Combination Therapy But For How Long And What Dose
The data support initiation of combination therapy, particularly with infliximab, but the optimal duration of continuing immunomodulator therapy prior to de-escalation remains controversial. It has been shown that the first 6 months of combination therapy are the most important to prevent immunogenicity . Van Assche et al demonstrated that maintaining azathioprine with infliximab after 6 months of combination therapy does not provide any extra clinical advantage compared to the optimization of infliximab dosing however, the authors did not assess the predictors of infliximab therapy failure after azathioprine withdrawal . Six months after stopping azathioprine, the CRP levels were normal. Two years later, however, the CRP levels were higher, infliximab levels lower, but there was no need to escalate infliximab dosing compared to patients who continued azathioprine . Retrospective studies have shown that continuing combination therapy for at least 2 years was associated with fewer IBD flares, fewer perianal complications, fewer switches to adalimumab, lower CRP levels, and stable infliximab doses . Oussalah et al assessed the consequences of azathioprine discontinuation in CD patients on infliximab who had reached remission, and they found that stopping azathioprine will lead to relapse if the duration of the combination therapy is less than 27 months and if the patient already has active inflammation .
Evaluation Of The Activity Of Tnf
We evaluated whether the formation of TNF- siRNA-encapsulating plasma sEVs could reduce TNF- expression in an ex vivo model . When macrophages were incubated with plasma sEVs derived from DSS mice injected with the CMV-siRTNF- circuit and then stimulated with LPS, a significant decrease in TNF- mRNA expression was observed , which was accompanied by a reduced amount of TNF- secreted into the cell culture medium . These results indicated that the CMV-siRTNF- circuit could trigger the self-assembly of TNF- siRNA into plasma sEVs in vivo, which could be further internalised by recipient cells to block TNF- expression.
Fig. 3: Evaluation of the activity of TNF- siRNA-encapsulating sEVs in an ex vivo model.
Nps Do Not Affect Cell Viability
Cytotoxicity is a primary concern in efforts to develop novel formulations for UC therapy. To evaluate the cytotoxicity of the obtained NPs, we treated Colon-26 cells and Raw 264.7 macrophages with various NPs, and examined cell viability using the MTT assay . A low degree of cytotoxicity was observed in the groups treated with HA-CUR-NPs. However, neither HA-siCD98-NPs nor HA-siCD98/CUR-NPs caused obvious cytotoxicity in either cell line, even after 48 h of co-incubation. This indicates that these NPs have excellent biocompatibility. In addition, we examined the cytotoxicity of HA-CUR-NPs at higher CUR concentrations up to 125 µM after 5 h of co-incubation . It was found that HA-CUR-NPs exhibited slight cytotoxicity on Colon-26 and Raw 264.7 at a CUR concentration of 125 µM, under which the cells retained viability over 81%. However, at CUR concentrations below 100 uM, more than 88% of cells were viable. Therefore, HA-CUR-NPs were well tolerated by both cell lines under CUR concentration of 100 uM, and this concentration was used for further cellular uptake imaging test.
Also Check: Does Ulcerative Colitis Cause Back Pain
Combination Therapy For Inflammatory Bowel Disease
Correspondence to: Keith S Sultan, MD, Assistant Professor of Medicine, Department of Medicine, Division of Gastroenterology, Hofstra Northwell School of Medicine, 300 Community Dr., Manhasset, NY 11030, United States.
