Assessment Of Dose Escalation
Dose escalation was defined differently for each biologic therapy, although the principle was the same. First, an induction period was calculated for each therapy, based on the labeled induction length, with an extra 1 week added for adalimumab and golimumab, and an extra 2 weeks added for infliximab and vedolizumab, to account for slight delays or variation in administration. Induction doses for adalimumab , golimumab , and vedolizumab were ignored for the purpose of calculating dose escalation . If the average dose during maintenance was at least 20% higher than the product label, this was considered dose escalation. For infliximab, since dosing is weight-based and weight was not available from the claims data, the index dose was used to derive an average daily baseline maintenance dose. This was calculated by dividing the total quantity administered at index by 56 . If this estimated average dose during maintenance was at least 20% higher than the index dose, this was considered dose escalation. For all medications, dose escalation was evaluated as the only persistent portion of the maintenance period because the gap might signal a treatment interruption.
The Pros And Cons Of Biologics For Ulcerative Colitis
The introduction of biologics has changed treatment for many people with ulcerative colitis. Heres what you need to know about the risks and benefits.
Andrew Brookes/Getty Images
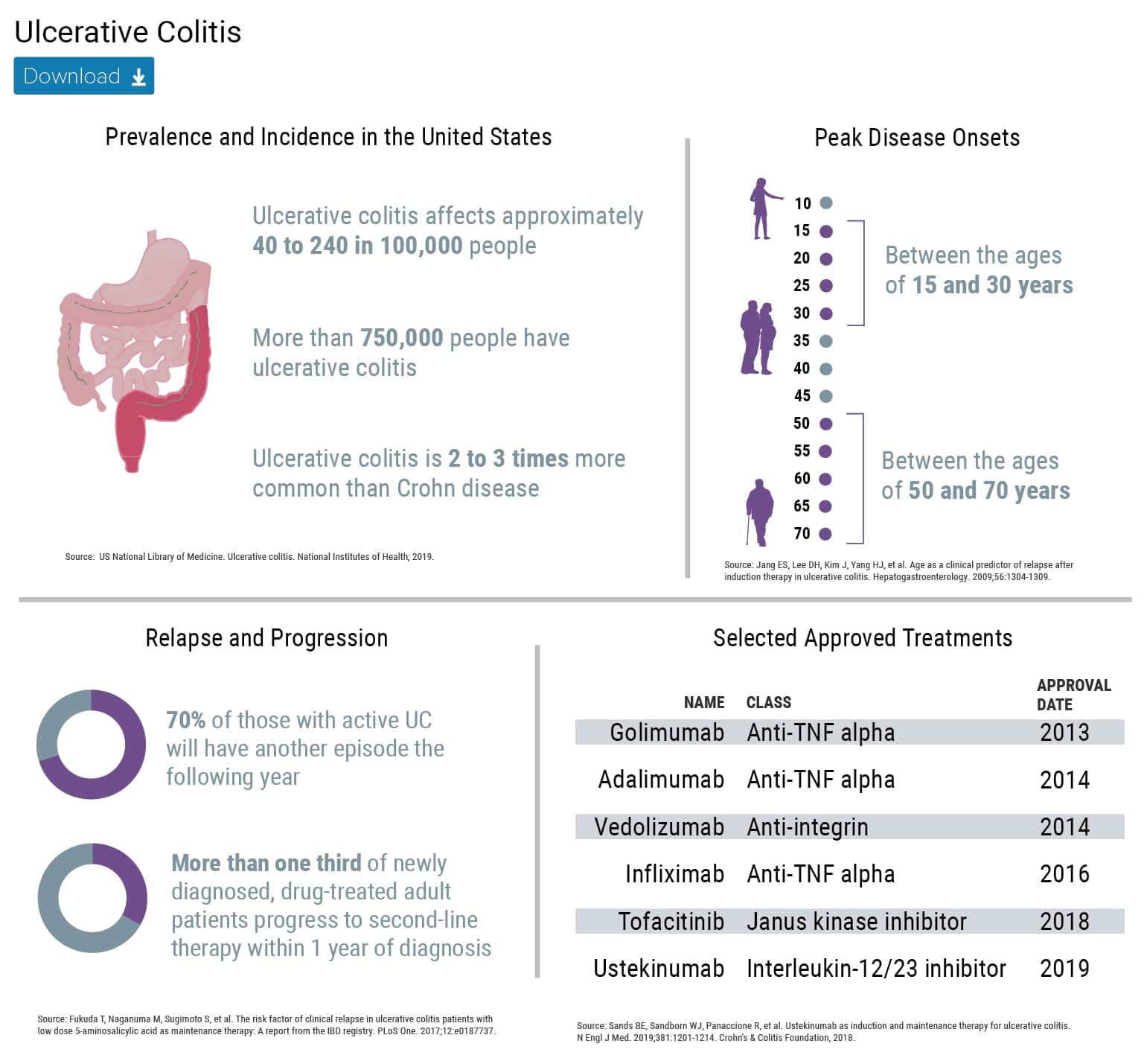
Over the past 15 years, treatment options for ulcerative colitis have expanded quite a bit. Among the newer options is a class of drugs called biologics.
Biologics are derived from natural sources, such as human or animal genes or microorganisms, and are designed to act on the immune system, specifically the parts that play key roles in fueling inflammation.
As inflammation is thought to be a cornerstone of the process involved in the manifestation of inflammatory bowel diseases, like Crohns disease and ulcerative colitis, they have proved to be very effective as treatment for certain patients, says Donald Tsynman, MD, a gastroenterologist at NewYork-Presbyterian Hospital in New York City.
The fact that biologics target the activity of the patients own immune system is what sets them apart from some other medications for ulcerative colitis, Dr. Tsynman says.
What Are The Potential Side Effects Or Complications
It’s true: There are some risks that come with taking biologics. But the fact of the matter is that all drugs come with some risks, and your GI is only likely to prescribe biologics if they think the positive impact will outweigh any potential side effects.
