What Are The Basics Of A Healthy Diet For People With Uc
This whole UC situation would be a lot easier if it came with an instruction manual for eating. But even though were not quite as lucky as that, there are plenty of to help you along the way.
Case in point: Doctors and dietitians generally discourage people with UC from adopting fad diets like Keto or Paleo, which may do more harm than good because you may not get the nutrients you needor you may get too much of what you dont need. On the what-you-can-eat side, they generally recommend following a plant-based, Mediterranean diet . But what you eat during a flare and what you eat the rest of the time likely wont be exactly the same. Here are some things to keep in mind:
What Is Uc Again And Why Does Diet Matter
If youre reading about UC and diet, you probably have some of the basics already down but just in case this is all new to you: Ulcerative colitis causes chronic inflammation in the colon and rectum, triggering frequent and urgent diarrhea, bloody stools, and abdominal pain and cramping.
Its not just a poop problem though. It can lead to nutrient deficiencies, actual malnutrition, and weight loss along with body-wide inflammation, which can spur joint pain, fatigue, and more. And these are all issues that can be influenced for better or worse by what you eat .
Whats tricky, though, is that theres no specific ulcerative colitis diet.
In fact, there isnt even a set list of trigger foods that applies to every single person with UC.
Just like everyones specific set of is unique, so too are their problem foods. So, what the heck are you supposed to do with that? Find yourself a guide, thats what.
The best way to figure out how to make your diet work for your UC is to seek the advice of a registered dietitian. Ask your gastroenterologist if they can refer you to an R.D. they trust.
In the meantime, get up to speed on which foods do commonly worsen symptoms in people with UC, along with what goes into a healthy diet in general. While you cant manage UC with diet alone, arming yourself with this knowledge can be a key piece of the puzzle.
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
