Green Banana & Applesauce
Both green bananas and cooked and cooled apples are high in soluble fibers and resistant starches which help to slow down transit and soak up excess moisture which can be helpful if diarrhea is a concern. According to theUniversity of Wisconsin Health, applesauce is helpful for ulcerative colitis and are a rich source of vitamins and minerals like potassium.
Nutritions Role In Treating Uc
Your health care provider can help you make up for these nutritional deficits by identifying foods to help control your UC symptoms and provide you a well-balanced, nutritious diet.
Certain foods or beverages may irritate your digestive tract and trigger flare ups of UC symptoms. Your health care provider will help you identify these foods, so you can avoid them and identify substitute foods that provide the same nutrients, without flare ups.
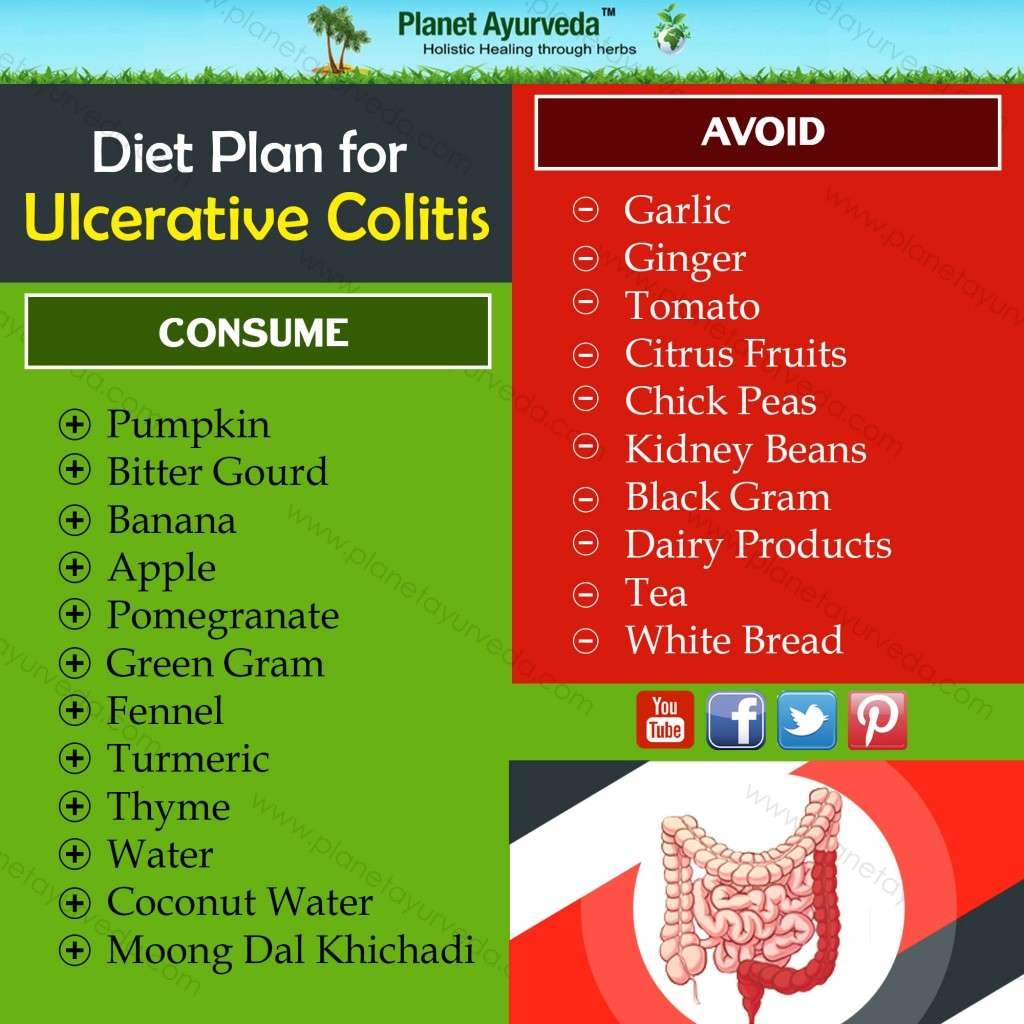
Foods more likely to trigger UC symptoms include:
-
Plant foods that contain insoluble fiber, such as fruits with skin or seeds raw green vegetables, especially cruciferous vegetables, such as broccoli or cauliflower whole nuts or whole grains and anything with a peel
-
Lactose, a sugar in dairy products, such as milk, cream, and soft cheeses
-
Sugary foods such as pastries and juices
-
Non-absorbable sugars: sugar alcohols found in sugar-free gum, candy, ice cream, and certain types of fruits/juices such as pear, peach, and prune
-
High-fat foods, including fried or greasy foods, butter, coconut, margarine, and cream
Recommended foods for UC include:
-
Refined grains, such as sourdough, potato, or gluten-free bread, white pasta, white rice, and oatmeal
Your health care provider may also recommend:
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, the symptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Read Also: Can Ulcer Cause High Blood Pressure
My Health Journey With Ulcerative Colitis
I feel like it is long overdue for me to share my health story on here! I have spent a long time trying to not talk about this disease, to downplay symptoms, and to pretend like it doesnt exist. But it is a part of me and always will be, so I am trying my best to be more open, more vulnerable, and more real. So let me tell you about my journey with ulcerative colitis.