Before you begin, you’ll first be screened for tuberculosis and hepatitis B. That’s because certain biologics can reactivate dormant or latent versions of those infections.
Assuming you’re infection-free, it’s important to be aware of possible side effects and complications of biologic medications so that you can let your doc know ASAP if you experience any issues, according to CCF. Some more common side effects include headache, fever, chills, hives, and rashes. More rare issues include infection , arthritis, and a lupus-like reaction.
Very, very rarely, there have been reports of lymphomabut its unclear whether the risk is actually higher in people who take biologics compared with the normal population, according to one 2011 review.
Don’t Miss: Can Ulcerative Colitis Turn Into Crohn’s Disease
What Should I Tell My Doctor Before Starting Humira
Tell your doctor about all of your health conditions, including if you:
- Have an infection, are being treated for infection, or have symptoms of an infection
- Get a lot of infections or infections that keep coming back
- Have TB or have been in close contact with someone with TB, or were born in, lived in, or traveled where there is more risk for getting TB
- Live or have lived in an area where there is an increased risk for getting certain kinds of fungal infections, such as histoplasmosis, coccidioidomycosis, or blastomycosis. These infections may happen or become more severe if you use HUMIRA. Ask your doctor if you are unsure if you have lived in these areas
- Have or have had hepatitis B
- Are scheduled for major surgery
- Have or have had cancer
- Have numbness or tingling or a nervous system disease such as multiple sclerosis or Guillain-Barré syndrome
- Have or had heart failure
- Have recently received or are scheduled to receive a vaccine. HUMIRA patients may receive vaccines, except for live vaccines. Children should be brought up to date on all vaccines before starting HUMIRA
- Are allergic to rubber, latex, or any HUMIRA ingredients
- Are pregnant, planning to become pregnant, breastfeeding, or planning to breastfeed
- Have a baby and you were using HUMIRA during your pregnancy. Tell your babys doctor before your baby receives any vaccines
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with IBD and their loved ones. More than 159,000 members come together to ask questions, give advice, and share their stories with others who understand life with Crohn’s disease and ulcerative colitis.