You May Like: What To Avoid Eating With Stomach Ulcer
The Best Diet For Ulcerative Colitis: Splitting Fact From Fiction
Many people claim to have cured ulcerative colitis with diet or supplements.
Unfortunately, there is no diet or pill that can cure the disease.
However, certain diet changes have shown tremendous promise in reducing symptoms and easing discomfort, helping patients live a normal life once more.
This article explains what we currently know about the role of diet in ulcerative colitis.
Contents
Also Check: Over The Counter For Ulcers
Even More On Low Fodmap
Foods to avoid include regular milk, wheat-based cereal and anything made with high-fructose corn syrup. “It can be a useful approach for dealing with gas, bloating or diarrhea.” In a study at Australia’s Monash University, 50% of UC patients following a low-FODMAP diet for three months improved their symptoms. Low FODMAP foods include kiwi fruit, cooked spinach, carrots, and peanut butter.
Recommended Reading: Can Stomach Ulcers Be Cancerous
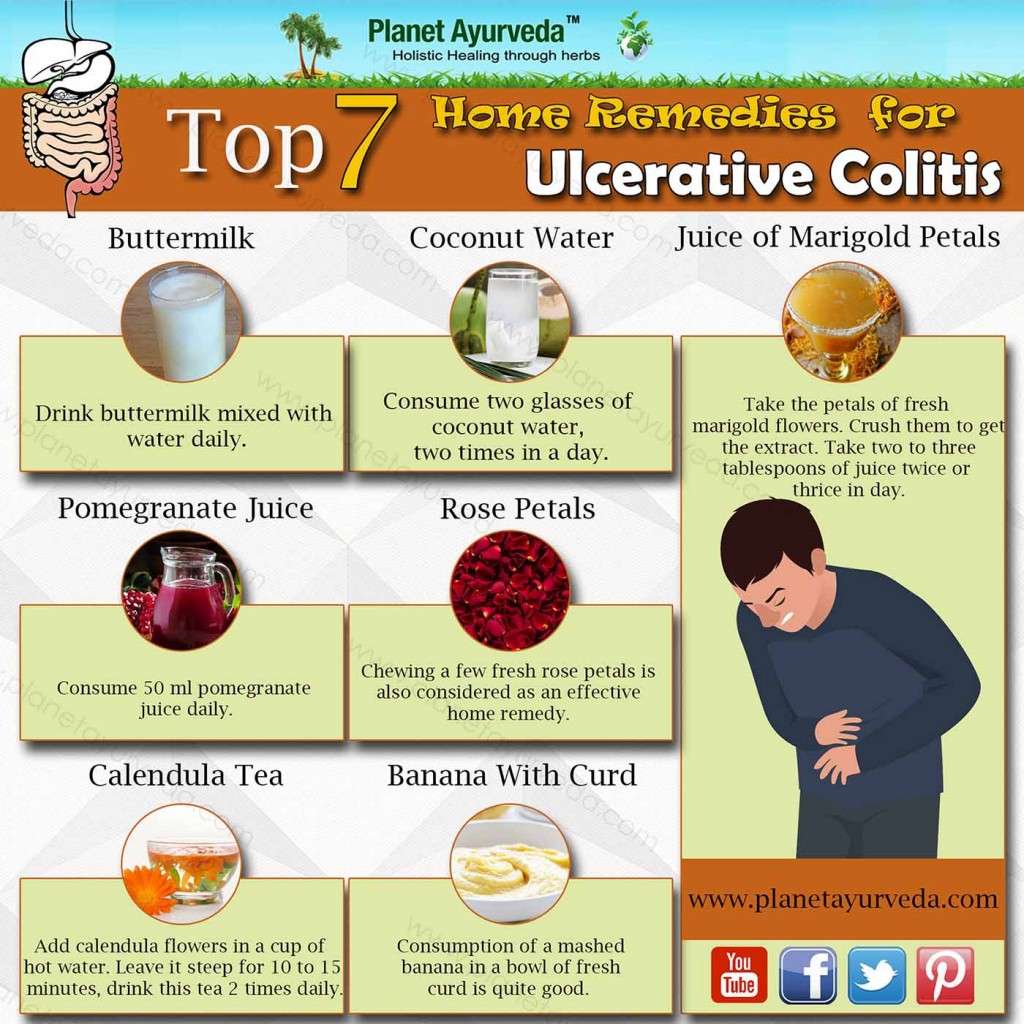
Ingredients To Avoid If You Have Uc
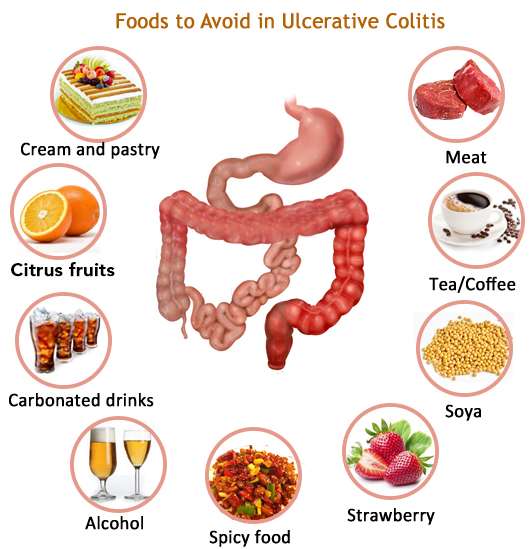
When you experience a UC flare-up, you should avoid foods that may worsen symptoms such as frequent bowel movements, diarrhea, bloody stools, and stomach pain, as well as fatigue, loss of appetite, and weight loss.
Limiting sugar is especially important during a time of active diarrhea, as sugar can make this worse, says Kennedy. Id recommend avoiding added sugars at all costs and switching to unsweetened applesauce instead.
If youre thinking about using artificial sweeteners, that may not be such a wise choice, either.
Artificial sweeteners are controversial, with some people feeling that they could possibly be a trigger food for those with IBD, Kennedy explains. It would be a personal choice to include them in a colitis-friendly diet.
Although the evidence is thin, a review published in September 2021 in the journal Frontiers in Nutrition, suggest that artificial sweeteners might trigger inflammation-causing changes to the gut bacteria, which could be problematic for people with conditions like IBD.
