Is Ulcerative Colitis Serious
Unfortunately ulcerative colitis, or UC as its often referred to, does have the potential to be a serious illness due to some of the complications it can cause.
However, its important to remember that most people with ulcerative colitis dont experience some of the more serious complications that can occur due to receiving effective treatment. To help minimise your risk of complications you should follow the treatment prescribed by your doctor.
Some of the things that can cause serious complications include
You May Like: What To Eat If You Have A Bleeding Ulcer
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
You May Like: What To Take For Ulcers
Your Uc Flare Management Plan
Your doctor may help you deal with a flare by changing your medications or offering new ones. Treatment of flares can include mesalamine products and usually a steroid, such as prednisone,” says Desi.
There are also some things you can do at home to temper a flare. These include:
During an ulcerative colitis flare, its recommended that you schedule regular visits to see your doctor, at least once every three months until the symptoms go away. After the flare has subsided, physicians recommend one or two checkups a year to manage the disease.
When an ulcerative colitis flare strikes, you have options for getting your life back on track. Its important to learn what you can about maintaining your health and work with your doctor to find the best ways to safely control UC. And remember to always let your doctor know when new or persistent symptoms arise.
Recommended Reading: Treatment For Ulcerative Proctitis Flare Up
Give Yourself Some Tlc
Stress doesnât cause UC, but it makes symptoms and flares worse for some people. If it affects you, try meditation, breathing exercises, or a massage. You could also see a pro to try biofeedback, hypnotherapy, or a type of counseling called cognitive behavioral therapy, which helps you learn new ways to handle problems. Being active helps, too. Try yoga, tai chi, or other low-impact exercises like walking.
You May Like: What To Do For Ulcerative Colitis Flare Up
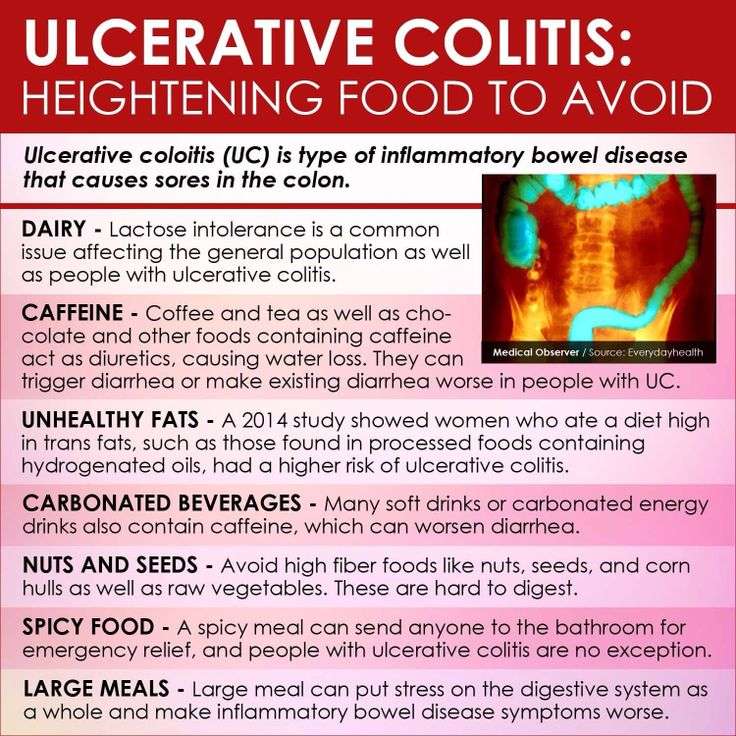
Number : Follow An Elimination Diet & Test Each New Food
This should be where you start.
The food list should be small initially.
It should comprise no more than 3-5 foods and should also be very minimal on the supplement front.
Yes, 3-5 foods is very limited, but thats the whole point.
This is so that your immune system does not have many potential triggers to react to.
And so that as you gradually introduce foods, you can work out what your triggers are.
