Review Question: What Are The Most Reliable Techniques/tools To Measure The Dimensions Of A Pressure Ulcer
One systematic review looked at the performance of instruments designed for measuring the dimensions of pressure ulcers. This systematic review was included in the current evidence review and it was subsequently updated to include 1 other study . Overall 13 studies were included in the evidence review.,,,,,,,,,,,, Evidence from these is summarised in the clinical GRADE evidence profile below. The quality of these studies is outlined in .
The OMeara review looked at studies of any design which reported an evaluation of a pressure ulcer measurement instrument as the main focus of the investigation. The authors did not include assessment checklists where the focus was the performance of the tool overall rather than the measurement of pressure ulcer dimensions.
Also Check: Mouth Ulcers Treatment Home Remedies
Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Pressure Ulcers: What To Look For And Document About A Deep Tissue Injury
The professional staff at nursing homes and hospitals must conduct a comprehensive head-to-toe skin assessment on patients most at risk for developing decubitus ulcers. The skin may be compromised, requiring daily skin care to promote health.
Any detected bedsore should be fully documented in the residents healthcare plan to ensure they receive the best care for healing.
Documentation identifying a detectable pressure sore should include:
- The sores location
- The stage of the ulcer
- Pressure ulcers size, including its width, depth, and length, measured in centimeters
- Any identifiable sinus tract, tunneling, or undermining
- The presence of exudate , including its location, amount, and color
- The appearance and size of the wound bed, including a description of visible tissue
- A description of the sores edges, including any evidence of redness, rolled edges, maceration , or induration
- A description of the area surrounding the sore
- The absence or presence of pain
- The absence or presence of any foul odor
The nursing home team must ensure that patients most at risk for developing bedsores are moved at least once every 2 hours. If the patient is sitting in a wheelchair, chair, or recliner, they should readjust their body weight at least once every 15 minutes.
People highly susceptible to developing pressure sores need assistance from nurses, nursing aides, and licensed practical nurses to minimize the potential of falling and causing injury.
Don’t Miss: Do Ulcers Cause Acid Reflux
Summary Of Main Results
We have successfully conducted a network metaanalysis of dressings and topical agents for healing pressure ulcers. Alongside the analysis we have applied a new method of GRADE assessment , which allows us to view the results in the light of our certainty in their findings. Using this approach, we found the majority of the evidence to be of low or very low certainty, and was mainly downgraded for risk of bias and imprecision . This level of uncertainty within the totality of the dataset impacts on all subsequent interpretation of its outputs.
This review includes 51 RCTs involving a total of 2964 participants, comparing 39 different dressings or topical agents for the healing of pressure ulcers. Most of the studies were in older participants, but four included participants with spinal cord injuries and one was in younger people said to be chronically ill or physically disabled. Seventeen studies included participants mainly with Stage 2 pressure ulcers and 15 mainly had Stage 3 pressure ulcers 13 studies investigated treatment of ulcers with a mean duration of less than three months.
We treated each topical agent as a separate intervention, but initially grouped dressings by class as described in the BNF 2016 . The network involved 39 studies in 2116 participants, encompassing 21 different interventions in 27 direct contrasts and these informed 210 mixed treatment contrasts.
Protect The Periwound Skinexpand: More
Askina® Barrier Cream acts as a protectant and moisture barrier against maceration caused by incontinence or bodily fluids, to protect sensitive, fragile skin and severely dry skin, including peri-wound areas. It is indicated for use on intact skin.
Askina® Barrier Film Swab and Askina® Barrier Film Spray are sterile liquid dressings intended to form a uniform, transparent film when applied to the skin. The film can provide oxygen and moisture permeability. Both dressings are indicated for use on intact or damaged skin.
Description
- Manage bacterial load and odor
- Manage exudate and promote moist healing
- Protect the periwound skin
Recommended Reading: Foods You Should Not Eat With Ulcerative Colitis
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Appendix 11 Time To Event Data: Direct Evidence
The duration of followup ranged from 3 to 26 weeks, but the distribution was insufficient to allow modelling of time dependence in the network.
Seven studies reported timetoevent data. We calculated the hazard ratio using the method and spreadsheet from Tierney 2007 one study reported the hazard ratio directly, adjusted for exudate level. The timetohealing data are shown in Analysis 3.1 and summary statistics for the timetohealing and the proportion healed are compared in Table 22 for the studies that report both healing outcomes.
In the individual network, two studies in 95 participants suggested that the time to healing may have been quicker for hydrocolloid versus saline gauze there was no heterogeneity . One study in 24 participants suggested healing may have been quicker for collagenase ointment compared with hydrocolloid . In the other studies, the CI showed much uncertainty.
