Crohns Disease And Ulcerative Colitis
A serious but rare complication of these forms of inflammatory bowel disease is fulminant or toxic colitis, formerly called toxic megacolon.
The signs and symptoms of this condition can include bloody diarrhea along with fever, racing heartbeat , low blood pressure , metabolic acidosis , low urine output , and acute kidney failure.
Toxic colitis is more common with ulcerative colitis than it is with Crohns disease.
Read Also: Foods To Avoid With Peptic Ulcer
Treating Ulcerative Colitis Is Important To Prevent Complications
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
Ulcerative colitis is a chronic illness that is a type of inflammatory bowel disease . Ulcerative colitis is usually characterized as causing inflammation in the lining of the colon, but it is an immune-mediated condition. This means that it involves the bodys immune system, which can lead to effects in organs and body systems other than the digestive tract.
A diagnosis of ulcerative colitis is difficult to receive for many reasons. Often people have not even heard of the disease before their diagnosis. Learning that it will probably mean taking medication for the rest of their lives can be upsetting and daunting.
In addition, ulcerative colitis goes through periods of active disease and less active or no activity . Little is currently known about why ulcerative colitis might flare-up, though some people living with the disease are able to identify their personal triggers.
How You May Feel
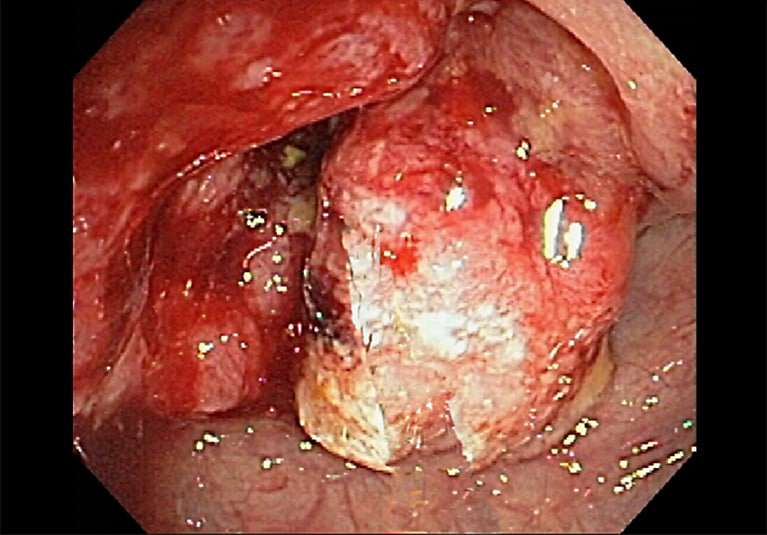
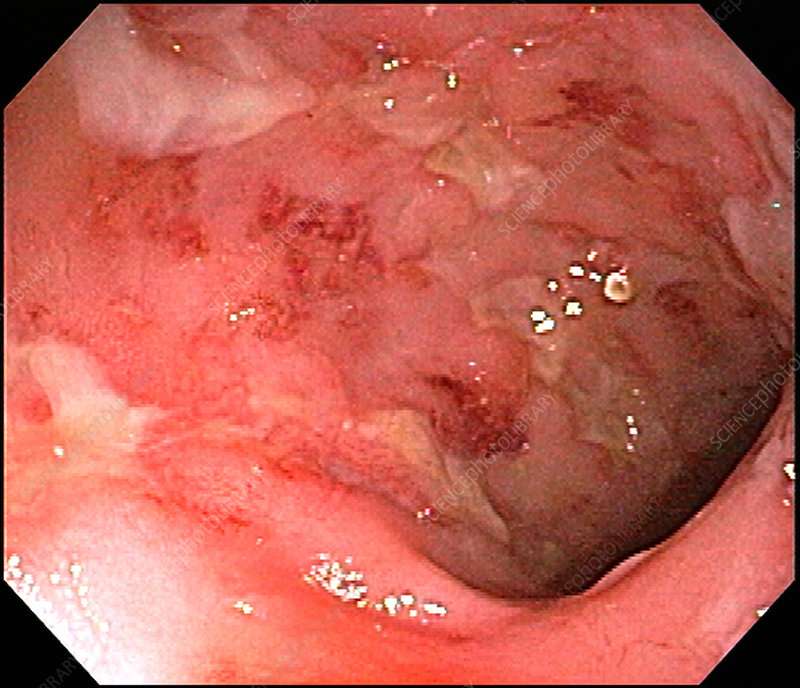
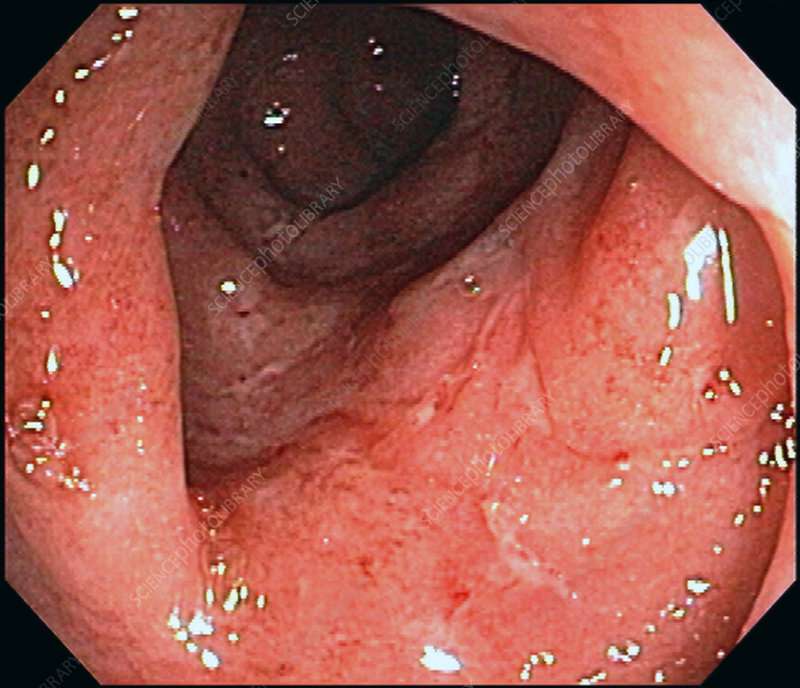
Ulcerative colitis attacks the lining of your digestive tract. It causes swelling and sores in the lining.
If youâve just been diagnosed with it, hereâs what might happen during a flare-up:
You might have some of those symptoms, but not all. And they may change over time. They can range from very mild to very bad.
Read Also: Diet Plan For Ulcerative Colitis Flare Up
What Are The Complications Of Ulcerative Colitis
Ulcerative colitis may lead to complications that develop over time, such as
- anemia, a condition in which you have fewer red blood cells than normal. Ulcerative colitis may lead to more than one type of anemia, including iron-deficiency anemia and anemia of inflammation or chronic disease.
- bone problems, because ulcerative colitis and corticosteroids used to treat the disease can affect the bones. Bone problems include low bone mass, such as osteopenia or osteoporosis.
