Using Different Disease Indices
Increasing the threshold for quiescent disease to CRP < 10 mg/L according to ECCO guidelines resulted in 61 active and 52 patients in remission . Using these categories of active and IBD in remission, the prevalence of fatigue was not significantly different from the more conservative disease in remission definition.
Table 3.
Colon Cancer And Ulcerative Colitis
Long-term ulcerative colitis is associated with a risk of colon cancer. However, as treatments improve and it becomes more manageable to keep the inflammation caused by ulcerative colitis at bay, the risk has lowered. Regular colonoscopies with biopsies are usually recommended to keep watch for any changes in the cells of the colon.
Disease Course / Severity
Indicators of disease severity, measured as the need for steroids, immunosuppressors, biological agents or surgery and relapse rate, have not been extensively studied. Peeters et al found no significant agreement for the number of bowel resections in familial CD . Later, Annese et al showed a high concordance for the need for steroids , immunosuppressive drugs , and surgery and relapse rate in CD families, as well as a high concordance for the need for steroids and relapse rate in UC families. However, there were no differences between the observed and expected concordance rates of these clinical features . Likewise, Cabréet al were unable to demonstrate any relevant concordance for the severity items assessed in both CD and UC pairs: need for immunosuppressors biological agents , or surgery . In line with these results, a Danish population-based study found that having a family member undergoing surgery or receiving a tumor necrosis factor – inhibitor did not change the individuals own risk of surgery or of receiving TNF- inhibitors .
In summary, while there is unquestionable evidence that there is higher transmission of disease within families, and perhaps of disease type as well, family history per se is not a prognostic factor for disease phenotype or disease course.
Don’t Miss: Signs And Symptoms Of Diabetic Foot Ulcer
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Don’t Miss: How To Treat Venous Stasis Ulcers
Assessing The Risk Of Ibd When There Is A Positive Family History
Over the last decades, several studies have been conducted to predict the risk of developing IBD in relatives of an affected proband. The increased risk in relatives is difficult to quantify with precision, despite many published studies. The large variation can be explained by markedly heterogeneous methodologies and possible bias caused by differences in population selection, study design and ascertainment of diagnosis. Furthermore, different studies tend to use different estimates to report on risk .
A positive family history of IBD has been reported in 1.5-28% and 1.5-24% of CD and UC probands, respectively, highlighting the study variation . White populations have a higher prevalence of IBD family history compared to African American , Hispanic or Asian populations .
Ulcerative Colitis By Age And Gender
Ulcerative colitis occurs roughly equally in people of any sex. Some studies have shown slightly more males develop ulcerative colitis than females. However, the military health system study showed ulcerative colitis was slightly more common in females than in males.
Most people are diagnosed in their 20s and 30s, but ulcerative colitis can be diagnosed at any age, including in children and older adults. Overall, IBD in children tends to be more common in male children than in female children.
There is another peak in the diagnosis rates of ulcerative colitis in people over age 60. The median age of diagnosis of ulcerative colitis was shown to be 34.9 in one study.
The prevalence of ulcerative colitis increases with each decade of life. This means that ulcerative colitis is more common in people over age 50. Per 100,000 people, the prevalence of ulcerative colitis is estimated as:
- 80 and over: 348
Don’t Miss: What Causes Ulcers On Feet
Does The Risk Increase Or Decrease Depending On Which Family Member Is Affected
Yes. The risk of IBD depends on the exact relationship to the family member affected with the disease. Risk is higher if there are first-degree relatives affected, as compared to second-degree relatives. The highest risk is observed when both the mother and the father have IBD. In this rare situation, around 1/3 of the descendants will develop IBD.
Do Gender And Age Affect Your Risk Of Ulcerative Colitis
You can get UC at any age. But it most commonly starts when youâre between the ages of 15 and 30. After that, people ages 50-70 are most likely to develop it.
Research done in North America found that men were slightly more likely than women to be affected by UC. Men are also more likely to be diagnosed later in life, in their 50s and 60s.