There was some suggestion of a time dependent effect because there were qualitative and quantitative differences between the HR and the RR: for shorter studies , the HR gave a smaller effect than the RR, but for the medium and longer term studies the HR gave a larger effect than the RR, suggesting that wounds that heal do so relatively quickly.
Analysis
Comparison 4 Direct evidence: group interventions, timetohealing data, Outcome 1 Timetohealing .
Recommended Reading: How To Prevent Pressure Ulcers On Heels
What Are Pressure Sores
Pressure sores are sores on your skin. Theyre caused by being in a bed or wheelchair nearly all the time. Sometimes theyre called bedsores or pressure ulcers. The sores usually develop over the bony parts of your body. Those are places with little padding from fat. Sores are common on heels and hips. Other areas include the base of the spine , shoulder blades, the backs and sides of the knees, and the back of the head.
People who need to stay in bed or in a wheelchair for a long time are at greater risk of developing pressure sores. This can include people who are paralyzed and those who arent able to get up on their own. But even some people with short-term illness and injuries can get pressure sores. Sores can happen if they have to stay in bed or a wheelchair while they heal. Lastly, some chronic diseases make it hard for pressure sores to heal. Those include diabetes and hardening of the arteries.
Description Of The Condition
Pressure ulcers, also known as pressure injuries, bedsores, decubitus ulcers or pressure sores, are localised areas of injury to the skin, the underlying tissue or both. They often occur over bony prominences such as the sacrum and heel , and are caused by external forces such as pressure, or shear, or a combination of both .
Risk factors for pressure ulcer development have been summarised into three main categories: a lack of mobility poor perfusion and low skin status the latter category includes the presence of stage 1 pressure ulcers or incontinence or both, which also increases the risk of ulceration by producing a detrimental environment for the skin .
