Comparing Crohns Disease And Diverticulitis Signs And Symptoms
Crohns disease symptoms include diarrhea, fever and fatigue, abdominal pain and cramping, blood in stool, mouth sores, reduced appetite and weight loss, drainage near the anus due to fistula, inflammation of the skin, eyes, and joints, inflammation of the liver and bile ducts, and delayed growth or sexual developing in children.
Signs and symptoms of diverticulitis include severe pain that may last for days and takes place in the lower left side of the abdomen, nausea and vomiting, fever, abdominal tenderness, constipation, and in some cases diarrhea .
Diagnostic Focus And Assessment
The laboratory tests performed on the first day of admission revealed leukocytosis with neutrophilia , thrombocytosis , anemia , elevated inflammatory biomarkers , and low serum urea levels . The abdominal ultrasound examination was normal. Lower digestive endoscopy pointed out multiple ulcerations, hemorrhage, and edema of the sigmoid colon , thus suggesting a possible IBD however multiple orifices raised the suspicion of a CD, which was afterwards confirmed through a barium enema.
Figure 1. Initial aspect of the colon at colonoscopy.
Histopathological examination of the colonic biopsy specimens showed active inflammation associated with architectural changes of the colonic mucosa and crypt abscesses, which highly suggested a chronic inflammatory process, most likely UC. By taking into account the macroscopic aspect of the colonic mucosa and the histopathological results correlated with the presence of colonic diverticula, we were able to establish the diagnosis of SCAD.