Telephone: +1-516-3873990 Fax: +1-516-3873930
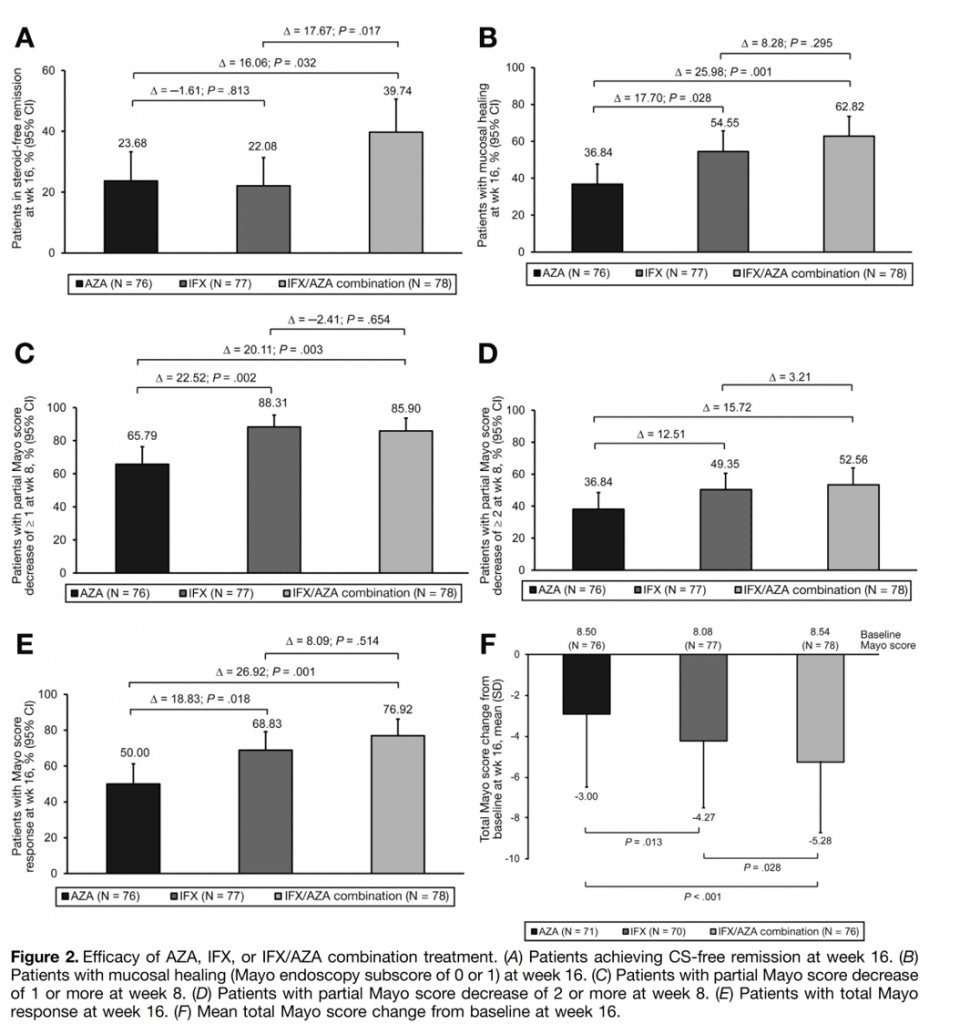
Combination Treatment For Crohn’s: Risk Cost
The treatment is not without risk. Remicade and other anti-TNF drugs increase a patient’s risk of life-threatening infections and cancers. So do immune-suppressing drugs, although the Remicade trial suggested that combination therapy is not more risky than azathioprine or Remicade alone.
In the study, 4% of patients receiving the Remicade/azathioprine combination developed serious infections, as did 5% of those in the Remicade-only group and 5.6% of those in the azathioprine-only group.
And the treatment is expensive. A 155-pound patient would need about 350 milligrams of Remicade per treatment. Four 100-milligram vials of Remicade cost $2,763, according to drugstore.com.
Other anti-TNF drugs, which Sandborn and Kerman say should work as well as Remicade, cost about as much. But Kerman notes that anti-TNF therapy for Crohn’s disease is actually cost-effective, as the drugs prevent hospitalizations, loss of work, and other expenses.
“I’d like for Crohn’s patients to ask their doctors to consider combination treatment with these biologics and immune modulators as an early therapy,” Kerman says. “It has been shown that treating much earlier gives them a much better chance of responding, rather than getting the treatment after damage already has been done.”
The combination therapy does not cure Crohn’s disease. Treatment must continue indefinitely. However, Sandborn says that some of the patients in the earliest clinical trials are still doing well after 12 years of treatment.