Are you living with IBD and considering starting a biologic treatment? Share your experience in the comments below, or start a conversation by posting on your Activities page.
Recommended Reading: Sand Beds For Pressure Ulcers
The Future Of Biosimilars
As of December 2019, a total of 26 biosimilars have been approved in the United States. But that number could grow quickly, according to Anita Afzali, MD, a gastroenterologist and the medical director of The Ohio State University Inflammatory Bowel Disease Center in Columbus.
There are more than 650 biosimilars under development, Dr. Afzali notes, adding that most are in the early stages of development. Whats to come in the United States will certainly be a hot topic of discussion.
So far in the United States, biosimilars for IBD have been approved for all the same uses as their originator drugs but have not been ruled interchangeable with those drugs. In practice, this means that pharmacists cant substitute a biosimilar for a biologic, as they could with a generic for a brand-name drug.
Afzali worries that this may become a distinction without a difference. Its easy to imagine, she says, that an insurance company or hospital system could simply cover only the biosimilar equivalent of an original biologic. In this imagined scenario, she says, the state or the insurance or the pharmacist is saying, You have to try the biosimilar, even when a person has already experienced side effects from the biologic that might become worse with the biosimilar.
Treatment Loses Effect Over Time
Some people find treatment is effective to begin with, but this becomes less over time. This often happens because the immune system recognises the drug as a foreign substance and thinks it is harmful. It then produces proteins called antibodies against the biologic drug and these stop it from working as well.If this happens there may be a few options:
Increase the dose.
Add an immunosuppressant so that you would be taking a combination of medicines. There is evidence that this can reduce the levels of antibodies.
Change to a biologic that works in a different way.
Change to a different biologic that works in the same way.
Don’t Miss: Calcium Alginate For Pressure Ulcers
How Do You Know If Your Biologic Is Working
There are three major ways to evaluate whether a UC patient is responding and doing well on a biologic, says Dr. Nandi:
-
Clinical remission
-
Endoscopic remission
-
Steroid independence
“It’s not enough to be doing OK on a biologic. We want you to have clinical remission and endoscopic remission without steroid reliance,” says Dr. Nandi. Why the high bar? Well, healthy tissue means reduced symptoms and a lower cancer risk, which is already higher for people with IBD. And the main alternative to biologics is long-term steroid use, which is detrimental to the body.
It’s typical for some patients to feel dramatically better on a biologic medication, but still have active disease. “There has to be some kind of objective evidence that the inflammation is improving. If the patient isn’t taking steroids, feels great, and we can’t find evidence of inflammation via scope or imaging, then we know the biologic is working. This is known as deep remission,” says Dr. Nandi.
Some patients see improvement in just eight weeksothers take longer. It just depends on your body and how you react to the specific drug. But once the biologic is working, it’s typically administered indefinitely to keep the inflammation under control.
Dr. Nandi says he likes his patients to stay on the biologic for eight to 12 weeks to see if a clinical response occurs.
The Importance Of Balancing Other Risks
While medication risk is an important consideration that is well-recognized, it is important to recognize the higher risks of complications from poorlycontrolled disease activity, including fistula, stricture, and surgery. Notably, Osterman et al. showed that higher disease activity and corticosteroid use were associated with an increased risk of infection.95 Furthermore, the increased mortality risk associated with corticosteroids and narcotics has been well demonstrated.96-98 Lastly, recent studies have shown the 10-year risk of surgery is around 40% for CD99 and around 15% for UC.100 In patients with CD, the risk of developing an intestinal complication, such as fistula or stricture, is 50% within 20 years after diagnosis.101 Thus it is important to put the risks of medications into perspective with the high risks of poorly-controlled IBD.
