Symptoms Of Inflammatory Bowel Disease
Symptoms of inflammatory bowel disease may range from mild to severe, with periods of active illness followed by periods of remission. Common signs of both Crohn’s disease and ulcerative colitis include:
- Diarrhea: Loose stools are one of one of the most common symptoms of IBD.
- Fever and fatigue: Many people with IBD experience a low-grade fever. You may also feel tired or have low energy.
- Abdominal pain and cramping: Inflammation and ulceration can affect the normal movement of contents through your digestive tract and may lead to pain and cramping. You may also experience nausea and vomiting.
- Blood in your stool: You might notice bright red blood in the toilet bowl or darker blood mixed with your stool. You can also have bleeding you don’t see .
- Reduced appetite: Abdominal pain and cramping, as well as inflammation, can affect your appetite.
- Unintended weight loss: You may lose weight and even become malnourished because you cannot properly digest and absorb food.
What Causes Ulcerative Colitis
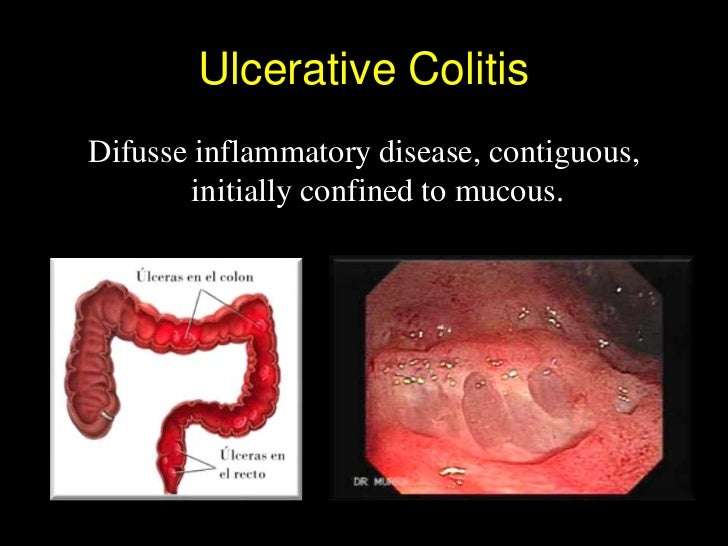
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders. White blood cells that usually protect you attack the lining of your colon instead. They cause the inflammation and ulcers.
Doctors arenât sure why people get the condition. Your genes may play a role the disease sometimes runs in families. Other things in the world around you may make a difference, too.
Things that can affect your risk of getting ulcerative colitis include:
- Age. Itâs most likely if youâre between 15 and 30 years old or older than 60.
- Ethnicity. The risk is highest in people of Ashkenazi Jewish descent.
- Family history. Your risk could be up to 30% higher if you have a close relative with the condition.
Food and stress donât cause it, but they can trigger a flare of symptoms.
Don’t Miss: Is Omeprazole Good For Ulcers
How Are Night Sweats Evaluated
Your health care provider may do blood tests to check for an increase in inflammation. Increased inflammation could be a sign of a IBD flare, but can also indicate other conditions that cause night sweats.8
It is possible that your provider will order additional tests to rule out some of the common causes of night sweats, such as tuberculosis or HIV infection. Based on your history and other symptoms, your provider may choose to do additional tests.
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
You May Like: Compression Therapy For Venous Leg Ulcers
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
During surgery, your small intestine will either be diverted out of an opening in your abdomen or be used to create an internal pouch that’s connected to your anus called an ileoanal pouch.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Also Check: Ulcerative Colitis Colon Cancer Screening
Are There Different Types Of Uc
When you get diagnosed with UC, your gastroenterologist may tell you that you have a certain type of UC. There are a few different subtypes, and each can have slightly different symptoms. Heres a breakdown.
-
Ulcerative proctitis. In this type of UC, the inflammation is confined to the rectum, rather than both the rectum and the colon. Symptoms of this type of UC include rectal pain and bleeding and a sense of urgency to have bowel movements.
-
Left-sided colitis. In left-sided colitis, inflammation can extend from the rectum to the splenic flexure, a bend in the colon near your spleen. Another type of UC called proctosigmoiditis also falls under the umbrella of left-sided colitis, and it affects your rectum and the sigmoid colon, which is the lower part of your colon. Symptoms of these types of UC include bloody diarrhea, weight loss, reduced appetite, and pain on the left side of your abdomen.