People with UC may also be more sensitive to gluten, a protein thats found in grains such as wheat, rye, and barley. The symptoms of gluten intolerance include bloating and diarrhea.
There isnt an ideal frequency for indulging in sweets, but moderation is key. When youre not dealing with a flare, Kennedy says you may be able to indulge a little, but the main goal is to try to limit the chances of triggering UC symptoms.
Lifestyle Diet In Inflammatory Bowel Disease
Topics in this Post
Inflammatory bowel disease, also known as IBD, consists of Crohn’s disease and ulcerative colitis. No specific food, diet or lifestyle causes, prevents or cures inflammatory bowel disease. And multiple factors can trigger the diagnosis.
Your diet does not cause inflammatory bowel disease, or induce a flare. However, modifying your diet can manage symptoms during a flare.
While several specialized diets may help certain patients, no plan has been proven to prevent or control inflammatory bowel disease, except for enteral nutrition, which is delivered in a nutrient-rich formula.
Keeping a food diary is a great way to manage flare-ups. A dietitian specializing in inflammatory bowel disease may recommend a particular diet based on your symptoms.
These tips may help you manage inflammatory bowel disease:
Be careful with vitamins and mineral supplements. Remember, most of your needed vitamins are obtained by eating a balanced diet. Some over-the-counter supplements can contain lactose, starch and other ingredients that can worsen your symptoms.
Besides eating a recommended diet, some supplements may be suggested for patients with inflammatory bowel disease. Talk to your health care professional about healthy levels of calcium, vitamin D, folic acid, vitamin B12, iron and zinc.
As with any health condition, a healthy lifestyle makes it easier to manage your diagnosis:
Topics in this Post
Recommended Reading: Best Treatment For Stage 3 Pressure Ulcer
Common Supplements Recommended For Ibd Patients
Your healthcare provider may recommend that you take vitamin or mineral supplements, especially if you are experiencing nutritional deficiencies. We can help you learn about supplements that are commonly recommended for IBD patients.
This information can help you learn which vitamins and minerals are important to maintain your nutrition, along with the various foods you may want to try as part of your IBD-friendly diet.
Your body is unique. What works for one patient, will not work for everyone. Check with your healthcare providers before starting any supplements, as you will need proper dosing.
Preparing For An Appointment
Symptoms of ulcerative colitis may first prompt you to visit your primary care doctor. Your doctor may recommend you see a specialist who treats digestive diseases .
Because appointments can be brief, and theres often a lot of information to discuss, its a good idea to be well prepared. Heres some information to help you get ready, and what to expect from your doctor.
Read Also: Best Way To Treat Mouth Ulcers
Whole Grain Breads Cereals And Pastas
Whole grain flour is high in fiber because it hasnt had the germ or bran removed.
Its important to avoid eating food made from any whole grain flour, such as:
, including beans, lentils, and peas, are high fiber, high protein foods. Because of the indigestible sugars in beans, theyre also notorious for causing gas. If you are experiencing a UC flare-up, youll want to pass on the following:
- all beans, including chickpeas
- soy nuts, including soybeans and edamame
Can Food Cause Crohns Or Colitis
We dont know what causes Crohns and Colitis but we do know that a combination of the following factors are likely to play a part:
- A problem with the immune system, where the body attacks its own cells
- Changes in the bacteria in the gut.
These, together with environmental factors, like food and stress, may trigger the conditions.There isnt any clear evidence that specific foods cause Crohns or Colitis. Some researchers think a diet low in fruit and vegetables may increase the risk of Crohns and a low intake of vegetables may increase the risk of Colitis for some people. Theres also some evidence that eating a lot of meat or table sugar, called sucrose, may increase the risk of Crohns and Colitis. But there isnt enough evidence yet to say for certain whether food affects the risk.
Dont Miss: Can You Eat Pizza With Ulcerative Colitis
Recommended Reading: Allopurinol And Azathioprine For Ulcerative Colitis
Chronic Inflammatory Bowel Disease The Telltale Symptoms
Symptoms also include fatigue, which manifests itself as severe tiredness with no cause and has a profound impact on the patients personal, social and working life.