- problems with growth and development in children, such as gaining less weight than normal, slowed growth, short stature, or delayed puberty.
- colorectal cancer, because patients with long-standing ulcerative colitis that involves a third or more of the colon are at increased risk and require closer screening.
In some cases, ulcerative colitis may lead to serious complications that develop quickly and can be life-threatening. These complications require treatment at a hospital or emergency surgery. Serious complications include
Severe ulcerative colitis or serious complications may lead to additional problems, such as severe anemia and dehydration. These problems may require treatment at a hospital with blood transfusions or intravenous fluids and electrolytes.
Inflammation In Other Areas
Some people with IBD have painful inflammation in other areas of the body, including:
- joints of the fingers, hands, feet, ankles and knees
- joints of the spine, including vertebrae and sacroiliac joints
- eyes
Two specific skin problems that can occur as a result of IBD are:
- pyoderma gangrenosum small, sunken ulcers on the skin
- erythema nodosum painful, small, reddened nodules on the skin .
Don’t Miss: Hind Gut Ulcers In Horses Symptoms
Early Recognition Close Monitoring And Timely Re
Any patient meeting the criteria for severe disease should be recognized promptly and admitted in the hospital. Stool cultures for enteric pathogens and Clostridium difficile should be taken at the earliest possibility but results should not be awaited before rapid IV corticosteroid therapy. Flexible unprepared sigmoidoscopy with minimal air insufflation should be performed within 24 hours of admission to confirm diagnosis and exclude a superimposed infection with the cytomegalovirus .3,8
Following initiation of corticosteroid therapy patients should be closely monitored with daily blood works, clinical examination and serial abdominal films as clinically indicated. Positive stool cultures should prompt treatment with antibiotics, presence of a significant amount CMV inclusions on colonic biopsy are an indication for ganciclovir treatment. Formal re-assessment is performed between days 3 and 5.3,8 As discussed above, current evidence does not allow for a singular recommendation. Failure of corticosteroid therapy is therefore based on a clinical, biochemical and radiological assessment. Several indices such as stool frequency, CRP and albumin levels and colonic dilatation on plain radiography can be used as described above.