Prevalence
Pressure ulcers are one of the most common types of complex wound. Prevalence estimates differ according to the type of population assessed, the data collection methods used and period of data collection and whether Stage 1 ulcers were included).
One large European study estimated a hospital pressure ulcer prevalence of 10.5% whilst a US study estimated a prevalence of 9.0% across acutecare, longterm care and rehabilitation settings ). In the UK, national pressure ulcer data are collected across community and acute settings as part of the National Health Service Safety Thermometer initiative . About 4.4% of patients across these settings were estimated to have a pressure ulcer in November 2014 .
Treatments for pressure ulcers
Impact of pressure ulcers on patients and financial costs
Read Also: Diet To Heal Leg Ulcers
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
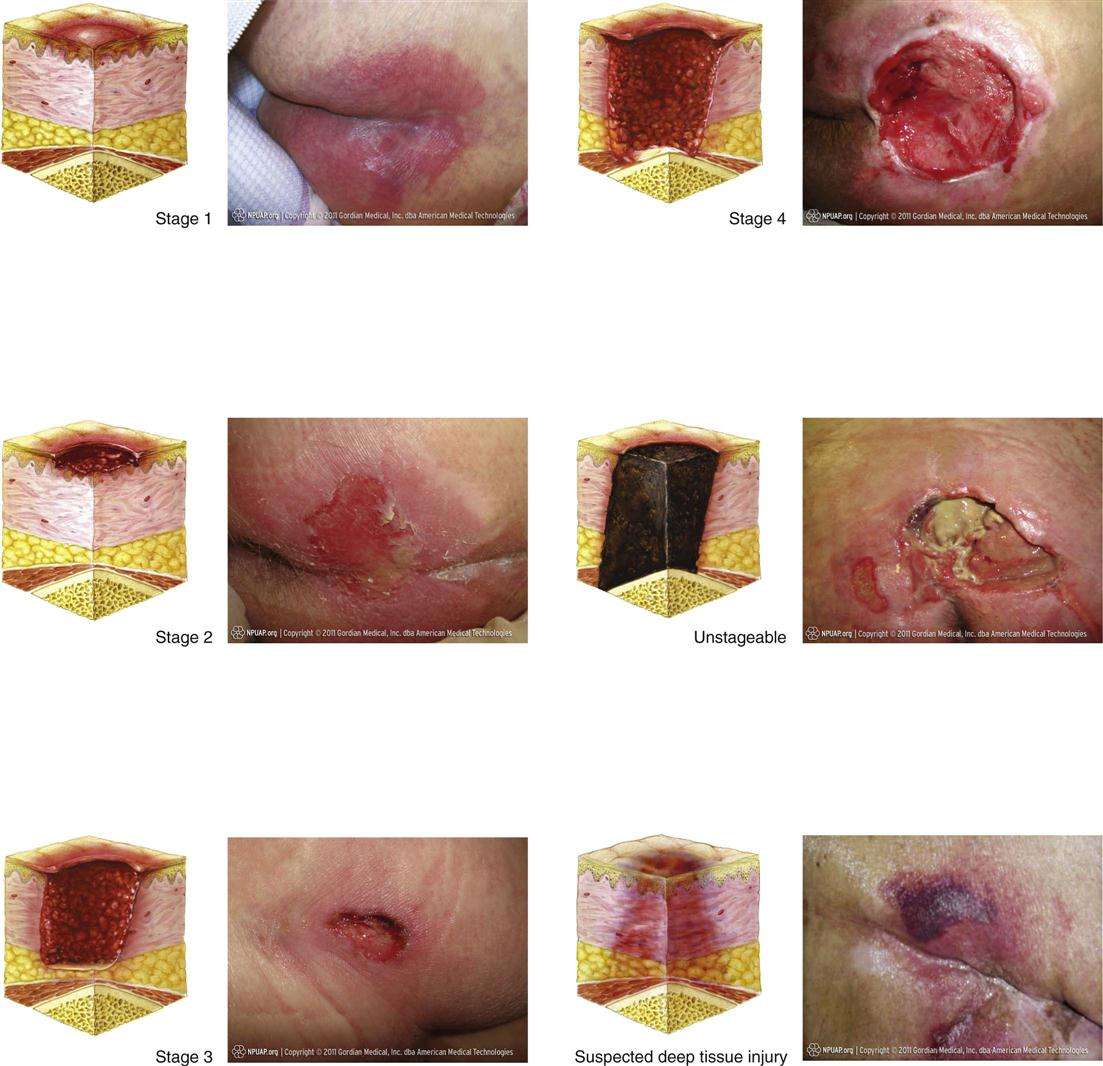
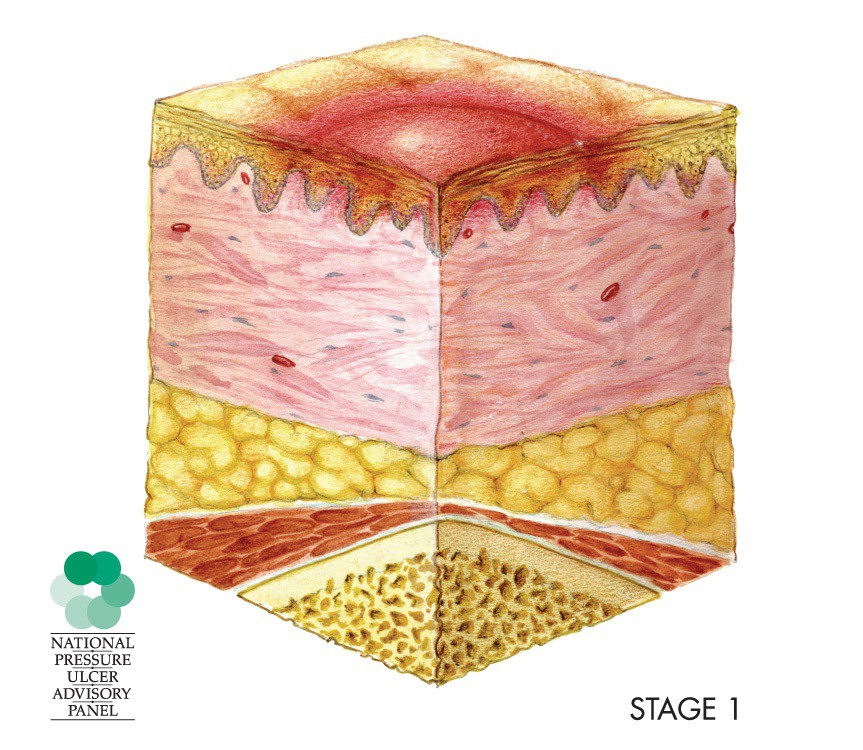
What Do Stage 1 Bedsores Look Like
Stage 1 bedsores typically appear as red-colored patches of skin that do not blanch. This means that the red-colored patch of skin does not turn white when a finger is pressed upon the irritated area. On a dark-skinned patient, a stage 1 bedsore may simply appear to be a different color than the surrounding skin. It will not necessarily be red in color, but the affected skin may appear purple or blue.
Recommended Reading: Natural Remedies For Stomach Ulcers In Humans
Questions For Your Doctor
- What should I do if I or a loved one has pressure sores and is too heavy to move?
- Does an adjustable bed help reduce the risk of pressure sores?
- Can you die from an infected pressure sore?
- Is diabetic foot ulcer the same as a pressure sore?
- Can you get pressure sores from sitting in the same position in your job for longer than 2 hours at a time?