Main Difference Colitis Vs Ulcerative Colitis
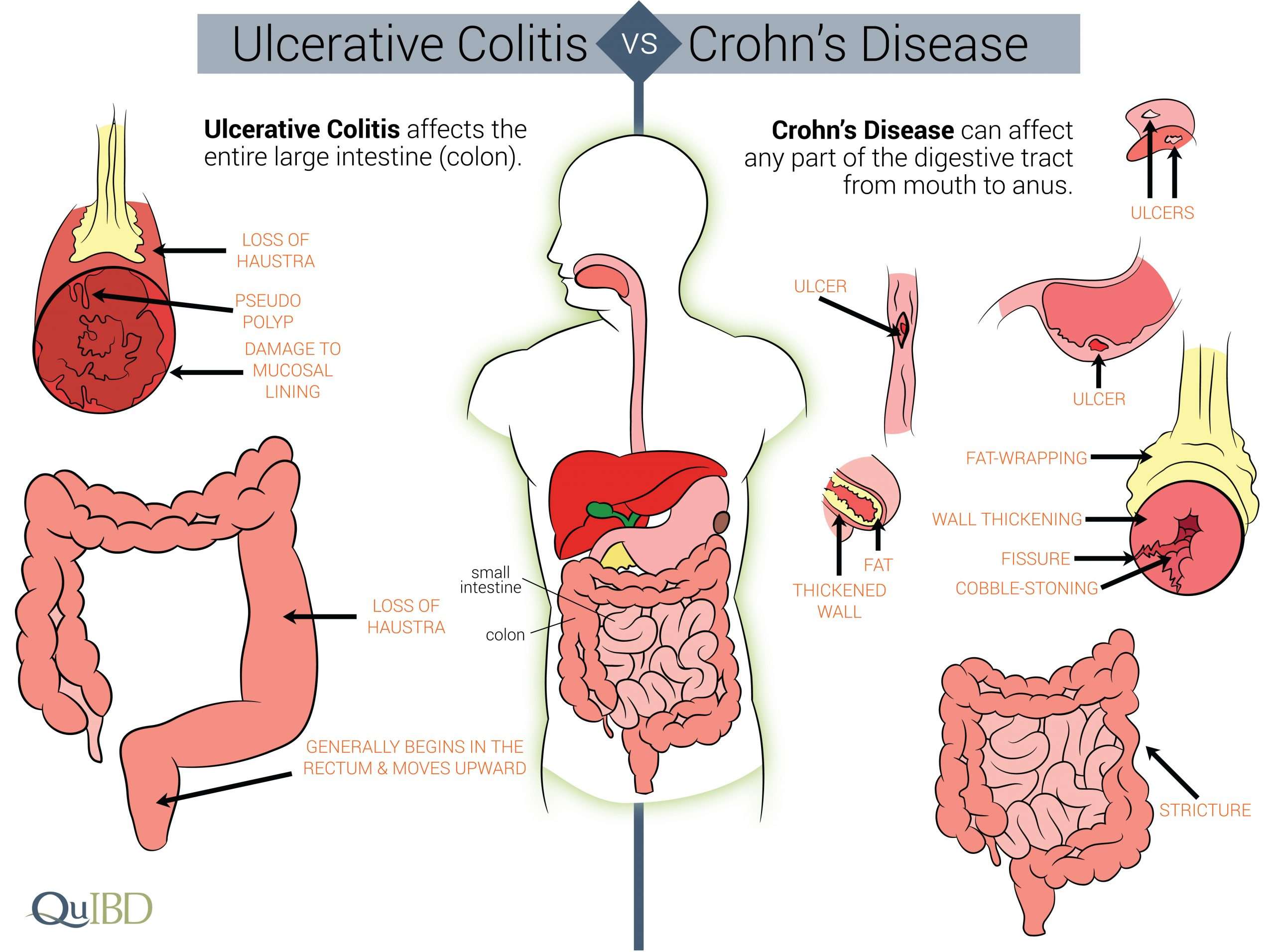
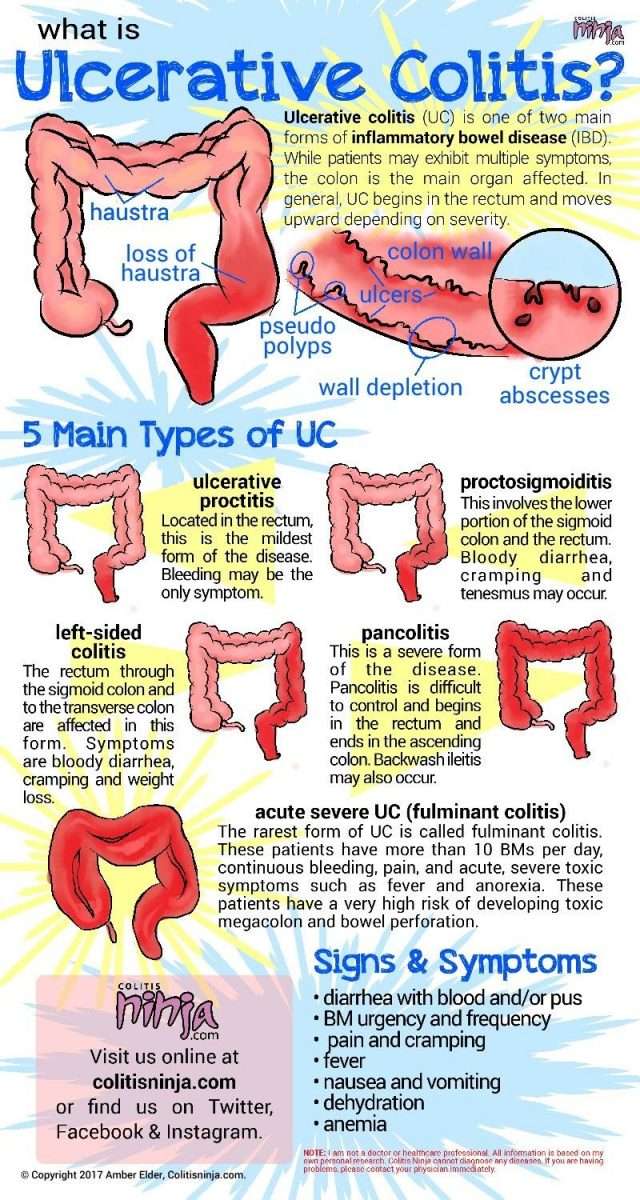
Colitis and ulcerative colitis are two medical conditions which affect the colon. These two terms often used interchangeably since they share similar signs and symptoms. But, it is important to distinguish the difference between them in order to make an accurate diagnosis and treatment. The main difference between colitis and ulcerative colitis is that ulcerative colitis is one form of colitis which results in the chronic inflammation of colonic mucosa and rectum giving rise to ulceration and bleeding.
1. What is Colitis ? Causes, Signs and Symptoms, Diagnosis, and Treatment
2. What is Ulcerative Colitis? Causes, Signs and Symptoms, Diagnosis, and Treatment
3. What is the difference between Colitis and Ulcerative Colitis?
You May Like: Stomach Ulcer And Chest Pain
Diverticulitis & Colitis Diet
Fact Checked
Diet is an important part of the management of diverticulitis or colitis 1. In diverticular disease, small pockets or pouches form in the wall of the colon when these pouches get inflamed, the condition is called diverticulitis. Colitis is an inflammation of the large intestine this can be caused by irritable bowel disease, an inflammatory bowel disease like Crohns, or infections. When you have either of these conditions, you have to make some changes in your diet during the flare-ups to aid in your recovery.
