What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
What Does A Uc Cramp Feel Like
People who have UC describe a pronounced sensation of squeezing and releasing in their abdomen, Dr. Ha says, that feels more like pressure than a stabbing pain.
Doctors diagnose UC based on where symptoms are occurring. Many people with the condition experience whats known as left-sided colitis, where the pain and inflammation occur on their left side, from the rectum up to the descending colon.
Cramps can also be accompanied by bloating and gas, which cause a feeling of pressure and knotting in your abdomen.
Upper Middle Abdominal Pain
A type of IBD called gastroduodenal CD often causes pain in the middle and upper sections of the abdomen. These Crohn’s disease pain locations correlate with problems in the:
This disease type is rare, accounting for only about 4% of all diagnoses. It’s even more rare for it to only impact the duodenum. This happens in just 0.07% of all CD cases.
Other symptoms of gastroduodenal CD may include:
- Fullness, or an inability to eat very much at once
| Jejunoileitis |
Recommended Reading: Best Alcohol To Drink With Ulcerative Colitis
What Are The Medication Options For Ulcerative Colitis
There are a few types of drugs used to treat ulcerative colitis.
Aminosalicylates are typically the first kind of drug prescribed for ulcerative colitis. They work by reducing inflammation directly in your digestive tract and can be taken on an ongoing basis.
Corticosteroids, also known simply as steroids, are used to treat disease flares. Most drugs of this type work by suppressing the entire immune system, so they can have severe side effects and shouldnt be taken for long periods.
Biologics are made of antibodies that are grown in the lab and work by stopping certain proteins in the body from causing inflammation.
Small molecules are oral medications that also work on the immune system but act differently from biologics.
These drugs are used to treat moderate to severe ulcerative colitis.