I was first diagnosed with ulcerative proctitis, which is a pretty mild form of inflammatory bowel disease , in 2013. To be honest, once I started taking medication, I would completely forget I had it most days. I carried out life just as usual, eating whatever I wanted and going out all the time. Then things started to get a little more serious and I wasnt feeling so great. I got re-tested in 2017 and found out that things had progressed a lot, and I was then diagnosed with ulcerative colitis . UC and Crohns disease are the two diseases that make up IBD. Both UC and Crohns disease are autoimmune diseases UC affects just the colon , while Crohns can affect any part of the GI tract.
Its truly mind-blowing how prevalent autoimmune diseases are becoming especially in women. I can count four other people in my groups of friends that have autoimmune diseases most of them affecting the gut. I have become a tad obsessed with learning about autoimmunity and especially the role the gut microbiome plays in it, so you can expect more posts on these topics.
xx Cami
Dont Miss: Specific Carbohydrate Diet Ulcerative Colitis
Add In Meal Replacement Shakes As Necessary
Many experts recommend meal replacement shakes or nutritional supplements, like Ensure Plus or Boost, to help with weight maintenance. Liquid supplements like these take up very little volume and are easy on the stomach, but they contain a relatively high amount of calories and protein.
I eat every two or three hours, even if its a couple of crackers, and drink a meal replacement shake. This helps me maintain my weight, said a member.
Note that these shakes often contain dairy products, so talk with your doctor for their recommendation, especially if you are sensitive to dairy or are lactose intolerant.
Also Check: Is Ulcerative Colitis A Serious Disease
Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs they typically develop over time. Most people experience mild to moderate symptoms, but the course of ulcerative colitis may vary and some people have long periods of remission. The symptoms depend on the location of the disease-causing inflammation. If you have ulcerative colitis, you may have the following signs and symptoms:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- An increased risk of blood clots in veins and arteries
Whole Grain Breads Cereals And Pastas
Whole grain flour is high in fiber because it hasnt had the germ or bran removed.
Its important to avoid eating food made from any whole grain flour, such as:
, including beans, lentils, and peas, are high fiber, high protein foods. Because of the indigestible sugars in beans, theyre also notorious for causing gas. If you are experiencing a UC flare-up, youll want to pass on the following:
- all beans, including chickpeas
- soy nuts, including soybeans and edamame
You May Like: Skin Graft Diabetic Foot Ulcer
Finding The Right Uc Diet For You
For those living with ulcerative colitis, choosing the right foods to eat may feel overwhelming. If you are worried you may not be getting enough of one or more nutrients, speak with your gastroenterologist. They may test your blood for nutrient levels to find out whether you are deficient. If you are deficient in any nutrient, your doctor may recommend a safe and effective dietary supplement.
You can also request a referral to a registered dietitian who can work with you to get the most out of the nutrients in the foods youre able to eat. Working with a registered dietitian or nutritionist can also help you navigate life events, such as parties, dining out, vacations, and more. Understanding what triggers your flare-ups life stress or specific foods is important information that a food journal can help you decipher.
The good news is that for people with UC who establish a healthy and safe diet plan, sticking to it often helps them feel better and manage symptoms. Feeling pretty good today, wrote one MyCrohnsAndColitisTeam member. Ive gone lactose- and gluten-free, and symptoms have reduced a lot. Also gave up caffeine. Living on avocado!
Should You Take Nutritional Supplements With Uc
In some cases, you may not be able to get all your nutritional needs directly from food your intestines just cant do their best nutrient-absorbing job when its dealing with ulceration. Thats where supplements come in. Again, its important to understand that theres not a set list of supplements that everyone with UC should takeit really varies from person to person.
Your GI or registered dietitian will recommend supplements based on your specific situation after looking at your symptoms and test results. And always get the green light from your doctor before adding a supplement to your routinesome may actually contain sugar alcohols, lactose, and preservatives that can actually aggravate your symptoms.
That said, here are some supplements that are commonly recommended for people with UCdont forget to take them on a full stomach, or else they could irritate your GI tract:
Keep in mind, this isnt an exhaustive list of possibilitiesyour doctor may recommend other vitamin or mineral supplements, including potentially a multivitamin, depending on your specific nutritional needs.
Recommended Reading: Where Does Ulcerative Colitis Occur
How To Identify Your Trigger Foods
Theres no way around this one: Youve got to Even if you work with an R.D. , this will be an important part of that process. For example, maybe you realize that every time you eat dairy, diarrhea follows a few hours later. Or maybe a night of drinking really sparked a flare-up. Watch for patterns like this and make note. And dont forget to take your food diary with you to your doctors appointmentsit can be a useful tool to help you and your health care team figure out how best to manage your UC. You can go the old-fashioned route and use a paper format or try an app like GI Monitor.