Ways To Have Healthy Sleep With Ulcerative Colitis
1. Change your sleeping position
Sleeping position makes a great deal in terms of relieving pain and having better sleep. Choose a sleep position in which you feel more comfortable, mostly sleep straight against your back. This sleeping position suits most of the people who suffer from this disease. Certain sleeping positions may increase the flares and inflammation in intestines. So to reduce the symptoms and inflammation it is better to change your sleeping position till ulcerative colitis gets treated.
2. Revise your Medications
This is required because sometimes the medications which are going are not that effective on your body and needs to be changed. If the medication is not helping you with the disease, then it might increase pain rather than giving relief from it. Also certain UC medicines can also cause difficulty in sleeping like corticosteroids. This medication is used for controlling ulcerative colitis flares but it gets hard to sleep after taking this medicine. You need to consult you doctor for change in medication or alternative medicine. The doctor may advice you the following-
- To change medication
- Adding some medicine or pills to help you sleep
- Changing the time of medication to day time
3. Eat Dinner Early
Triggers of UC related to diet include the following-
- Lactose
4. Improve your Mental Health
5. Practise Good Sleeping Habits
6. Heating Pads and Sleep Aids
- Diarrhoea
Also Check: Will Ulcer Cause Back Pain
Health Problems Affecting Other Parts Of The Body
Some people with ulcerative colitis also have inflammation in parts of the body other than the large intestine, including the
- joints, causing certain types of arthritis
- skin
- liver and bile ducts, causing conditions such as primary sclerosing cholangitis
People with ulcerative colitis also have a higher risk of blood clots in their blood vessels.
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Also Check: Arterial Ulcer Vs Venous Ulcer
Complications Caused By Nutritional Deficiencies
Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
Inflammation And Your Immune System
Inflammation is your immune systems normal reaction to protect your body from bacteria, viruses, and other potentially harmful substances. However, for people with UC, the immune system is mistakenly triggered to attack the inner lining of the large intestine. This results in excess inflammation, leading to the symptoms of UC.
Although it isnt known for sure what triggers the excess inflammation, too much of the protein TNF alpha may be to blame. Your bodys immune system naturally produces TNF alpha, but if you have UC, your body may be producing too much of it.
Read Also: Mouth Ulcer On Tongue Causes
What You Eat In The Morning
While eating certain foods does not usually trigger IBD flares, it could worsen existing flares and symptoms. The Crohns & Colitis Foundation recommends avoiding the following food categories that can worsen a persons symptoms during a flare:
- Greasy, fried foods Fast food, fried potato chips, donuts, etc.
- High-fiber foods Raw vegetables and fruit
- Gas-inducing foods Beans, cabbage, broccoli
- Gas-inducing drinks Caffeinated or carbonated beverages
- Problem foods Foods you recognize as personal flare triggers
When To Contact A Doctor
People need to discuss any blood in the stools with their doctor, even if they have experienced it before.
A person may also wish to monitor their UC symptoms, so they know what is usual for them to experience. People can then discuss any abnormal symptoms with a healthcare professional.
If individuals have ongoing diarrhea that lasts for a couple of weeks, they can contact their doctor to discuss concerns and treatment.
The Crohnâs and Colitis Foundation advises people to seek emergency medical attention if they experience any of the following:
- inability to keep down liquids due to nausea, vomiting, or pain
- rectal bleeding with blood clots in stools
- continuous pain
Managing UC with treatment may help reduce bleeding. There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding.
Anti-inflammatory medications for UC can include:
- 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
- Corticosteroids: A short-term treatment to help reduce inflammation.
- Immunosuppressants: These medications can help suppress the immune response that can cause inflammation. However, they may take up to 6 months to be effective.
- Biologics: For treatment of moderate to severe UC, biologics help block molecules that trigger inflammation.
Read Also: What Can I Take For A Stomach Ulcer
Optimal Dose Targeting Is Primordial
Several lines of evidence suggest that conventional weight-based dosing of infliximab salvage therapy might be insufficient in ASUC. The severe intestinal inflammation is associated with an important intestinal loss of protein resulting in hypoalbuminaemia but also a rapid clearance of infliximab in the faeces.58 Additionally, high concentrations of mucosal metalloproteinases, associated with inflammation, lead to degradation and inactivation of anti-TNF antibodies.59,60
In a pharmacokinetic study, Brandse et al showed that patients with a faster intestinal clearance of infliximab were at risk for worse clinical outcomes and had an increased chance of infusion-related reactions compared to patients with a normal drug clearance. Drug clearance seemed to be highest in the group of patients with higher CRP levels .59 In a retrospective analysis of 50 patients hospitalized for ASUC an accelerated dosing strategy of infliximab was associated with a lower colectomy rate .61 However, in another multicentre, retrospective study including 213 patients with steroid refractory ASUC no difference was found between normal and accelerated dosing strategy, although dosing regimens including a higher induction dose of infliximab were associated with a lower rate of colectomy.62
Patients not responding to rescue therapy with infliximab or cyclosporin by day 7 or that develop serious complications earlier should be referred for colectomy.25
What Causes Ulcerative Colitis
Ulcerative colitis is thought to be an autoimmune condition.