Immunomodulators are a second-line drug for treating ulcerative colitis. These drugs limit inflammation at its source in the immune system.
Other drugs for ulcerative colitis may include antibiotics and certain pain relievers.
Switching To A Biosimilar: Effies Experience
At the start of 2020 the government announced that coverage was changing for people who take Remicade® for the treatment of Crohns disease or ulcerative colitis. This meant that patients receiving the biologic drug infliximab, marketed as Remicade®, would see this coverage discontinue with new coverage for the biosimilar version: Inflectra and Renflexis.
Ulcerative colitis advocate Effie was one of those people. In this self-produced video, Effie talks all about her experiences with switching to a biosimilar, takes us through her first Inflectra infusion, and answers some of the same questions you may be asking yourself if you will be going through the same process:
- What is a biosimilar?
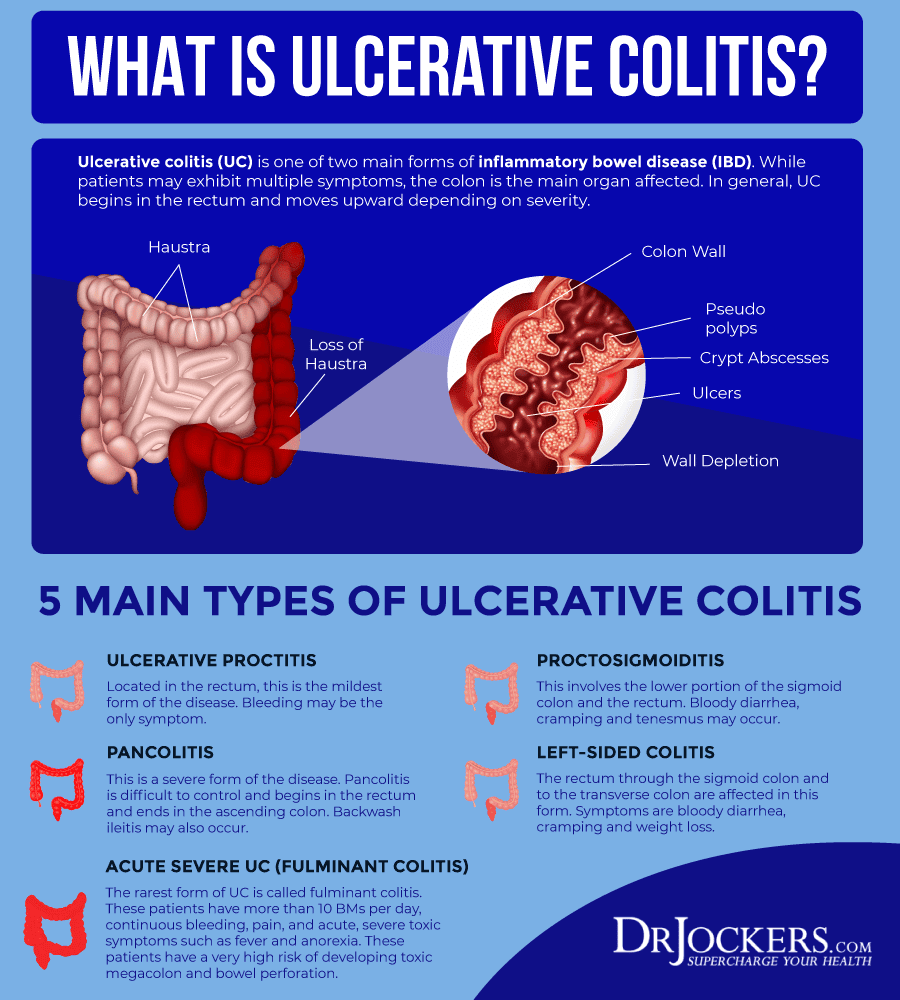
Ulcerative colitis is a form of inflammatory bowel disease that causes the lining of the colon to become inflamed. Ulcers can form in the large intestine and produce pus and mucus.
Symptoms can vary among people but may include bloody stools, abdominal pain, loose or urgent bowel movements, and persistent diarrhea.Constipation may also occur in people living with ulcerative colitis.
Read on to learn about the link between ulcerative colitis and constipation, how to manage it, and when to see a healthcare provider.
Read Also: How To Relieve An Ulcer
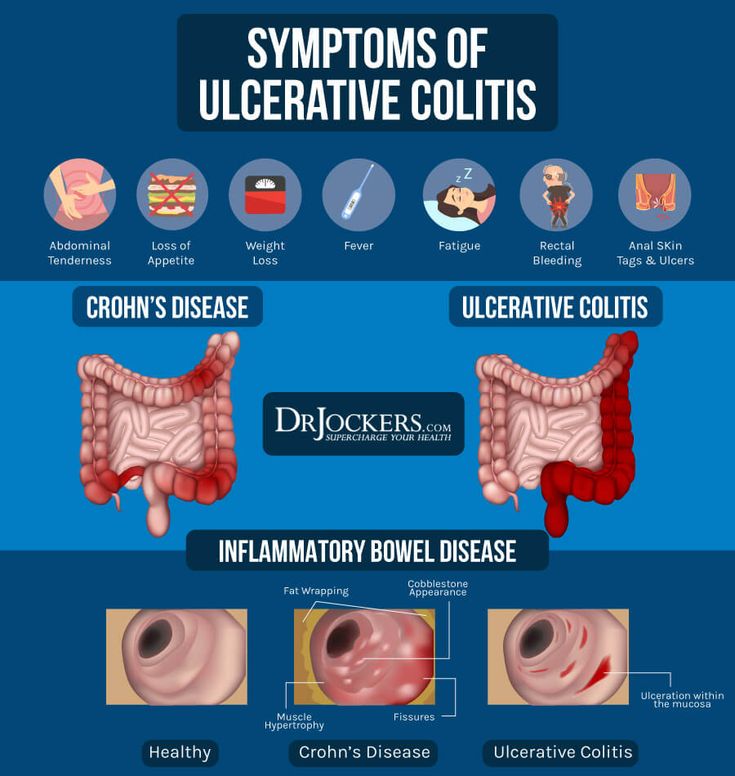
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
Ulcerative Colitis Symptoms You Should Never Ignore
Ulcerative colitis is an autoimmune disease in which the immune system attacks the colon and causes a range of symptoms, both in the GI tract and around the body.
Symptoms of ulcerative colitis, a type of inflammatory bowel disease , can vary widely depending on how much inflammation a person has and where the inflammation is located.