Diagnoses in people over 65 are rising. Researchers think this is due both to increasing cases of UC and to an aging population. Between 25% and 35% of people with IBD are 60 or older and about 15% of them were diagnosed later in life.
Some research has found that older people are more likely to get surgery for their UC than younger people with the condition. Theyâre less likely to take immunomodulator medications . This may be because they have other conditions and take other medications that could interact with immunomodulators.
Don’t Miss: Good Foods To Eat With An Ulcer
Can I Go To Work With Colitis
A diagnosis of ulcerative colitis doesnt have to put the brakes on your career. Most people can continue to work. Although the condition, which inflames the colon, can make a typical workday more challenging, many people are able to stick with the same jobs they held prior to their colitis diagnosis.
Does Colitis Run In The Family
Asked by:Vernie Thompson DVM
The most common risk factors for ulcerative colitis include: Age: Ulcerative colitis usually begins before age 30 or people may develop UC at any age. Race or ethnicity:Caucasians have the highest risk of UC although anyone of any race can get it. People of Ashkenazi Jewish descent have an even higher risk of UC.
Also Check: What Are The Symptoms Of A Ulcerative Colitis Flare Up
Should You Stop Taking Your Ibd Medication
First of all, do not make any changes to your medication regimen without first talking to your doctor.
According to the ACG, keeping IBD well-controlled or in remission may help protect you from contracting COVID-19.
Right now the real hotspots for spread of this infection are in health care settings, says Dr. Ungaro. If your condition is well-controlled and you stop taking your usual medications, you risk having a flare. We do not want patients to have a flare in the midst of this pandemic and end up in the ER where they could be exposed .
If youre using steroids: Topical steroids, which are taken via suppositories or enemas, are unlikely to cause problems. Systemic steroids, however, are another story. If youre on oral steroids, now is a good time to start tapering off them if you can, says Dr. Ungaro, but do not stop taking steroids cold turkey. Call your gastroenterologist, discuss whether it is a good idea for you to start decreasing your dose, and find out how to do so slowly and safely.
If youre using aminosalicylates, biologics, or immunomodulators: If youre doing well on a drug in one of these classes, stick with it, says Dr. Morganstern. If you stop, youre at risk of flaring.
One exception, however, may be for patients who are stable and taking both an immunomodulator and a biologic. If someone is in remission on combination therapy, I might try removing the immunomodulator and keeping the biologic, says Dr. Morganstern.
Why Patients Stop Uc Treatment
People stop taking their ulcerative colitis medications for a number of reasons, says Phanijphand.
One of the leading reasons is the steep cost of the drugs. The out-of-pocket cost for prescription medicines can run over $2,000 per year, while the cost of UC care in general can run from roughly $15,000 to $25,000 per year, according to a study published in Inflammatory Bowel Diseases in January 2020.
The study also found that patients using biologics had the highest costs. Treating UC with corticosteroids had higher costs than with nonsteroidal anti-inflammatory drugs, but the latter groups costs rose more over time.
Also, when a person feels better, they may decide they no longer need UC medicine.
âSome patients think that once their symptoms are gone, they can stop taking their meds,â Phanijphand says. âThey believe theyâre cured or that they may have been misdiagnosed.â
Also Check: Reasons For Low Energy And Fatigue
Don’t Miss: Ulcerative Colitis And Hair Loss
What Happens During Ulcerative Colitis
The cause of ulcerative colitis, which is called pathophysiology, is not well understood. It’s thought that it may be connected to something causing the bacteria and other microbes that normally live in the colon to be out of balance, leading to an immune response and inflammation.
However, there is research underway that has started to uncover some of the reasons why people might develop the disease, including the following.