Recommended Reading: Signs And Symptoms Of Ulcerative Colitis Flare Up
Development Of Optimised Aav8
Although we optimised the delivery vehicles of the genetic circuit and developed an AAV9-based strategy for permanent self-assembly of sEV-enclosed siRNAs for the treatment of UC, the therapeutic effects observed in UC models may not be liver dependent because AAV9 has tropism for a wide range of tissues, and the CMV promoter is a strong constitutive promoter without tissue specificity. AAV8 has strong liver tropism,, and the thyroxine-binding globulin promoter is a hepatocyte-specific promoter,. Therefore, the expression cassette designed for tandem expression of TNF- siRNA, B7-1 siRNA and integrin 4 siRNA was inserted downstream of the TBG promoter, and the entire circuit was further incorporated into an AAV8 vector . Such an AAV8-TBG-driven genetic circuit ensures that the corresponding siRNAs are transcribed only in hepatocytes while avoiding undesired siRNA expression in extrahepatic cells.
Fig. 10: Intravenous injection of the AAV8-TBG-siRT+B+I induces long-term combination therapy in the DSS-induced chronic UC model.
Combination Of Anti Tnf
Since their introduction, anti-TNF agents have been a game changer for the management of IBD. However, a significant proportion of patients fails to respond or loses response to these drugs and the development of anti-drug antibodies has been identified as a major responsible for treatment failure . In a prospective, open-label trial, the association of an immunosuppressant with infliximab has been linked with a significant reduction of antibodies toward infliximab formation
Don’t Miss: Foods That Flare Up Ulcerative Colitis
Construction And Characterisation Of The Genetic Circuits Targeting Tnf
TNF- is a key pro-inflammatory cytokine produced primarily by activated macrophages and T lymphocytes, and it plays an integral role in the pathogenesis of UC. TNF- induces other pro-inflammatory cytokines and IL-6), enhances leucocyte migration by inducing the expression of adhesion molecules and inhibits apoptosis of inflammatory cells. We therefore evaluated the therapeutic effects of the genetic circuit designed to specifically target TNF- in colonic macrophages for the treatment of UC. We constructed a genetic circuit consisting of two functional modules: the promoter module drives the transcription of siRNA, which leads to the package of saturated cytoplasmic siRNA into sEVs, while the siRNA expression cassette module maximises the expression of the siRNA guide strand and minimises the expression of undesired passenger strand. Based on our previous study, the cytomegalovirus promoter was selected as the promoter module, and the pre-miR-155 backbone was selected as the optimal siRNA expression cassette to produce siRNA. By inserting the TNF- siRNA sequence into the 5 arm of the pre-miR-155 hairpin, a CMV-directed genetic circuit carrying a TNF- siRNA expression cassette was constructed .
Fig. 1: Schematic description of the architecture of the genetic circuits.
How Is Combination Therapy Used To Treat Ibd
It is usually used in patients who have moderate to severe Crohns disease or ulcerative colitis which isnt responding to single medications.
Traditionally treatment of IBD follows a step-up approach, working through a pyramid of different medications until an effective treatment is found for the patients Crohns disease or ulcerative colitis. Biologics are at the top of this pyramid, with immunosuppressants on the step below. Due to following this treatment pathway, patients who start taking a biologic treatment are usually already taking an immunosuppressant medication which they havent been responding well to. This can then result in combination therapy, with the patient starting a biologic while continuing to take the immunosuppressant. A patient may stay on the immunosuppressant for six to 12 months before stopping it1.
However, in some cases the step-up treatment pathway isnt followed and a doctor makes a decision on a case-by-case basis to follow a different route, perhaps starting a patient straight on a biologic as their first treatment.
He continued: The efficacy of combination therapy offers a huge potential benefit, and use of combination therapy is most advantageous in patients with the most severe disease. In selecting a treatment for a specific patient, however, clinicians must consider the riskbenefit ratio for that individual.
You May Like: How To Take Flax Seeds For Ulcerative Colitis
Similar Articles Being Viewed By Others
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
09 September 2021
Anam Akhtar
28 May 2021
Daniel van der Lelie, Akihiko Oka, R. Balfour Sartor
24 June 2019
volume 13, Article number: 5700
Colitis Tissue Uptake Orally Ha
To investigate the in vivo bio-distribution of HA-functionalized NPs in the GIT, we orally administered DSS-treated mice with HA-DiR-NPs encapsulated in hydrogel, and examined the time-dependent passage and in vivo targeting efficacy of the formulations using near infrared fluorescence imaging. As shown in Figure. 5b and Figure S5 , a strong NIRF signal was observed in the small intestine and colon at 8 h after oral administration. This signal decreased gradually with time, indicating that rapid clearance occurred in the feces. As the fluorescence was relatively weak by 24 h post-administration, mice were gavaged daily during the treatment process.