Dont Miss: Best Ulcerative Colitis Diet Book
Symptoms With Diverticulitis And Colitis
Abdominal pain: Pain and discomfort are hallmarks of both diseases, though they’re felt in different ways. With diverticulitis, discomfort can vary from tenderness to severe pain. You’ll typically feel the discomfort on the lower left side of your abdomen, according to the National Library of Medicine.
However, as Mayo Clinic points out, people of Asian heritage may feel it more acutely on the right side of the abdomen. The tenderness tends to be continuous over a period of days, says Mayo Clinic.
With colitis, abdominal pain may be continuous or could appear and then disappear, according to the National Library of Medicine. You might experience pain in the form of cramps, states the Mayo Clinic.
Diarrhea and constipation:Diarrhea is the most common symptom of colitis â it may even wake you out of your sleep â and it can be bloody and may include pus, according to the Mayo Clinic. Constipation is also possible, according to Johns Hopkins Medicine. People with colitis may also feel an urgent need to poop, yet not be able to, says Mayo Clinic. Rectal spasms are also possible. While you could experience constipation with diverticulitis, diarrhea is less likely, Mayo states.
Bloating and fever: Both diverticulitis and colitis can cause bloating and fever, according to the National Library of Medicine.
Also Check: Clinical Manifestations Of Ulcerative Colitis
What Is Crohns Disease
Crohns disease is a type of IBD where there is inflammation of the entire gastrointestinal tract, or parts of it, from mouth to anus. In addition, the entire thickness of the bowel wall is involved in Crohns disease, which can lead to some serious complications.
What are symptoms of Crohns disease?
The symptoms of Crohns disease depend on what parts of the GI tract are involved. Common symptoms include abdominal pain, weight loss, and diarrhea.
If the lower part of the GI tract such as the colon and the small intestines are involved, you might also experience:
-
Abdominal pain
What are complications of Crohns disease?
Crohns disease can lead to some serious complications, such as:
-
Fistulas, where a hole is formed between the intestines and other parts of the body such as the skin, bladder, or vagina
-
Abscesses, which are pockets of infection that may need surgery or a procedure to drain them
-
Strictures, which are a narrowing of the bowel that can lead to blockages
-
Cancers of the GI tract
Read Also: How Do They Check For Ulcers
What Causes Diverticular Disease Vs Ulcerative Colitis
Causes of Diverticular Disease
Diverticulosis is thought to be caused by increased pressure on the intestinal wall from inside the intestine.
- As the body ages, the outer layer of the intestinal wall thickens. This causes the open space inside the intestine to narrow. Stool moves more slowly through the colon, increasing the pressure.
- Hard stools, such as those produced by a diet low in fiber or slower stool “transit time” through the colon can further increase the pressure.
- Frequent, repeated straining during bowel movements also increases the pressure and contributes to the formation of diverticula.
Diverticulosis in developed countries is blamed largely on a diet low in fiber.
- Fiber is found in fruits and vegetables, whole grains, and legumes .
- There are two types of fiber soluble and insoluble.
- Soluble fiber forms a soft gel-like substance in the digestive tract.
- Insoluble fiber passes through the digestive tract nearly unchanged.
Causes of Ulcerative Colitis
The cause of ulcerative colitis is uncertain. Researchers believe that the body’s immune system reacts to a virus or bacteria, causing ongoing inflammation in the intestinal wall. Although UC is considered to be a problem with the immune system, some researchers believe that the immune reaction may be the result, not the cause, of ulcerative colitis.
Also Check: Best Thing To Take For Stomach Ulcer Pain
Diverticulitis Vs Ulcerative Colitis
This occurs in the diverticula. This occurs in the colon. Pathogenesis There is not enough evidence to suggest a genetic predisposition. Any weakness of the colon, particularly in the distal regions, can contribute to the formation of diverticula. Genetic predisposition and different environmental factors such as medications and exposure to various pollutants are believed to be the causes of ulcerative colitis. Clinical Features Change in bowel habits, vomiting, abdominal bloating, colicky abdominal pain , and constipation due to the obstruction of the large bowel are the main clinical features. In rare cases, there can per rectal bleeding when an inflamed diverticulum has ruptured. Clinical features include blood and mucus diarrhea, rectal bleeding and cramp-like abdominal pain. In addition to that, there can be nonspecific symptoms such as fever, weight loss and aphthous ulcers in the mouth. The continuous loss of blood and decreased absorption of iron can cause anemia. Complications Hemorrhages and anemia are the main complications. The chance of malignant changes is extremely low. Toxic megacolon and malignant changes are the most serious complications. In addition, there can be hemorrhages, anemia and associated arthritis. Investigations Management
What Are The Signs And Symptoms Of Diverticular Disease Vs Ulcerative Colitis
Symptoms and Signs of Diverticulosis
- Pain in the belly
- Bloating
- Constipation
- Cramping
These symptoms are nonspecific. This means that similar symptoms are seen in many different digestive disorders. They do not necessarily mean that a person has diverticulosis. If an individual has these symptoms, he or she should see a healthcare professional.