Who Has A Greater Risk Of Developing Ibd
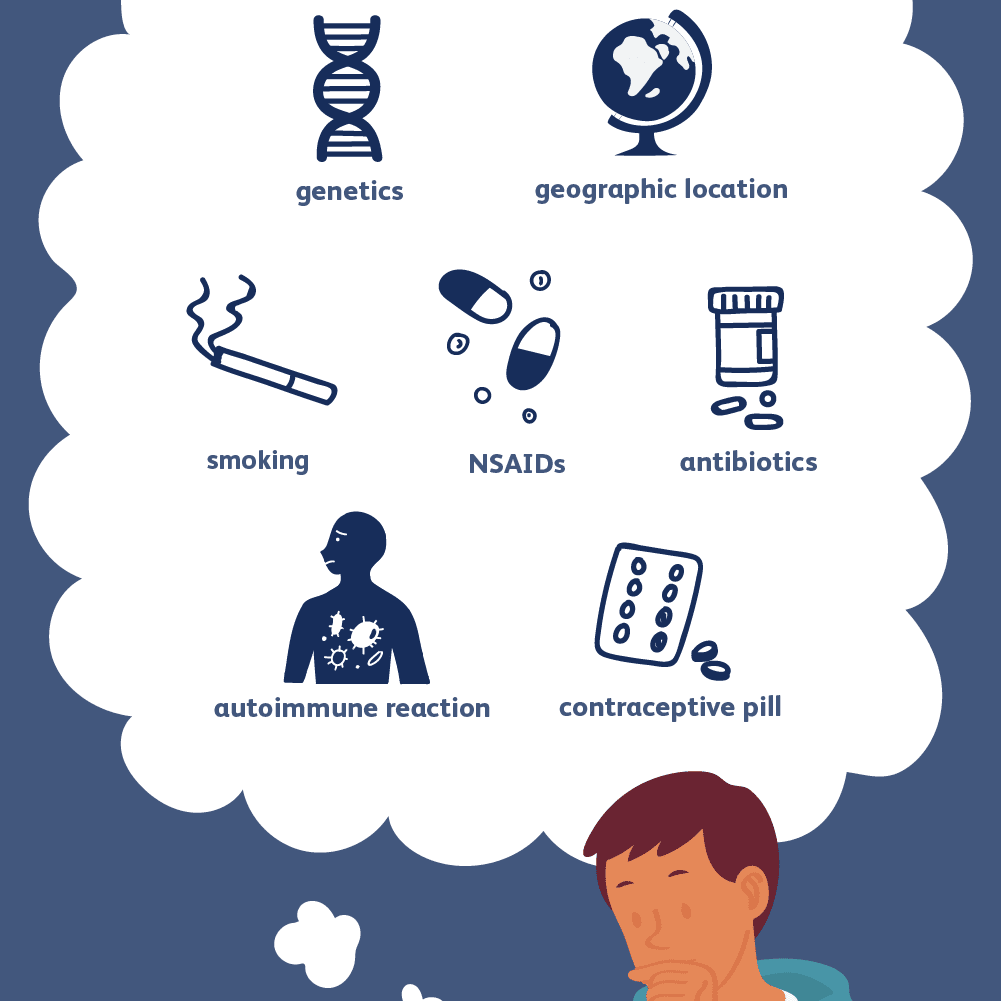
While inflammatory bowel disease is a perplexing group of diseases that tends to be difficult to diagnose and treat, researchers have collected a significant amount of information concerning the genetics, distribution, and contributing environmental factors for IBD. Overall, IBD affects people of all genetic backgrounds, but it seems to have a higher prevalence in western and developing countries. It also tends to be diagnosed most commonly in adolescents and young adults.