Pick nutrient dense foods and/or add a multi-vitamin in the beginning to avoid any nutrient deficiencies.
There are many types of elimination diet.
Some of the main ones that people will use to stop an ulcerative colitis flare up are:
- A carnivore diet
Ive used all of these with my clients with good success.
There are others, of course, but these are the main ones.
As far as which specific foods to consume, stating the obvious, I cannot be more specific without knowing the dependences listed in the section above.
That being said, for the testing:
1. Consume 1 x serving of the new food you are testing once per day for 4 days.
Only test 1 new food at a time.
Be sensible with serving sizes if you are unclear on what a sensible serving size is, eat 0.5-0.75 cups of the specific food.
You can increase the serving size over time.
The new food can be consumed with other foods that youve already tested and marked as safe.
Which foods to test and in which order is dependent on your
- dietary preferences
Recommended Reading: Do Ulcers Make You Bloated
Also Check: How To Dress A Diabetic Foot Ulcer
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medication such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. However, more severe flare-ups need to be treated in hospital to reduce the risk of serious complications, such as the colon becoming stretched and enlarged or developing large ulcers. Both of these can increase the risk of developing a hole in the bowel.
If medications aren’t effective at controlling your symptoms, or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
Read more about:
How Is It Evaluated And Diagnosed
Your health care provider will evaluate rectal bleeding by asking questions, performing a physical exam, and doing some tests.
Your provider may ask questions such as:3,4,8
- What are your bowel movements like?
- Have you had any recent changes in bowel habits?
- Are your stools black or bloody? How often does this happen?
- Have you noticed blood on the toilet paper?
- Have you vomited recently? What did it look like?
- Have you had a recent colonoscopy?
- Have you had any recent trauma to the abdomen or rectum?
- What medications are you taking?
- Do you have a history of digestive or blood diseases?
- Have you been treated for prostate or pelvic cancer?
- Has anyone in your family had colon cancer?
- Have you experienced changes in weight recently?
Your health care provider may want to look at your stool.4 If you are in the hospital, you may be asked to use a special toilet or bedpan. If you are at home, your provider will instruct you on how to collect a sample.
Also Check: Signs Of Ulcerative Colitis Flare Up
Recommended Reading: Generic Drugs For Ulcerative Colitis
Tips On How To Stop A Flare
Learning how to stop, manage, or decrease symptoms during a flare-up can help improve the quality of life of people with UC.
Although managing flare-ups is important, knowing what can trigger a flare-up can help stop one from happening in the first place.
Some of the following strategies may be helpful to implement.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Recommended Reading: Drugs To Treat Ulcerative Colitis
Make Time For Activities That Make You Happy
Tip number three to help you prevent an ulcerative colitis flare-up: Always make time for things that make you happy. For me, its dancing. I have been taking dance classes since my pre-school years and continues to do so to this day. Its wonderful exercise, I have met amazing friends through this hobby, and it is also my favourite form of exercise. When I am in the dance studio, I forget about everything else in the world and focus on being in the present. So, whether it be dance, a sport that you love, or something as beautiful as painting, make time to feed your hobbies with your time and hopefully you will feel more fulfilled and less stressed!
How To Stop Ulcerative Colitis Bleeding
During an ulcerative colitis flare-up, one of the most common and most concerning symptoms is increased blood when passing a stool. This can often come with increased mucus production.
Due to the irritation and inflammation along the gut lining, reducing the fibre content of the food can be helpful. This can reduce irritation along the gut.
When preparing food it may be helpful to remove stems and skins from fruits and vegetables as well as ensure these are well cooked and perhaps pureed to a smooth texture. Other high-fibre foods such as popcorn as well as nuts and seeds may also be limited to reduce the irritation along the gut wall.