Symptoms and Signs of Diverticulitis
Diverticulitis is a more serious condition and causes symptoms in most people with the condition that include:
- Pain in the abdomen, usually in the lower-left side
- Bleeding, bright red or maroon blood may appear in the stool, in the toilet , or on the toilet paper. Bleeding is often mild and usually stops by itself however, it can become severe.
- Fever
- Chills
- Constipation
- Worsening abdominal pain
- Vomiting
- Constipation for an extended period of time
- Burning or pain during urination
- Bleeding from the rectum
Symptoms and Signs of Ulcerative Colitis
- Frequent loose bowel movements with or without blood
- The urgency to have a bowel movement and bowel incontinence
- Lower abdominal discomfort or cramps
- Fever, lethargy, and loss of appetite
- Weight loss with continuing diarrhea
- Anemia due to bleeding with bowel movements
You May Like: Specific Carbohydrate Diet Ulcerative Colitis
What Are The Treatments Complications And Risk Of Cancer For Diverticular Disease Vs Ulcerative Colitis
Diverticular Disease Treatment
A high-fiber diet is the mainstay of diverticulosis and diverticulitis prevention.
- Start a high-fiber diet because it will decrease the risk of complications and the accompanying symptoms however, will not make the diverticula a person has gone away. Foods high in fiber include:
- Whole-grain cereals and bread
- Fruits
- Vegetables
- Beans, peas, and lentils.
In the past patients with diverticulosis/diverticulitis were told that foods to avoid included seeds, corn, and nuts because it was thought fragments of these foods would get stuck in the diverticula and cause inflammation. However, current research has not found this to be the case, and the fiber content of such foods may benefit individuals with diverticulosis/diverticulitis. Discuss your diet or potential diet changes with your doctor.
Treatment for diverticulitis depends on the severity of the condition.
Treatment consists of IV or oral antibiotics, bowel rest, and possibly surgery.
If diverticulitis attacks are frequent or severe, the doctor may suggest surgery to remove a part of the patient’s colon.
- As with any surgery, there are risks the patient should discuss with his or her doctor.
- Sometimes the operation requires at least two separate surgeries on different occasions.
When Surgery Is Needed
If medication isnt reducing the inflammation and IBD progresses, surgery may be needed. This is where people with ulcerative colitis tend to fare better.
If the colon gets bad enough in ulcerative colitis, its removed and replaced with an internal pouch, which functions like a colon, says Cohen. According to the Mayo Clinic, colectomy surgery whether partial or full usually requires additional procedures that reconnect the remaining portions of the digestive system so they can still rid the body of waste.
However, things are looking up. A study published in December 2019 in the Journal of Gastrointestinal Surgery found that due to advances in medicine and medical care for IBD patients over the past decade, the number of hospitalized patients with ulcerative colitis who require a colectomy decreased by nearly 50 percent between 2007 and 2016.
According to the Crohns and Colitis Foundation, proctocolectomy with ileal pouchanal anastomosis usually called J-pouch surgery is the most common surgery performed on people with UC who have not responded to medication. Surgeons remove the rectum and colon and then create a temporary opening in the abdomen, called a loop ileostomy, which will allow waste to move from the small intestine into an ostomy bag that sits outside the body while the digestive system heals from the surgery. In some cases a stoma, or permanent opening in the abdomen that funnels waste into an external bag, is required, notes the Mayo Clinic.
Recommended Reading: Air Mattress For Decubitus Ulcers
Therapeutic Focus And Assessment
We initiated therapy with corticosteroids and 5-amino-salicylate derivatives , as well supportive treatment . The initial disease progression, within the first 2 weeks, was burdened by the presence of up to 11 bloody stools per day, prompting the patient to undergo multiple blood transfusions . After ~14 days of corticosteroid therapy, the patient’s condition started to progressively improve. We repeated colonoscopy after ~6 weeks , and we observed an improvement of the initial colonic lesions.
Figure 2. Aspect of the colon after 6 weeks.
Getting To A Diagnosis
Theres no doubt that IBD can significantly decrease quality of life, between uncomfortable symptoms and frequent bathroom visits. IBD can even lead to scar tissue and increase the risk of colon cancer.