Next, we evaluated the tissue bio-distribution of HA-functionalized NPs. HA-CUR-NPs encapsulated in hydrogel were orally administered to DSS-treated mice. Once the NPs were released from the hydrogel, they had to go through the mucus layer. As shown in Figure 5c, tissue cross sections revealed that almost all colonic epithelial cells had internalized the NPs by 12 h after oral administration of HA-CUR-NPs. Importantly, we also found that large amounts of NPs penetrated deep into the mucosa and were taken up by the cells .
Don’t Miss: Best Wound Care For Stage 2 Pressure Ulcer
Investigators Tout Promising Data On Ustekinumab Combination Therapy For Ulcerative Colitis
In total, 64.9% of patients who achieved clinical response with ustekinumab during induction were in symptomatic remission after 44 weeks.
New data continues a positive trend for ustekinumab , guselkumab and golimumab as potential treatments for patients with ulcerative colitis.
Janssen Pharmaceuticals announced the new data from the Stelara Phase III UNIFI trial and an ongoing analysis from the phase 2a VEGA study.
Combination Therapy Commonly Used With Entyvio Stelara
Lutz et al. Poster 3524370. Presented at: Digestive Disease Week May 21-24, 2021 .
Disclosures: We were unable to process your request. Please try again later. If you continue to have this issue please contact .
Entyvio and Stelara were commonly used in combination therapy for the treatment of inflammatory bowel disease, according to research at Digestive Disease Week.
When used with an immunomodulator , anti-TNFs are associated with lower rates of anti-drug antibodies and increased rates of clinical remission but also with increased rates of infections,Megan Lutz, MD, fellow at the University of Wisconsin School of Medicine and Public Health, told Healio Gastroenterology. and are newer biologic therapies that do not seem to carry the same risk for infection as anti-TNFs or immunomodulators. A growing body of evidence also suggests that these newer biologics have lower rates of immunogenicity and are not necessarily more effective when used with an immunomodulator. Further prospective data are needed to determine efficacy and minimize risk for patients initiating combination therapy with vedolizumab or ustekinumab for IBD.
Investigators stratified rates of combination therapy by time from drug approval and previous exposure to other biologic agents. They used bivariate statistics to compare patient characteristics between those on monotherapy and combination therapy at enrollment.
Read Also: New Biologic Drugs For Ulcerative Colitis
Quantification Of Cellular Uptake Using Flow Cytometry
Colon-26 cells and Raw 264.7 macrophages were seeded in 12-well plates at a respective density of 4×105 and 1×105 cells/well and incubated overnight. The medium was exchanged to serum-free medium containing various NPs . Cell treated with blank NPs were used as a negative control. After incubation for different time periods , the cells were thoroughly rinsed with PBS to eliminate excess NPs, which were not taken up by cells. Subsequently, the treated cells were harvested using accutase or trypsin, transferred to centrifuge tubes, and centrifuged at 1,800 g for 5 min. Upon removal of the supernatant, the cells were re-suspended in FCM buffer, transferred to round-bottom polystyrene test tubes , and kept at 4 oC until further analysis. Analytical FCM was performed using the FITC channel on the FCM CantoTM . A total of 5,000 ungated cells were analyzed. The competition assay was carried out to confirm the cellular uptake of HA-functionalized NPs. The uptake efficiency of Colon-26 cells and Raw 264.7 macrophages with these NPs in the presence of free HA as a competitor was also tested by FCM.