Joint, skin, eye and liver problems can also be associated with these diseases: these are immune-mediated extra-intestinal manifestations, which in some cases can even anticipate the typical symptoms of the disease by a few years.
Diet Recommendations For Crohns Disease Flare
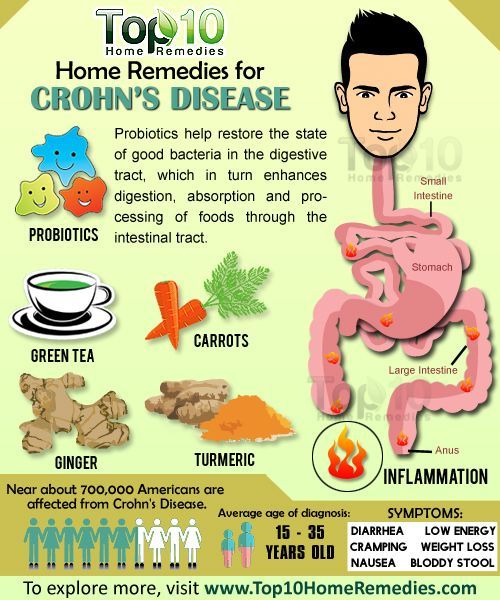
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
You May Like: Ulcerative Colitis And Canker Sores
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Is Ulcerative Colitis And Autoimmune Condition
We are frequently asked whether Ulcerative Colitis it is an autoimmune condition. The short answer is yes, but its most important to understand what that means for your treatment plan.
With Ulcerative Colitis, the body recognizes harmless gut bacteria as an enemy and attacks the tissues in the colon. In a typical immune response, the body will send white blood cells to the area of illness or infection to help protect the body. After the body has combated the illness or infection, the inflammation will resolve.
However, in a colon affected by UC, the body continues to send white blood cells to the inner layer of the large intestine, which accumulate and continue to attack. This process causes a buildup of inflammation and can lead to sores, or ulcers, in the affected area. Because UC is recognized as an autoimmune condition, the treatment methods generally target the immune response within your body.
Medical Treatments for Ulcerative Colitis include:
Read our full discussion of Ulcerative Colitis autoimmune treatment options here.
You May Like: Is Coconut Good For Ulcerative Colitis
Where Can The Best Product Be Purchased From
We will review some of the best ways to buy products from an online store. A few different steps are involved in purchasing a product, and each one is important to ensure you get what you want.
First of all, make sure that your desired product has been released. It can be checked by checking the website’s release date page or clicking on new arrivals.
Next, read reviews about the products before purchasing them not only does reading reviews help with making informed decisions, but it also helps other shoppers who might be looking for feedback! Finally, when ordering something, order two sizes up if no size chart is provided because sizing charts vary between brands.
Pita Chips And Hummus
Hummus is made with mashed chickpeas, olive oil, and other seasonings.
The Crohns and Colitis Foundation recommend 1/4 cup of hummus and 2 ounces of pita chips as a snack.
To make hummus at home, a person can blend chickpeas, tahini, and a little olive oil together. They can add seasoning to taste but should avoid adding too much salt.
Even though it is high in fiber, pita chips and hummus can be a generally well-tolerated snack or small meal. The chickpeas in hummus may help symptoms in a person experiencing gas or bloating.
Read Also: Draw Sheets Are Used To Prevent Pressure Ulcers
Main Difference Colitis Vs Ulcerative Colitis
Colitis and ulcerative colitis are two medical conditions which affect the colon. These two terms often used interchangeably since they share similar signs and symptoms. But, it is important to distinguish the difference between them in order to make an accurate diagnosis and treatment. The main difference between colitis and ulcerative colitis is that ulcerative colitis is one form of colitis which results in the chronic inflammation of colonic mucosa and rectum giving rise to ulceration and bleeding.