-
Extensive colitis. This type of UC involves usually inflammation involving the entire colon is called pancolitis. Symptoms include bloody diarrhea, abdominal pain, weight loss, and reduced appetite.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Recommended Reading: Can Ulcers Cause Black Stool
When To Call Your Doctor
If youre having any of the above UC symptoms, especially bloody stool, endless diarrhea, or severe pain, make an appointment with your primary-care doctor. It could always be something other than UC, but its important to get it checked out.
The sooner you treat UC and work to stop the damage to your intestinal lining and overall health, the better. If your GP suspects UC, they will likely refer you to a gastroenterologist, which is a type of physician specializing in digestive health care. This doc can further evaluate your symptoms, run any necessary tests, and get you a diagnosis.
If youve already been diagnosed with UC, call your gastro if youre experiencing any increase in symptoms like bloody stools, diarrhea, and pain, along with weight loss, fatigue, and fever.
And we totally get it. Talking about UC symptoms with your doctoror anyone!can feel awkward or embarrassing . But its hugely important that youre honest about whats going on so your doctor can get you the best treatment possible.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Also Check: What Makes Ulcerative Colitis Worse
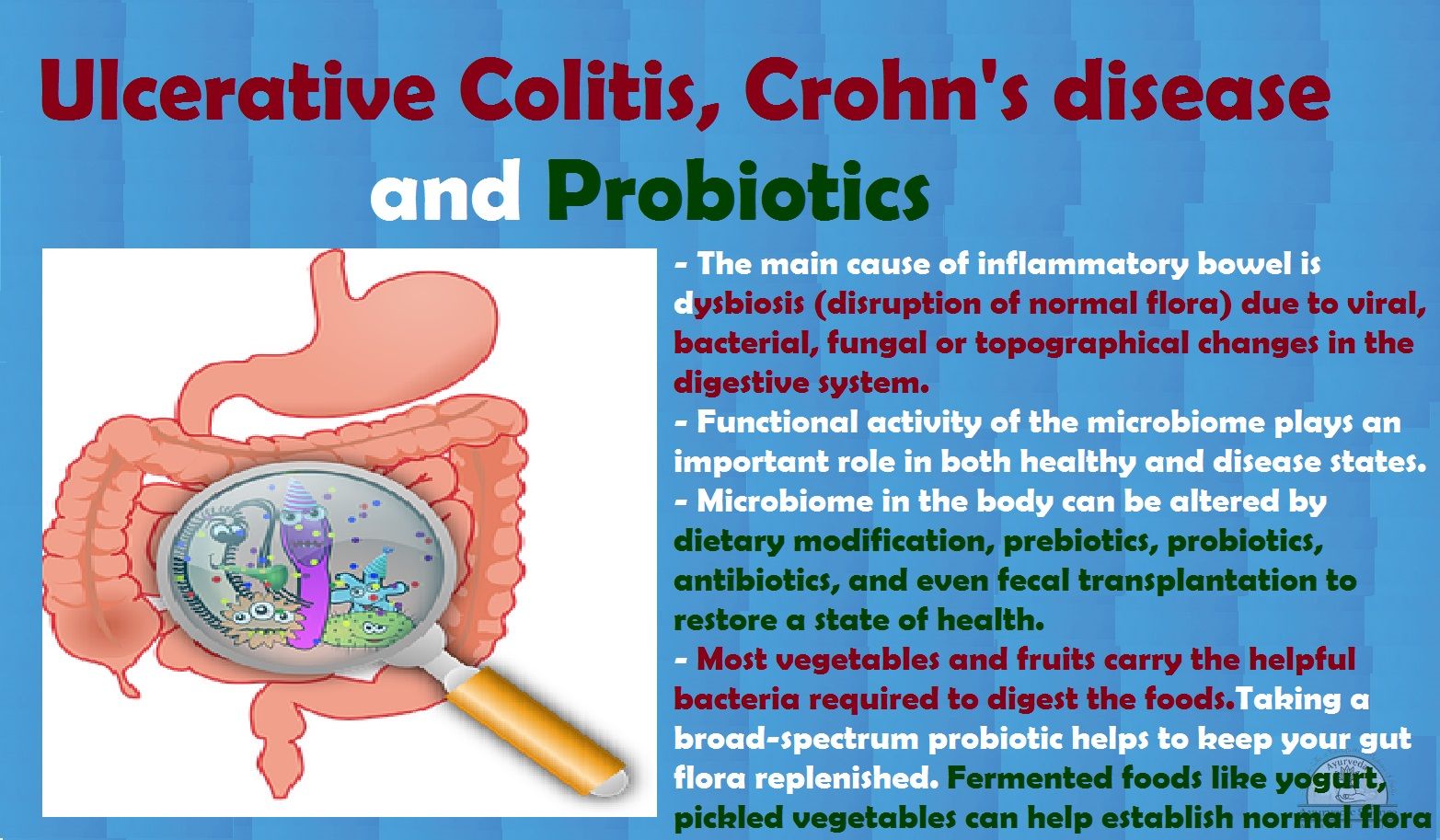
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Read Also: What Foods Can You Eat When You Have An Ulcer
What Can I Expect If Symptoms Return
Itâs important to know your body when you have a long-term illness like UC, where symptoms come and go. Understand yours and keep them on your radar. Maybe youâre having more bowel movements than normal, or youâre in more pain. Other signs include:
- Diarrhea with blood or pus
- Stomach pain and cramping
- Pain or bleeding in your rectum
- Strong urge to have a bowel movement
- Trouble having a bowel movement
- Weight loss
- Extreme tiredness
- Fever
âThese are the early flashing red lights on your dashboard that should get you talking to your doctor,â Iroku says.
The things that aggravate your condition — certain foods or medicines — can change over time. As you get older, your body, including your GI system, may be more sensitive to irritation.
You and your doctor can also work together to figure out if your symptoms are truly a UC flare or the sign of something else, like irritable bowel syndrome, an infection, or a side effect of medication.