Abdominal pain and bloody diarrhea are the most common warning signs of UC, and can range from mild and intermittent to severe and chronic. The pain of UC is quite common and can significantly impact quality of life. Ulcerative colitis symptoms tend to come and go, often with extended periods of time in between flares. These are called remission periods.
The disease tends to develop gradually over time, so you might not automatically think of ulcerative colitis or IBD if you have occasional abdominal pain or digestive distress.
Ongoing inflammation along with ulcers and abscesses in the intestines are additional common causes of pain. Scarring in the lining of the intestinal tract can lead to painful obstructions. Pain may occur in different areas such as the abdomen or rectal area, depending where the inflammation is located. For example, people may experience moderate to severe pain on the left side of the abdomen if the UC affects the rectum and the lower segment of colon.
UC symptoms might ebb and flow, but they wont go away unless you see a gastroenterologist and start treatment.
Also Check: Is Papaya Good For Ulcerative Colitis
Home Remedies For Uc Joint Pain
Just like other aspects of your UC, joint pain is sometimes one that you can help keep under control at home. According to Dr. Keller, keeping your joints moving can make all the difference. Exercise therapy, such as gentle water exercises developed for arthritis, can help with the pain, she says. And when you are sitting or standing, pay special attention to your posture. A physical therapist can help you develop an exercise program and observe your posture to help you move correctly.
Given that this all comes down to controlling inflammation, adding anti-inflammatory supplements such as turmeric to your diet may also be helpful. Curcumin is the active ingredient in turmeric and has been shown to improve inflammation related to both inflammatory arthritis and UC. In a 2021 review published in Complementary Therapies in Medicine, curcumin supplementation was associated with decreases in inflammatory markers in adults with rheumatoid arthritis and UC in comparison to a control group.
And dont forget about the variety of topical pain relievers that are now available over the counter. They are divided into different types based on how they work on your pain. Your pharmacist can help you navigate the options and choose the one that is right for you.
UC and Joint Pain: Crohns and Colitis Foundation. Arthritis and Joint Pain.
Recommended Reading: Colitis Vs Ulcerative Colitis Symptoms
When Does Cramping Usually Happen
UC cramps can be exacerbated by food, so many people notice cramping after eating or before a bowel movement, says Ha. Cramping can also be tied to eating trigger foods, which often include high-fiber fruits and veggies, lactose, nonabsorbable sugars, high-fat or sugary foods, alcohol, and caffeine.
The hormone fluctuations that occur during a womans menstrual cycle may also trigger UC cramping, according to a study published in January 2018 in Inflammatory Bowel Diseases.
Cramping can occur at all times and throughout the night. Medication and other treatments can help reduce symptoms.
Don’t Miss: Best Supplements For Ulcerative Colitis
Types Of Ulcerative Colitis
The different types of ulcerative colitis and symptoms are based on the location of inflammation within the colon or rectum. The types of ulcerative colitis include:
- Ulcerative proctitis: This is the mildest form of ulcerative colitis. Inflammation is in the rectal area and causes rectal pain and bleeding and an urgent feeling to move your bowels.
- Proctosigmoiditis: With this type, inflammation is in the rectum and lower area of the colon, causing stomach pain and cramping, bloody diarrhea and trouble moving your bowels despite the urge to go.
- Left-sided colitis: The inflammation of this type extends from the rectum through the sigmoid and descending colon in the upper-left abdomen. This type causes stomach pain and cramping on the left side, bloody diarrhea and weight loss.
- Pancolitis: This type causes inflammation of the entire colon that causes stomach pain and cramping, bloody diarrhea, significant weight loss and fatigue.
- Fulminant colitis: This is the rarest and most severe form of ulcerative colitis. It can cause extreme diarrhea, dehydration and shock, and it can be life-threatening.
Where The Pain Occurs
Pain is a common symptom of UC. According to the Crohns & Colitis Foundation, 33% of people with UC experience chronic abdominal pain. Pain management is, therefore, an important part of the treatment plan.
Pain due to UC occurs most commonly in two regions: the rectum and the lower left side of the abdomen. Doctors associate the areas of inflammation with a certain type of UC.
The severity of the symptoms can vary over time, with people often experiencing periods of mild or no symptoms, known as remission, alternating with periods of more severe symptoms, known as flare-ups.