1. What is Colitis ? Causes, Signs and Symptoms, Diagnosis, and Treatment
2. What is Ulcerative Colitis? Causes, Signs and Symptoms, Diagnosis, and Treatment
3. What is the difference between Colitis and Ulcerative Colitis?
Dont Miss: Best Dressing For Venous Stasis Ulcer
Create A Plan That Works For You
If you have UC, informed dietary choices can make a big difference. Nutrition takes on special importance, especially since the disease can make it harder for your body to absorb calorie and nutrients. Choosing nutrient-rich foods is important.
Avoiding trigger foods is also key. They can make your symptoms worse. They can even keep your body from properly absorbing calories and nutrients from the foods you eat.
New research in mice shows that emulsifiers in processed foods like lecithin, polysorbate, and gums, weaken the intestinal mucous lining and negatively alter gut bacteria. This can potentially lead to more intestinal inflammation, flare-ups, and symptoms. More research is necessary to confirm these findings in humans, but the research findings are compelling enough for those with inflammatory bowel disease to consider reducing how much processed foods they eat.
For these reasons and more, a well-balanced diet is important. It can help minimize your symptoms and lower your risk of complications from UC.
Recommended Reading: New Biologic Drugs For Ulcerative Colitis
Ulcerative Colitis Diet: What To Avoid In A Flare Up
A study in the journal of Advances in Nutrition found that a high fat diet can increase intestinal permeability, something that is already a problem for those with ulcerative colitis. A review in the Mediators of Inflammation journal indicates that the upset caused to the gut wall by ulcerative colitis may also increase intestinal permeability and as such, reducing foods that also impact intestinal permeability, particularly during a flare up, is advisable.
A spokesperson from Crohns & Colitis UK explains that there is no one-size-fits-all approach to eating while in a flare up.
No particular diet has been proven to help people with ulcerative colitis, they say. Some people find that certain foods trigger symptoms or flare-ups but others do not. Everyone is different and what works for one person may not work for another. Theres no single diet that works for everyone. While changing your diet can help you manage your symptoms, it does not replace medical treatment. Its important not to make any changes to your diet without speaking to your IBD team or dietitian first.
Uc And Lactose Intolerance
People with UC often think they have lactose intolerance, which means they cant properly digest the sugar in milk and milk products, because some symptoms are similar. But UC doesnât make you more likely to have lactose intolerance. Your doctor can do a simple test to find out.
If you can, keep milk and dairy products in your diet. They are a very good source of calcium and vitamin D, which keep your bones healthy. Using steroids such as prednisone for a long time can thin your bones and make it harder for your body to absorb calcium, raising your chance of having osteoporosis.
If dairy products cause you discomfort, see if you can eat them in small amounts. Or try a lactase supplement to break down the lactose in dairy products.
If you just cant stomach dairy products, your doctor may want you to take calcium and vitamin D supplements. Watch a video on how dairy affects ulcerative colitis.
You May Like: Can Tylenol Cause Stomach Ulcers
You May Like: Treating Ulcers In Horses With Omeprazole
Will Ulcerative Colitis Affect My Stool
Changes in bowel movements are one of the key markers of Ulcerative Colitis. UC stool shape, color, and smell can be quite different than your average bowel movement. If you have Ulcerative Colitis, your immune system essentially attacks healthy cells in your digestive tract, which causes inflammation in your colon and rectum. Below are some key indicators that you may have Ulcerative Colitis based on your stool.
- Color: You might notice bright red, maroon or black color indicating the presence of blood. You may also notice more mucus in the stool than normal.
- Odor: The odor of the stool may be increasingly foul compared to the typical smell.
- Texture: Presence of UC typically causes loose, watery stools. In reference to the Bristol stool chart, UC stool texture will most likely resemble types 5 through 7.
- Frequency: Inflammation can cause increased motility and frequency of bowel movements. Many people experience frequent urgency and diarrhea.
- Effort: People with UC may experience burning or painful stools.
Always consult your primary care doctor. They can refer you to a local GI specialist if needed
If diagnosed, you may want to seek a specialist for your specific disease in your area