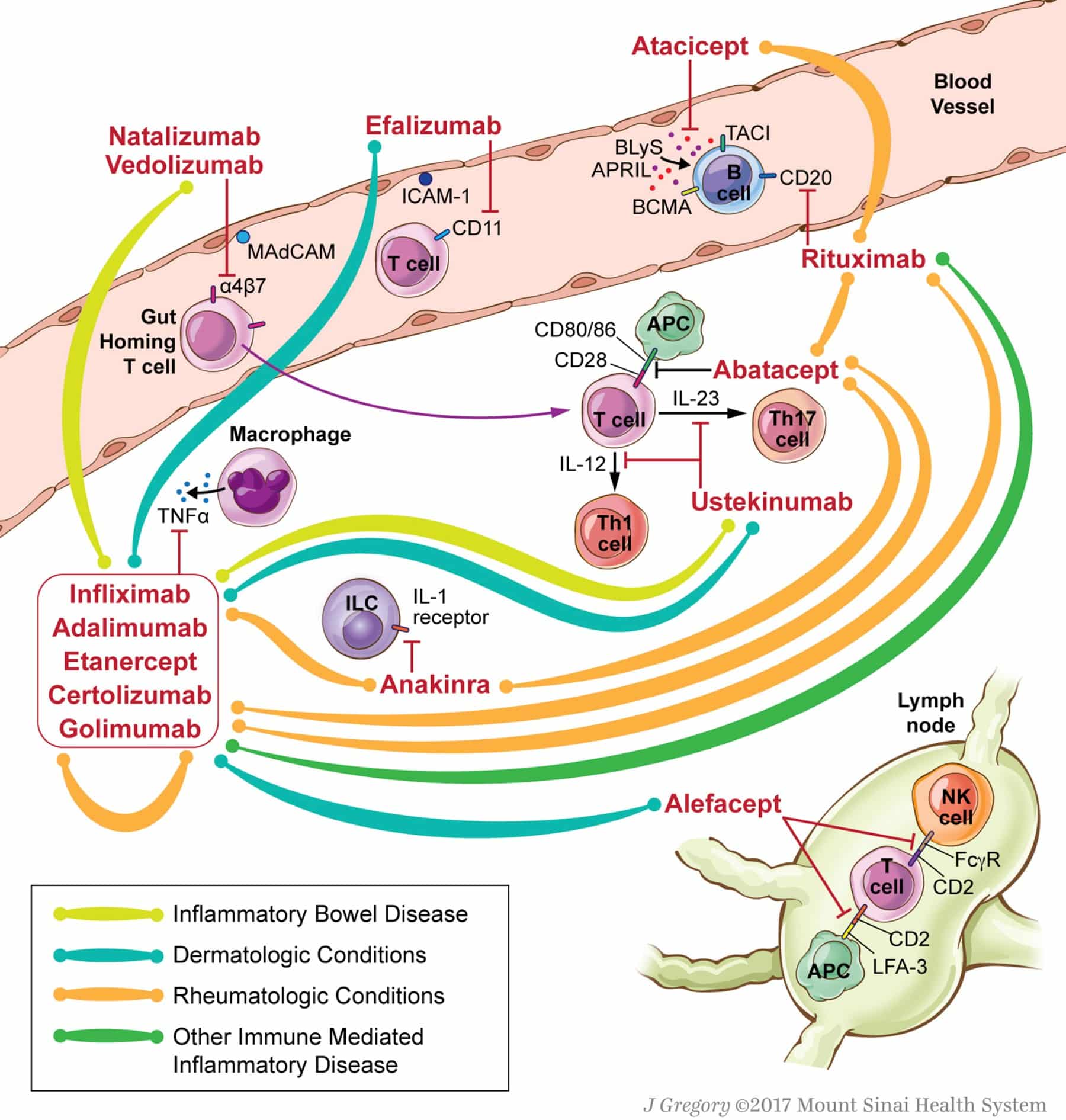
Introduction: Why Do We Need Combination Therapy In Ibd
The objective of this presentation was to discuss sequencing of therapies incorporating new molecules and new strategies in IBD with emphasis on combination biologics. The rationale for dual biologic therapy is that multiple pathways drive inflammatory process and that remission rates for currently available biologics remain limited when used as single agents. Furthermore, mechanistic failure can lead to secondary loss of response with single biologic agents, biologics used second- or third-line tend to be less effective, and agents effective for luminal disease may not be as effective for extraintestinal manifestations or other concomitant immune-mediated inflammatory diseases . This is particularly relevant given the burden of IBD often goes beyond the gut, and studies have shown that IBD patients have a 7.5 times higher risk of developing another IMID compared with non-IBD patients.