One of the best predictors of a future UC flare is whether youâre having one right now. If you have active ulcerative colitis this year, your odds of a flare next year are around 70%. This also means if youâre in remission today, your chances of staying symptom-free also rise.
Quitting smoking, staying active, lowering stress, and avoiding trigger foods will help keep your symptoms at bay for longer.
Show Sources
Feeling Chills And Ibd
| | |
Not every symptom of Crohns disease and ulcerative colitis is gastrointestinal that is, related to the digestive system. Some common symptoms are extraintestinal, meaning they affect other parts of the body. In addition to abdominal pain, cramping, bloating, diarrhea, and weight loss, people with inflammatory bowel disease can experience chills.
Fever and chills can have a variety of causes in people with Crohns or UC. They could be due to a drug allergy, or they may be a sign your IBD is becoming more severe. People on treatments that affect the immune system, like biologics, need to be aware of the reasons fevers can occur while taking these medications.
Its important to contact your doctor if youre experiencing fever and chills, especially if the symptoms intensify over time.
Don’t Miss: Best Medicine For Stomach Ulcer Pain
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
- low energy
- weight loss
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
You May Like: Are Fermented Foods Good For Ulcerative Colitis
Classifications Of Ulcerative Colitis And Their Symptoms
- Ulcerative proctitis: Inflammation is confined to the area closest to the anus . For some people rectal bleeding may be the only sign of the disease. Others may have rectal pain and a feeling of urgency . This form tends to be the mildest.
- Proctosigmoiditis: Involves the rectum and the lower end of the colon, known as the sigmoid colon. Bloody diarrhea, abdominal cramps and pain.
- Left-sided colitis: Inflammation extends from the rectum up through the sigmoid and descending colon, which are located in the upper left part of the abdomen. Bloody diarrhea, abdominal cramping and pain on the left side and unintentional weight loss.
- Pancolitis: Affects more than the left colon and often the entire colon. Bloody diarrhea that may be severe, abdominal cramps and pain, fatigue and significant weight loss
- Fulminant colitis: A rare, life-threatening form of colitis affects the entire colon and causes severe pain, profuse diarrhea and, sometimes, dehydration and shock. People with this condition are a risk of serious complications, including colon rupture and toxic megacolon, a condition that causes the colon to rapidly expand.