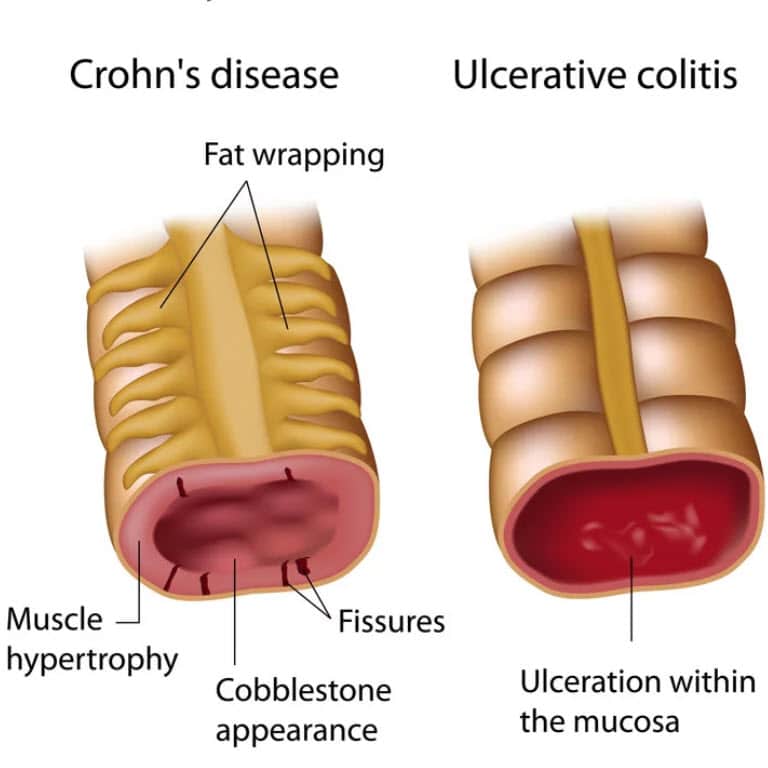
While Crohn’s disease and ulcerative colitis do appear to run in families, the connection is not always direct . The risk of inheriting is a complex process with many factors, influenced by both one’s genetic predisposition and environment.
Recommended Reading: Could I Have An Ulcer
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Crohns Disease And The Immune System
A persons immune system usually attacks and kills foreign invaders like bacteria, viruses, fungi, and other microorganisms. During a normal immune response, cells travel out of the blood to the intestines and produce inflammation. Under normal circumstances, harmless bacteria thats present in the GI tract are protected from an immune system attack.
Don’t Miss: What Foods To Eat If You Have An Ulcer
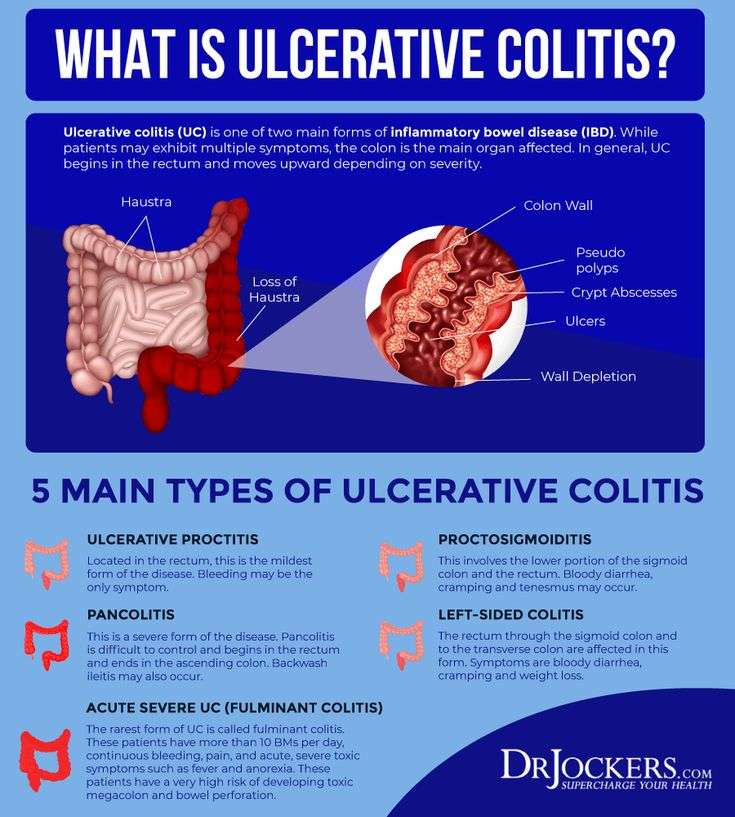
Where And How Does Ulcerative Colitis Start
Ulcerative colitis is an inflammatory bowel disease . This chronic digestive disorder is characterized by inflammation in the colon and the rectum. People diagnosed with ulcerative colitis can develop sores on the inside of their large intestine, which can lead to bleeding, diarrhea, and other symptoms.