Don’t Miss: How Do You Test For Stomach Ulcers
Back Pain And Ulcerative Colitis
| | |
Research indicates that nearly 25 percent of people with inflammatory bowel disease including ulcerative colitis and Crohns disease experience chronic lower back pain. Ankylosing spondylitis and axial arthritis both of which can cause back pain are two common causes of back pain for people with UC.
That said, a doctor may not suspect that a person with back pain has UC unless they also experience gastrointestinal symptoms. If you do experience back pain, its important to let your doctor know even if you dont suspect its related to UC. They will be able to determine the cause of your pain and work with you to find the best way of managing it.
A person having backaches may not realize theyre related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
What Causes Uc Cramping
Common causes of UC cramping, according to Ha, are flare-ups, lack of sufficient control of the condition , eating foods that are high in saturated fat or sugar, and adverse reactions to medication.
Cramping due to gas and bloating can also be caused by irritable bowel syndrome , a separate condition from ulcerative colitis that can cause symptoms even when your disease is in remission. IBS can be linked to certain gas-causing foods, including dairy if youre lactose intolerant.
You May Like: Stage 2 Pressure Ulcer Pictures
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
People Describe How They Were Diagnosed With Ulcerative Colitis
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohn’s disease .
UC is a chronic condition that can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while there’s no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesn’t cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Don’t Miss: What Foods To Eat With A Peptic Ulcer
Pain As A Tool For Diagnosis
Pain can come from different sources, and pain in the abdomen is particularly difficult to pinpoint. This means that it is not a symptom that is normally used to diagnose IBD or a specific form of IBD.
Rather, the type and location of pain may be used together with other signs and symptoms. The pain serves to help a healthcare provider begin a diagnosis of IBD or other conditions. Keep in mind that it’s only a starting point.
Sex Pregnancy And Ankylosing Spondylitis
Sex may be painful if you have ankylosing spondylitis. If it is, try taking some painkillers beforehand and experiment with different positions.
Ankylosing spondylitis can make you feel tired, so its important your partner understands how your condition affects you. Good communication can help you maintain an active sex life and counselling can sometimes benefit both partners.
Its fine to use the contraceptive pill if you have ankylosing spondylitis, but you should tell your doctor youre taking it.
If youre thinking of starting a family, its very important for both men and women with ankylosing spondylitis to discuss medication with a doctor beforehand.
Some drugs such as methotrexate should be stopped several months before a woman tries to get pregnant. Latest research suggests its safe for men to take methotrexate when trying for a baby with their partner.
Biological therapies seem to be safe in the earlier stages of pregnancy but are then stopped later in pregnancy.
If you become pregnant while using a conventional DMARD such as methotrexate or a biological therapy, discuss this with your rheumatology team as soon as possible.
Usually, pregnancy doesnt cause any special problems for the mother or baby, though the symptoms of ankylosing spondylitis may not ease during pregnancy. If your spine is very stiff, it may not be possible to have an epidural during childbirth. This is an injection into the back that stops people feeling pain in part of the body.
Don’t Miss: What Can I Eat When I Have A Stomach Ulcer
Joint Pain: The Most Common Non
About 30 percent of people with ulcerative colitis experience joint pain, according to the Crohns and Colitis Foundation, making it the most common non-GI symptom of the disease. Joint pain often occurs in the knees, ankles, elbows, and wrists. Its usually joint pain thats symmetrical, meaning both knees or both ankles, says Dr. Rubin. This type of joint pain tends to parallel bowel activityso if you fix the intestine, the joint pain goes away.
However, ulcerative colitis is also related to inflammatory joint conditions that affect your spine, like ankylosing spondylitis. This type of joint pain can be independent of your bowelso your bowel can be completely in remission, and your back or your pelvis is inflamed, and you can have joint damage, says Rubin.
The good news: Some medications used to treat ulcerative colitis are also used to treat inflammatory joint conditions like ankylosing spondylitis. Its not that fixing the bowel makes these joints betterits that the medication that works on the bowel also works on these joint conditions, says Rubin. So if youre experiencing joint pain, its important to work with your doctor to understand what type of joint pain you have and get proper treatment. In some cases it may be necessary to see a doctor who specializes in the joints, a rheumatologist, to work with your IBD doctor.