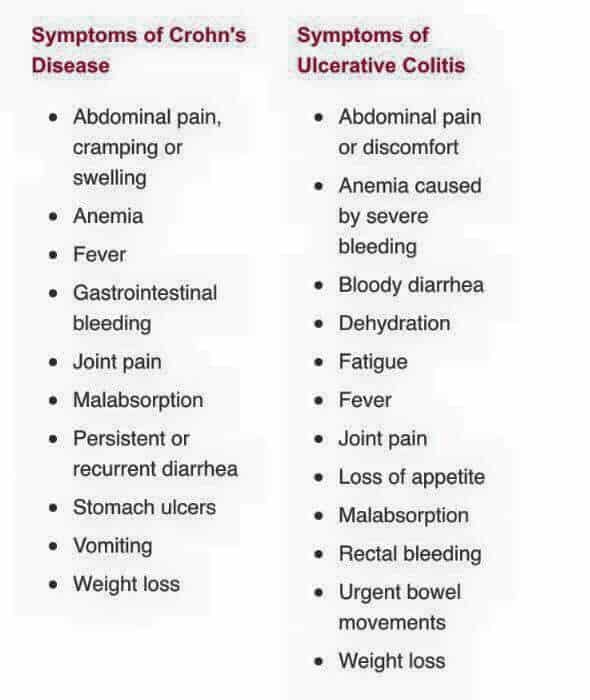
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
Recommended Reading: Sample Meal Plan For Ulcerative Colitis