If youve experienced these symptoms or have been diagnosed with ulcerative colitis, you may be unsure exactly how the disease began. Heres what you need to know about where in the body ulcerative colitis starts and how.
Important Safety Informationabout Entyvio
Please see the full Prescribing Information, including the Medication Guide, for ENTYVIO and talk with your healthcare provider.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call .
You May Like: Does Ulcer Pain Come And Go
How Can I Stop My Ulcerative Colitis From Bleeding
There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding. Anti-inflammatory medications for UC can include: 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
New Genetic Markers For Ulcerative Colitis Identified
- Date:
- University of Pittsburgh Schools of the Health Sciences
- Summary:
- Scientists have identified genetic markers associated with risk for ulcerative colitis. The findings bring researchers closer to understanding the biological pathways involved in the disease and may lead to the development of new treatments that specifically target them.
An international team led by University of Pittsburgh School of Medicine researchers has identified genetic markers associated with risk for ulcerative colitis. The findings, which appear today as an advance online publication of the journal Nature Genetics, bring researchers closer to understanding the biological pathways involved in the disease and may lead to the development of new treatments that specifically target them.
Ulcerative colitis is a chronic, relapsing disorder that causes inflammation and ulceration in the inner lining of the rectum and large intestine. The most common symptoms are diarrhea and abdominal pain. Ulcerative colitis and Crohn’s disease, another chronic gastrointestinal inflammatory disorder, are the two major forms of inflammatory bowel disease .
Story Source:
You May Like: What Are Ulcers In Horses
Why Do People With Crohn’s Or Uc React Differently To Gut Microorganisms
The current theory is that inflammatory bowel diseases like Crohns disease and ulcerative colitis develop when the immune system overreacts to the microorganisms in the digestive tract. White blood cells, whose job is to fight infection, travel to the intestine to fight harmless microorganisms. The white blood cells stay in the intestines and cause lasting inflammation.4,5
Researchers believe that inflammatory bowel disease is likely caused by a genetic predisposition combined with environmental factors and a dysfunction in the immune system, which is driven by the gut microbiota .4-7
Will My Child Inherit Ulcerative Colitis
UC runs in families. In fact, having a family history of UC is the biggest risk factor for the disease. Its likely that people inherit a genetic risk for UC. In addition, certain factors in their environment seem to play a role in their immune systems attack on their large intestine, setting off the disease.
You May Like: Medical Card For Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed In Children
Diagnosing ulcerative colitis begins with an examination and a detailed medical history. Your childs clinician will rule out other possible causes and may recommend one or more of the following tests:
Drug therapy can reduce inflammation and control symptoms. Ulcerative colitis medications may include:
- anti-inflammatory drugs, such as steroids, to bring the disease under control
- immune system suppressants that can reduce swelling
- antibiotics to treat related complications, such as abscesses or fistulas
- antiulcer/H2 blockers to treat related ulcers and irritation
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Don’t Miss: How Do Biologics Work For Ulcerative Colitis
Why Does Colitis Make You So Tired
Anaemia, a common complication of Crohns or Colitis, may worsen fatigue. People with anaemia carry less oxygen in their blood, which can mean they easily become exhausted. Low vitamin D levels may also contribute to fatigue. Vitamin D is important for keeping your bones, muscles and immune system healthy.