If you experience any unusual symptoms, its important to call your doctor. You may be referred to a gastroenterologist for IBD testing, such as a colonoscopy, sigmoidoscopy, or a CT scan. Your doctor may also order blood and fecal testing. Diagnosing the specific form of IBD will lead to more effective therapies.
Commitment to daily treatment and lifestyle changes can help minimize symptoms, achieve remission, and avoid complications.
Regardless of your diagnosis, Healthlines free app, IBD Healthline, can connect you with people who understand. Meet others living with Crohns and ulcerative colitis through one-on-one messaging and live group discussions. Plus, youll have expert-approved information on managing IBD at your fingertips. Download the app for iPhone or Android.
You May Like: How To Ease Stomach Ulcer Pain
Summary Diverticulitis Vs Ulcerative Colitis
Diverticulitis is the inflammation of the diverticula arising from the colon whereas ulcerative colitis is the inflammation of the colon with the formation of associated ulcers. In the ulcerative colitis the colonic mucosa gets inflamed, but in diverticulitis, the diverticula that originate from the colon are the structures that get inflamed. This is the difference between diverticulitis and ulcerative colitis.
Are Ibs And Diverticulitis Related
People with one may also have the other, but technically are not directly related. However, the symptoms can be very similar, as discussed by Dr. Spiller in the medical journal Digestive Diseases. Diverticulitis is a type of inflammation in the colon. Sometimes doctors misdiagnose a patient with diverticulitis when they may actually have IBS, or they may also have IBS. These two conditions are sometimes difficult to differentiate. Learn more about IBS and diverticulitis.
Dont Miss: What Causes Mouth Ulcers On Gums
Also Check: Zinc Oxide For Stage 2 Pressure Ulcer
Study Design And Inclusion Criteria
This is a cross-sectional study and includes all patients18years old with a primary diagnosis of acute diverticulitis in 2014. The ICD-9 CM codes used were 56211, 56201, 56213, and 56203. The database was then queried to include all patients with prior diagnosis of CD or UC . Patients included in the study were required to have a primary diagnosis of acute diverticulitis with a prior diagnosis of either UC or CD. Primary study outcomes included mortality, cost of hospitalization, and length of stay for diverticulitis with either UC or CD. A second comparison was made between those with CD and those without IBD. Various patient demographics , comorbidities, and hospital characteristics were obtained. The severity of the co-morbidities was analyzed via the Deyo modification of the Charlson comorbidity index . This index measures 17 common medical conditions and assigns different weights to compile a score from 0 to 33, which correlates with overall severity of illness.
What Is Irritable Bowel Syndrome
Irritable bowel syndrome is a chronic condition associated with abdominal pain and a change in bowel habits either constipation or diarrhea. It is a chronic condition. In some cases, it can cause significant pain and discomfort.
The cause of this condition is unknown, but is thought to result from an impairment in the signaling between your gut and brain. There are certain triggers which cause the symptoms to flare up. Adjusting your diet and managing stress can help improve IBS symptoms.
Also Check: Preventing Pressure Ulcers In Nursing Homes
Can Ibs Cause Depression
Absolutely. Does IBS make you happy or sad? IBS can be very debilitating and therefore can cause people to be depressed. It used to be common to treat IBS with antidepressants . Unfortunately, this will rarely cure IBS and is not addressing the cause of the IBS. Many studies have documented a link between IBS and depression as well as anxiety, as described in the European Archives of Psychiatry and Clinical Neuroscience.
Ulcerative Colitis And Diverticulitis: Whats The Outlook
UC is a lifelong condition, and your symptoms may come and go. About 30% of people with UC have severe symptoms, and flare-ups might happen more frequently. While medications often help, surgery may also be needed.
In contrast, most cases of diverticulitis, even though itâs also considered a lifelong condition, clear up with a 7- to 10-day course of antibiotics and plenty of rest. If you have severe symptoms, talk to your doctor about other treatment options.
Managing your diet and stress and making time for regular physical exercise are key to lowering your risks for both conditions. However, because some of the symptoms are specific, there are steps you can take to avoid your condition flaring up or getting worse.
To prevent diverticulitis, you should:
- Eat more fiber. This helps your poop move better in your digestive tract and reduces any pressure on the colon walls
- Drink lots of water, this prevents constipation.
If youâre not sure what to eat, talk to your doctor.
To lower your odds for UC or manage flare-ups, you should:
- Get plenty of sleep. This can ease emotional stress and keep your immune system in check.
- Avoid using too many nonsteroidal anti-inflammatory drugs . For pain relief and fever, switch to alternatives like acetaminophen .
- Be careful when you take antibiotics. These drugs can trigger UC flare-ups. Let your doctor know if it does.
Show Sources
Recommended Reading: How To Prevent Skin Ulcers