This means the immune system, the body’s defence against infection, goes wrong and attacks healthy tissue.
The most popular theory is that the immune system mistakes harmless bacteria inside the colon for a threat and attacks the tissues of the colon, causing it to become inflamed.
Exactly what causes the immune system to behave in this way is unclear.
Most experts think it’s a combination of genetic and environmental factors.
Read Also: Foods To Eat To Help Ulcers
Is Ulcerative Colitis Curable
Ulcerative colitis can differ from person to person, but its usually a lifelong condition. Symptoms come and go over time.
Youll have flare-ups of symptoms, followed by symptom-free periods called remissions. Some people go years without any symptoms. Others experience flare-ups more often.
Overall, about half of people with ulcerative colitis will have relapses, even if theyre being treated.
Youll have the best outlook if the inflammation is only in a small area of your colon. Ulcerative colitis that spreads can be more severe and harder to treat.
The one way to cure ulcerative colitis is with surgery to remove your colon and rectum. This is called proctocolectomy. Once your colon and rectum are removed, youll also be at lower risk for complications like colon cancer.
You can improve your own outlook by taking good care of your ulcerative colitis and getting regular checkups to look for complications. Once youve had ulcerative colitis for about eight years, youll also need to start having regular colonoscopies for colon cancer surveillance.
It can be helpful to talk to others who understand what youre going through. IBD Healthline is a free app that connects you with others living with ulcerative colitis through one-on-one messaging and live group chats, while also providing access to expert-approved information on managing the condition. Download the app for iPhone or Android.
Ibd And Changing Your Diet
Some dietary changes that may help a person with IBD include:
- Low-fibre diet when IBD is active, most people find a bland , low-fibre diet helps to ease diarrhoea and abdominal cramping. People with Crohns disease who have a narrowed small intestine may need to eat a low-fibre diet most of the time.
- Low-fat diet people with Crohns disease who experience steatorrhoea may benefit from a low-fat diet.
- Low-lactose diet the milk sugar lactose is broken down by the enzyme lactase, commonly found in the lining of the small intestine. Some people with Crohns disease lack this enzyme, so should avoid milk and other dairy products. Lactose intolerance can be diagnosed with a simple test ask your doctor.
- Liquid diet a person with severe Crohns disease may need a nutritionally balanced liquid diet.
- Plenty of water people with IBD need to drink plenty of fluids to prevent dehydration.
Also Check: How Does Alcohol Affect Ulcerative Colitis
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
What To Eat During A Flare
All of the diets above are intended to be temporary and followed during a flare-up. Working with a dietitian can help prevent deficiencies in certain micronutrients, which is common with IBD.
During a flare its helpful to eat four to six small meals per day rather than fewer larger meals. Its also very important to drink fluids because diarrhea can occur with a flare and cause dehydration.
Recommended Reading: What Causes Ulcers On The Feet
Causes Of Ulcerative Colitis
Ulcerative colitis is the result of several factors that are not yet well understood. Abnormal immune response, genetics, microbiome, and environmental factors all contribute to ulcerative colitis.
Research suggests that ulcerative colitis could be triggered by an interaction between a virus or bacterial infection in the colon and the bodys immune response.
-
Typically, the cells and proteins that make up your immune system protect you from infection.
-
A normal immune response would cause temporary inflammation to combat an illness or infection. The inflammation would then go away once you are healthy and free of the illness.
-
In ulcerative colitis patients, the inflammation persists long after the immune system should have finished its job. The body continues to send white blood cells into the lining of the intestines, where they produce chronic inflammation and ulcers.
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Don’t Miss: How To Relieve A Stomach Ulcer
Treatment Of Ulcerative Colitis
Vedolizumab is a drug for people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The most serious side effect it causes is increased susceptibility to infection. Vedolizumab has a theoretical risk of a serious brain infection called progressive multifocal leukoencephalopathy Progressive Multifocal Leukoencephalopathy Progressive multifocal leukoencephalopathy is a rare infection of the brain that is caused by the JC virus. People with a weakened immune system are most likely to get the… read more because this infection has been reported with the use of a related drug called natalizumab.
Ustekinumab is another kind of biologic agent given to people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The first dose is given by vein and then by injections under the skin every 8 weeks. Side effects include injection site reactions , cold-like symptoms, chills, and headache.