Don’t Miss: How To Detect A Bleeding Ulcer
Follow Up With Your Doctor
You might need to try more than one biologic on your road to remission. Your doctor will tell you how to switch drugs safely. Biologics may not work very well when you start and stop treatment the wrong way.
Biologics can ease your symptoms for months or years. But over time, they may not work as well as they did at first. Thereâs no way to predict when or if this will happen. But you can tell your doctor anytime you have symptoms such as diarrhea or bleeding. Before they change your treatment, theyâll want to rule out infections or other stomach disorders that look like UC.
They can also run some tests to find out if youâre still responding to your biologic. If your medication stops working, your doctor may:
- Switch to a different kind of biologic
- Boost your dose
- Add another immunosuppressant
Your UC doctor will let you know how often you should come in for checkups. Be sure to keep up routine visits with your primary doctor, too. UC can occur alongside other health issues, so itâs a good idea to have more than one set of eyes on you.
Show Sources
Humira Pen And Other Forms
Humira comes in three forms: a prefilled pen, a prefilled syringe, and a vial of liquid solution. The drug is given as a subcutaneous injection. A healthcare professional can give you Humira injections. But you may be able to give yourself injections at home with the pen or syringe if your doctor approves. Youd need to be trained first.
Both the pens and syringes are prefilled with a single dose of Humira and come with needles. There are also special Humira starter packs available that contain several prefilled pens or syringes.
Humira also comes in a single-dose vial. But this form can only be used by healthcare professionals. You wont be able to use vials yourself.
If you have questions about which form of Humira is right for you or how to give yourself injections, talk with your doctor.
You May Like: 8 Foods To Eat During An Ulcerative Colitis Flare
Recommended Reading: Best Ulcer Prevention For Horses
Biologics May Be Used Along With Other Uc Medication
A biologic medication combined with a traditional ulcerative colitis drug may work better than either drug alone, Dr. Ullman says, but two biologics shouldnt be taken together because of an increased risk of complications.
Current guidelines also state that if you previously took a 5-ASA that wasnt successful, you shouldnt keep taking it if you move on to an anti-TNF drug, such as adalimumab or infliximab.
Interactions With Other Medications
Interactions between biologics and other medications can be significant, and each type of biologic drug can present different risks.
A doctor should be aware of all the over-the-counter or prescription medications, and all the supplements, herbal medications, and vitamins that a person takes before they prescribe a biologic.
Anyone using a biologic for UC should speak with a doctor before receiving a vaccine. For people who use certain biologic medications, including golimumab, infliximab, and adalimumab, having a live vaccine can be dangerous, and doctors recommend avoiding it.
$10,00030,000 per year on average, and the more expensive types can cost more than $500,000 annually.
Although many medical insurance plans may cover biologics, depending on a persons deductible, the cost can still be high.
A doctor may instead recommend a type of drug they call a biosimilar. There is very little clinical difference between these drugs and biologics. Biosimilars are less expensive but just as safe and effective.
The FDA approved the use of biosimilars in an effort to reduce costs. However, the FDA does not regulate whether insurance companies cover the costs of these drugs.
The following table provides an overview of biologics available to treat UC. The abbreviation IV stands for intravenous.
| Drug |
A range of biologic drugs can reduce UC symptoms in adults and help achieve remission. For children with moderate to severe UC, a doctor may prescribe infliximab.
Don’t Miss: What Pain Reliever Is Safe For Stomach Ulcer
What Makes Cura Different From Other Forms Of Curcumin
Unlike any available Curcumin on the market, we specifically use a non-absorbable formulation that reduces systemic exposure and increases curcumin concentration where its most needed: in the gut!
The formulation is designed to directly target and soothe inflammation in the intestinal mucosa, where IBD inflammation occurs. Our studies show this treatment to be highly effective for treating mild-to-moderate Ulcerative colitis.
Treating Moderate To Severe Ulcerative Colitis With Biologics
Treating ulcerative colitis has two main goals: helping to subdue your flare-up and maintaining it so you have fewer flare-ups. Biologics are among the newest drugs available for treating ulcerative colitis. They can be especially helpful for those who havent found relief yet.