When youre planning your meals, forget about sticking to three squares. Eating large portions can overwhelm your already-sensitive digestive system. Instead, aim for smaller portions spread throughout the day instead of a few big meals. Downing your food too fast can also lead to discomfort, so eat slowly and mindfully and really concentrate on chewing your food thoroughlythat gives your gut a little extra help!
Maintain A Balanced Diet
Like many digestive disorders, what works for some may not work for others. It can be difficult to say exactly what should be avoided for each person. However, those in the know agree that if you are living with UC it is extremely important that you drink plenty of liquids and maintain a healthy, balanced diet.
You May Like: Signs Of Ulcerative Colitis In Child
Recommended Reading: Interesting Facts About Ulcerative Colitis
Tips For Preparing Nutritious Foods For Uc
Its one thing to know which foods are nutritious for you, but another to safely consume them. As one MyCrohnsAndColitisTeam member put it, The hard part is getting your nutritional requirements in with limited choices. Practicing meal planning and preparation techniques can be helpful to ensure adequate nutrition.
Members often share creative ways theyve found to incorporate nutritious foods into their diet safely. I made some pureed green sauce with greens, anchovies, garlic, and EVOO to add to roasted veggies and soups, said one. I have a Nutri Ninja. It purees my fruits and veggies, so I eat lots of smoothies with almond milk and Activia yogurt added, shared another.
It may also be helpful to purchase meal replacements, such as protein shakes, to keep your weight up. One member had a tip for weight gain: I increase the recipes that use lots of natural fats olive oil, coconut oil, coconut cream, avocado and I might increase my red meat. All of those make me feel super healthy.
During a flare, ulcerative colitis symptoms become more severe, and certain foods can worsen them further.
Following these guidelines can keep you away from the most common food triggers during UC flares:
Canned Or Cooked Seedless Skinless Vegetables And Fruits
As mentioned above, its important to avoid high-fiber fruits and vegetables during a flare-up. However, its still important to give your body the nutrients it needs. For this reason, youll want to make sure that you eat plenty of cooked or steamed fruits without skins or seeds. You can also safely eat pureed soups and sauces made from vegetables.
Also Check: 5 Asa Drugs Ulcerative Colitis
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Which Nutrients Are Important In Crohn’s And Colitis
Vitamins and minerals
Your body needs vitamins and minerals to work and stay healthy. Your Crohns or Colitis may stop you absorbing enough vitamins and minerals from your food. Vitamins and minerals that you may not absorb properly include iron, vitamin B12, vitamin D and calcium.Eating a healthy, balanced diet may help improve the level of vitamins and minerals in your body. If blood tests show you have low levels of vitamins and minerals, your doctor or specialist nurse may recommend you take supplements to restore your vitamin and mineral levels.Speak to your doctor, specialist nurse or dietitian if you think you may have low levels of any of these nutrients.
Iron
Having low levels of iron is common in people with Crohns or Colitis. Possible causes include a lack of iron in the diet, blood loss and problems absorbing iron from food. Lack of iron can lead to anaemia, where there are fewer red blood cells to carry oxygen around the body.Common symptoms of anaemia include:
Vitamin B12
Vitamin D
Calcium
Fibre
Its important to speak to a dietitian before cutting down on fibre so you dont miss out on the health benefits. For example, they may suggest that some people cut down on fibre for a short time during a flare-up, before slowly adding it back in to the diet.Fibre-rich foods include:
Recommended Reading: What Can Help Stomach Ulcers
Tips For Managing Ulcerative Colitis Symptoms
- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods boil, steam, grill, poach, broil or saute
Recommended Reading: What To Drink With Stomach Ulcer
Food Prep And Meal Planning
Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
Read Also: How To Cure Colon Ulcers
What To Eat During Remission
Increase fiber and reintroduce whole grains — Slowly incorporate foods higher in fiber when gastrointestinal symptoms lessen.
Consume omega-3 fatty acids — Consider eating more fresh or canned fatty fish or taking a fish or flaxseed oil supplement.
Focus on wholesome foods in their natural state — This includes foods with minimal processing and minimum ingredients.
Dairy and lactose products will be better tolerated — If you have a lactose intolerance, avoid dairy or eat low-lactose or lactose-free products.
Added fats will be better tolerated — Continue to focus on using oils, such as olive oil or canola oil, instead of solid fats.
Continue to focus on protein foods — Consume beef, eggs, poultry and other lean meats or plant-based proteins, such as soy products.
Be sure to drink plenty of water — Drink water instead of fruit juices, soft drinks, alcohol and caffeinated beverages such as coffee or tea.
Eat High Nutrient Foods
If you have IBD, you already know that processed convenience foods are not going to be the best choice for your diet. A better choice is foods that have a lot of nutrients in a smaller package. Foods that are considered nutrient-dense would be fruits and vegetables, beans, whole grains, dairy products, and nuts and seeds.
For those with IBD who find these specific foods problematic, other low-fiber choices include peanut butter, eggs, oatmeal, bananas, salmon, and tofu. The more whole your foods are, the more nutrient-dense your diet will be. Avoiding foods that come in bags or boxes is a good rule of thumb.
Read Also: What Is Best Medicine For Ulcer
Also Check: Extra Virgin Olive Oil And Ulcerative Colitis