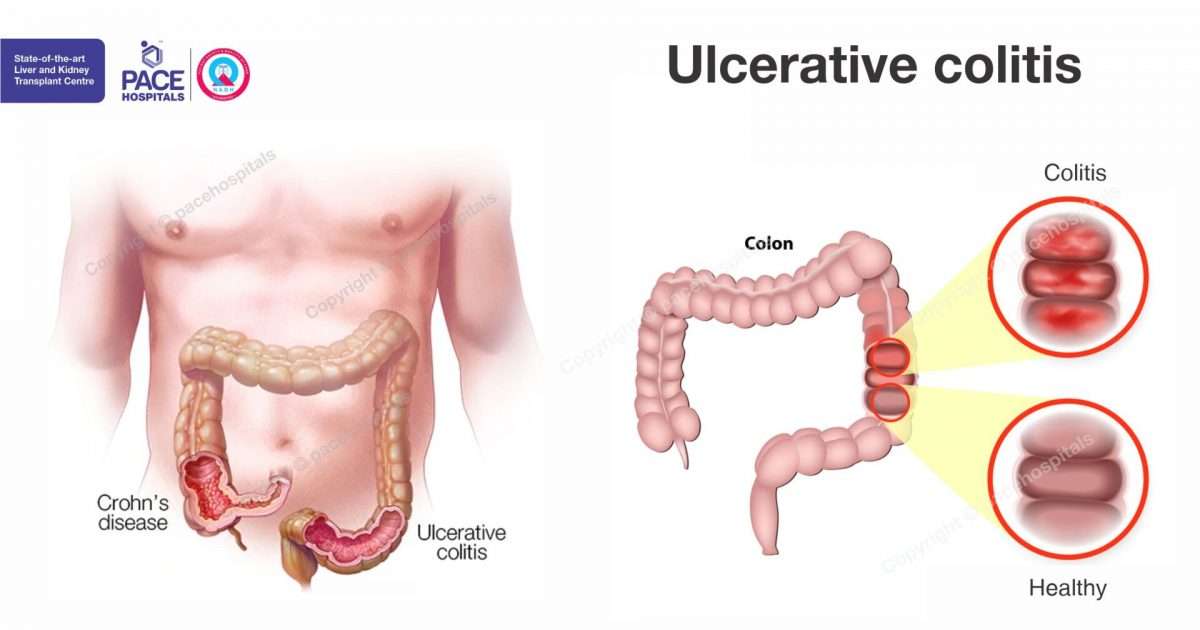
What Is Ulcerative Colitis
Ulcerative colitis is a condition that causes the inner lining of the large intestine to get red and swollen with sores called ulcers. It’s a chronic condition, which means it lasts a long time or constantly comes and goes.
Ulcerative colitis is a type of inflammatory bowel disease that happens only in the colon.
You May Like: Quantitative Research On Pressure Ulcer Prevention
Work With Your Doctor
You’ll need to see your UC doctor regularly. It may be every 6 months while you’re in remission. You’ll have routine procedures like colonoscopies and bloodwork to check on your UC.
If you’re having a flare-up, make sure to check in with your doctor. UC isn’t the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Can’t keep liquids down
When you have a flare, you can ask your doctor questions like these:
- Is UC causing my symptoms, or could they be due to another condition?
- Do I need to take any tests? If so, how often will I need to get them?
- Will you need to change the dose or type of my medication?
- If I need to take a new medication, what side effects could it cause?
- Should I make any lifestyle changes?
- When should I come back for another appointment?
Can Uc Go Into Remission
Ulcerative colitis is what experts call a relapsing and remitting disease. This means symptoms come and go over time. There may be months or even years when you wonât have any symptoms at all.
Thereâs no single definition of what it means to be in remission with UC. Your doctor could say itâs the balance between managing your symptoms and any side effects of treatment. But a better overall quality of life may be whatâs most important to you, like enjoying a symptom-free social life.
Depending on how itâs measured, around half of Americans with UC are in remission, says Ugo Iroku, MD, a board-certified gastroenterologist at New York Gastroenterology Associates. The other half have symptoms that range from mild to serious.
In general, there are three types of UC remission:
- Clinical remission. This is the most basic type of remission — no belly pain, diarrhea, or blood in your stool.
- Endoscopic remission. If youâre symptom-free and thereâs no inflammation of your bowels, youâre probably in endoscopic remission. Your doctor will look for inflammation during a colonoscopy, an exam that uses a tiny camera attached to a thin, bendable tube.
- Deep remission. This is the most robust level of remission. Doctors look for three things: no symptoms, inflammation, or sign of UC at a cellular level under a microscope.
Read Also: Ulcerative Colitis And Mental Health