Also Check: Why Do You Lose Weight With Ulcerative Colitis
You May Like: How Do You Get Ulcerative Colitis
Comparison With Acg Guidelines
Unlike the updated American College of Gastroenterology ulcerative colitis guidelines released in 2019, as reported by Medscape Medical News, the AGA clinical practice guidelines are not intended to cover all aspects of UC. Rather, explains Feuerstein, the guidelines are focused on providing the most thorough evidence-based answers to specific PICO questions based only on the GRADE assessment of the evidence.
The ACG guidelines, on the other hand, include recommendations for the diagnosis, medical management of the disease at all levels of severity, and quality of life, according to David T. Rubin, MD, FACG, from the University of Chicago, Illinois, who was lead author on the ACG guidelines. The two guidelines overlap around the use of biologic therapies and the choice of severity-based maintenance therapies in patients with moderate to severe disease to reduce the likelihood of future complications, he told Medscape Medical News. And although the ACG guidance does not specifically recommend early use of biologic agents over gradual step up after failure of 5-ASA therapy, Rubin acknowledges that large gaps in care with 5-ASA therapies indicate a clear need for better therapies.
Gastroenterology. Published online January 13, 2020. Full text
Humira For Crohns Disease
Humira is FDA-approved to treat moderate to severe Crohns disease in adults thats active. Active means that you have symptoms.
The goal of Humira is to ease the signs and symptoms of CD and help you reach remission, which is a time when you dont have symptoms.
CD explained
CD is a form of inflammatory bowel disease. CD can affect any part of your digestive tract, but it most commonly occurs in the small intestine and the large intestine . CD often causes symptoms such as diarrhea, stomach cramps, bloody stools, fatigue , weight loss, and frequent bowel movements.
Its believed that an overactive immune system is a factor in causing CD. Humira treats CD by blocking a protein called TNF. This decreases the activity of your immune system, leading to a reduction in the number and severity of CD symptoms.
Effectiveness for Crohns disease in adults
In adults with CD, Humira has been shown to be effective at causing and maintaining both remission and significantly easing CD symptoms.
In clinical studies, people with CD were treated with either Humira or a placebo. Researchers found that 21% to 36% of people who took Humira had a CD remission by week 4. This is compared with 7% to 12% of people who took a placebo.
Of the people who took Humira, 52% to 58% found that their CD symptoms eased significantly by week 4, compared with 34% of people who took a placebo.
Humira for Crohns disease in children
Recommended Reading: Herbal Medicine For Ulcerative Colitis
Read Also: How To Treat Peptic Ulcer Disease
A New Indication Of Success: Fda Approves Ozanimod For Ulcerative Colitis
The novel drug created at Scripps Research has achieved a second FDA approval, this time for ulcerative colitis, as clinical trials continue for Crohns disease.
May 27, 2021
LA JOLLA, CAOzanimod, the drug invented at Scripps Research that won FDA approval last year for relapsing forms of multiple sclerosis, has been approved in the United States for a second high-need medical condition, ulcerative colitis.
The once-daily oral drug, sold by Bristol Myers Squibb under the name Zeposia, can now be prescribed to treat adults with moderate to severe forms of the inflammatory bowel disease. Notably, its the first drug in a novel class of immune-modulating compounds to be approved for ulcerative colitis, which affects about 1 million people in the United States.
For patients with ulcerative colitis, this oral drug offers a better and more convenient option to control disease progression and improve quality of life, says Hugh Rosen, MD, PhD, who invented ozanimod along with fellow Scripps Research professor Edward Roberts, PhD, and their laboratory colleagues. The hope is that this will lead to fewer dangerous complications or serious infections than current treatment options, providing a steadier path for newly diagnosed patients as well as those failing other treatments.
Additional molecules developed by Rosen and Roberts at Scripps Research are currently in phase 2 clinical trials for major depressive disease and anxiety, and phase 1 studies for treatment of autism.