Theoretical advantages of combined therapy include greater efficacy, prevention of immunogenicity, and increased drug concentrations. Potential disadvantages of combined therapy include increased adverse effects, unknown safety risks, the complexity and cost of the regimen, and an increased need for patient monitoring.
You May Like: Heel Protectors For Pressure Ulcers
Up Therapy: Adding Imm To Failing Biologic
The issue of stepping up to CT by the addition of IMM to failing biologic is less well studied. A small retrospective cohort analysis by Ben-Horin et al examined the outcomes of 5 patients with a secondary loss of response to IFX associated with high ATI levels and undetectable trough. Two patients were treated with MTX and 3 received either AZA/6MP. In all cases patients experienced a decrease in ATI, an increase in trough, and a recapturing of clinical response. Despite the questionable efficacy of CT when the anti-TNF is ADA, the same group has recently shown a similar result when adding IMM as salvage therapy to failing ADA in 23 patients with confirmed antibodies to ADA. Salvage therapy with IMM was associated with elimination of antibodies to ADA, increased ADA levels, and recapturing of response in 11 patients .
Ibd Often Responds To Combination Therapy
Pharmacy Times
Inflammatory bowel disease has complex treatment options, but pharmacists can help patients make the right choice.
Inflammatory bowel disease is a term that encompasses 2 conditions that are characterized by inflammation of the gastrointestinal tract: Crohn disease and ulcerative colitis.1
This prolonged inflammation can wreak havoc on the GI system.
Individuals of any age can get IBD, but it is usually diagnosed between aged 15 and 40 years.2
Crohn Disease
Crohn disease affects men and women equally, and the disease occurs in all ethnic groups. Although diet and stress can aggravate Crohn disease, they do not cause it.3
Ulcerative Colitis
If left untreated, the disease often relapses and remits mucosal inflammation. Most patients with ulcerative colitis experience a mild to moderate course. However, 20% of patients may require hospitalization for severe disease activity.4
Statistics
An estimated 1.3% of adults in the United States, or about 3 million people, reported receiving an IBD diagnosis in 2015. This was an increase from 1999 when just 0.9% of the population reported having IBD. These estimates do not include children under aged 18 years who receive an IBD diagnosis.5
Also worth noting, compared with patients without IBD, patients who have the disease are more likely to have certain chronic health conditions, such as arthritis, cancer, cardiovascular disease, kidney disease, liver disease, migraines or severe headaches, and respiratory disease.5
Also Check: Foods To Eat When You Have An Ulcer
Combination Therapy In Children With Ibd
At the moment data on the effectiveness and safety of taking biologics and immunosuppressants in children with Crohns disease and ulcerative colitis is more limited10.
Due to this lack of research the use of combination therapy in paediatric patients with IBD is left to the treating doctor to balance, with a suggestion of withdrawing the immunomodulator after six months if optimum therapeutic drug levels of this drug have been reached11.
Combination Therapy In Ibd
In IBD, data on combination therapy thus far are mainly from retrospective cohort studies or case reports. A recent review found that in all studies to date, combination therapy had positive outcomes, with only one study reporting an increased risk of infection.
Specifically, a retrospective cohort study investigated the use of combination biologic or small molecule therapy in 50 patients with either IBD in remission and continued joint or skin inflammation or joint or skin in remission, but ongoing IBD activity. The study included a variety of combinations in UC and CD, most commonly with the base drug being vedolizumab. Results showed a significant increase in clinical and endoscopic remission rates with the introduction of combination therapy that was paralleled by improvement in biomarkers. Nothing atypical was observed in terms of safety.
Another retrospective cohort study described 22 refractory patients with CD for whom a second biologic was added sequentially. In the majority of cases the baseline biologic was vedolizumab or ustekinumab and add-on was mainly anti-TNF. The results showed a significant improvement in endoscopic, clinical, and biomarker outcomes, and 38% of patients remained on dual therapy at 1 year. Surgery was needed in 33% of cases and nothing atypical was noted in terms of adverse events.
To summarize the data available to date on combination therapy in IBD, possible combinations to consider are summarized in Table 2.
Read Also: Natural Remedies For Stomach Ulcers In Humans