Appendix 10 Ranking Interventions
Data for each intervention were shown as the probability that each intervention is the best, second best, third best treatment, etc. . There was substantial overlap of the individual rankograms, illustrated in Figure 21, which intentionally shows the confusion, together with some indication that dextranomer and tripeptide copper gel may be the best treatments and that the worst treatments may be the sequential hydrocolloidalginate dressings and sugar plus egg white. Across all treatments there was considerable uncertainty in the ranking of interventions and no intervention had more than 50% probability of being the best treatment. This, together with the mean rank being no higher than 3.6 and no lower than 18.6 , and no SUCRA value being 0 or 1, reinforces our view of the considerable uncertainty around treatment estimates in this network.
Rankograms combined individual networkKey to interventions: 1: saline gauze 2: alginate dressing 3: sequential hydrocolloid alginate dressings 4: basic wound contact dressing 5: collagenase ointment 6: dextranomer 7: foam dressing 8: hydrocolloid dressing 9: hydrocolloid +/ alginate 10: hydrogel dressing 11: ineligible radiant heat 12: ineligible skin substitute 13: iodinecontaining dressing 14: phenytoin 15: proteasemodulating dressing 16: PVP + zinc oxide17: silicone + foam dressing 18: soft polymer dressing 19: sugar + egg white 20: tripeptide copper gel 21: vapourpermeable dressing
You May Like: Best Smoothies For Ulcerative Colitis
Enhancing Healthcare Team Outcomes
The primary goal is to prevent pressure ulcers through various means including the use of air-fluidized or foam mattresses, improving the nutritional status of the patients, proper placing of patients in bed, changing position frequently, and treatment of the underlying diseases. A treatment plan involves the removal of all devitalized tissue that may serve as a reservoir for bacterial contamination . Also, it involves dressing by utilizing hydrogels, hydrocolloids, or saline-moistened gauze to enable granulation tissue to grow and the wound to heal. Treatment of underlying infection by topical or systemic antibiotic medications might be needed to help in the healing process, but tissue culture should be obtained before selecting the accurate drug. Pain and discomfort can be controlled by analgesics. A dietary consult should be made to ensure that the patient is receiving adequate calories. When possible, the patient should be out of bed to chair, and physical therapy should be consulted for ambulation and/or exercise. Wound care specialty trained nurses should assist in dressing changes, debridement of wounds, and provide close followup care. The nurses should also assist the clinician in the education of the patient and family. Pressure ulcers are very difficult to treat, it is crucial that the nurses and clinicians work together as an interprofessional team to provide the very best care including treatment, monitoring, and followup care.
Outcomes
What Do Bed Sores Look Like
Bed sores look different at each of the four stages. Most often, there is not much to see with Stage 1 and Stage 2 bed sores. However, Stage 3 and Stage 4 bed sores can appear as terrible, open wounds.
Also, bed sores may look different depending on the part of the body in which they occur. For example, a bed sore on the sacrum, coccyx, or buttocks will appear differently than a bed sore on the heal. Generally, this is the case because some parts of the body where pressure is applied have more tissue, muscle, and skin that may be deteriorated.
Don’t Miss: Aip Diet For Ulcerative Colitis
How Can You Tell If You Have A Pressure Sore
Sometimes, a pressure ulcer can be difficult to identify, especially in the early stages. Here is some information about the symptoms and signs that may indicate that you have a stage 1 pressure ulcer.
- Discolored, reddened, or darkened skin is one of the first signs of a pressure ulcer. For individuals with darker skin, purple, bluish, and shiny areas are one of the first signs. The area may feel warm or hard.
- If you remove pressure from the afflicted area for 30 minutes and the skin does not go back to normal, a pressure ulcer has begun to form.
- Press on the afflicted area with your finger to do the blanching test. Once the area goes white, you should remove the pressure. If the area remains white, this means blood flow has been impaired. The blanching test may not be as effective when it comes to dark skin.
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
You May Like: Crohn’s Versus Ulcerative Colitis Pathology
Agreements And Disagreements With Other Studies Or Reviews
We have been unable to identify any network metaanalyses directed at healing pressure ulcers and incorporating both dressings and topical agents. The AHRQ guideline reviewed the evidence for dressings in a series of pairwise comparisons and stated that overall, they did not find substantial evidence to support certain local wound applications over others . The most recent NICE guideline on the prevention and management of pressure ulcers considered all RCT evidence on dressings and separately all RCT evidence on topical agents. NICE recommendations are to not use saline gauze dressings and for the health professional and adult to discuss the type of dressing to use, taking into account pain and tolerance, position of the ulcer, amount of exudate and frequency of dressing change. These recommendations rely heavily on consensus decisions, weakly supported by the evidence, and as such, agree with the findings of this review.
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
Don’t Miss: Artificial Sweeteners And Ulcerative Colitis