Also Check: Mouth Ulcer On Tongue Remedies
Recommended Reading: Fish Oil And Ulcerative Colitis
Ulcerative Colitis Inflammation And How To Prevent It
Inflammation is one of those hot topic terms for diet and health. One of those words that gets thrown around all the time by health professionals, commercials, and wellness products. You know you should be avoiding it, and perhaps you know that there are foods and behaviors that help reduce it, but what is inflammation, why does it happen, and how is it related to ulcerative colitis?
Ulcerative colitis is a disease that affects the large intestine or colon. It is defined by the irritation and swelling caused by inflammation. In fact, its considered to be an inflammatory bowel disease. Unfortunately, theres currently no cure for ulcerative colitis, but the right treatments and lifestyle behaviors can help you feel like you have a handle of the condition. Reducing or preventing inflammation is a major step in improving the symptoms and suffering associated with ulcerative colitis.
Antibiotics & Gut Health In Ibd
Antibiotics target unwanted and damaging bacteria, but healthy gut bacteria get caught in the line of fire, leading to an imbalance of our gut microbiome known as dysbiosis.
Our gut microbiome is home to trillions of bacteria, archaea, microeukaryotes, and viruses, making up a fragile ecosystem that plays a critical role in our adaptive immune system, energy homeostasis, and the nutrient breakdown and metabolite production. It regulates nearly every aspect of our health but when thrown out of balance, the reduced bacterial diversity can lead to the development of many diseases, including IBD, obesity, type 1 diabetes, and colorectal cancer.
This may explain why antibiotics have been reported to cause flare-ups in IBD cases. Broad spectrum antibiotics reduce microbiota diversity, and this not only increases the risk of IBD but can exasperate symptoms of an existing condition.
Recommended Reading: What Foods Irritate Stomach Ulcers
Medications And Other Uc Triggers
Apart from antibiotics, there are some other medications that should be used with care, or altogether avoided, when managing UC.
Nonsteroidal anti-inflammatory drugs can cause flare-ups, so its best to avoid ibuprofen and naproxen, which can make bleeding worse.
As for medications commonly used to treat UC itself, many have side effects so its worth knowing as much information as possible and discussing with your healthcare team.
What Causes Inflammation
Put simply, inflammation is the way your body reacts to injury or infection. Your body has its own military equipped with white blood cells and other helpful chemicals. You can consider them your healthy troops. When there is a threat, your body sends these helpful soldiers to visit the site of invasion and defend you.
The threat is typically caused by a foreign organisms such as a virus, bacteria, or from injury. Think about that time you embarrassingly fell and scraped your knee. Do you remember the redness, swelling, and heat, and sensitivity? These are aftereffects of your body trying to defend you and get the healing troops to their line of duty. This reaction is acute inflammation, since it happens within minutes or hours after the incident.
Chronic inflammation happens when your body makes continual attempts to repair and contain a source of injury or infection over an extended period of time. This can last weeks, up to months. It can follow acute inflammation or be caused by an autoimmune disorder such as ulcerative colitis.
Don’t Miss: Iv Infusion For Ulcerative Colitis
Taking The Next Steps
Ulcerative Colitis can wreak havoc on your digestive system, causing pain and discomfort that, at first, may seem impossible to deal with.
Worrying after every meal can feel overwhelming and isolating if you have not set yourself on the path to avoiding this debilitating digestive upset.
Ulcerative Colitis can be controlled, and we know consistency and persistence are essential for long-term recovery.
Understanding the intricacies of this disease, how you can change your diet, and how you can seek help in this endeavor are the powerful points to note on your way to conquering Ulcerative Colitis.
Over 3,000 people have benefited from the knowledge and guidance of our professionals. We monitor cutting-edge studies and modify our practices in light of what has been found helpful in the medical field.
With the help of professional observation and strategy, you can expect long-term symptom relief, the prevention of problems, and an improvement in your quality of life.
Talking to a professional can help you improve your health and happiness, and services like OnPoint Nutrition’s online team of licensed dietitians are a great place to start.
Let us empower you to take the steps toward the better living you deserve.
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Also Check: Does Stelara Work For Ulcerative Colitis
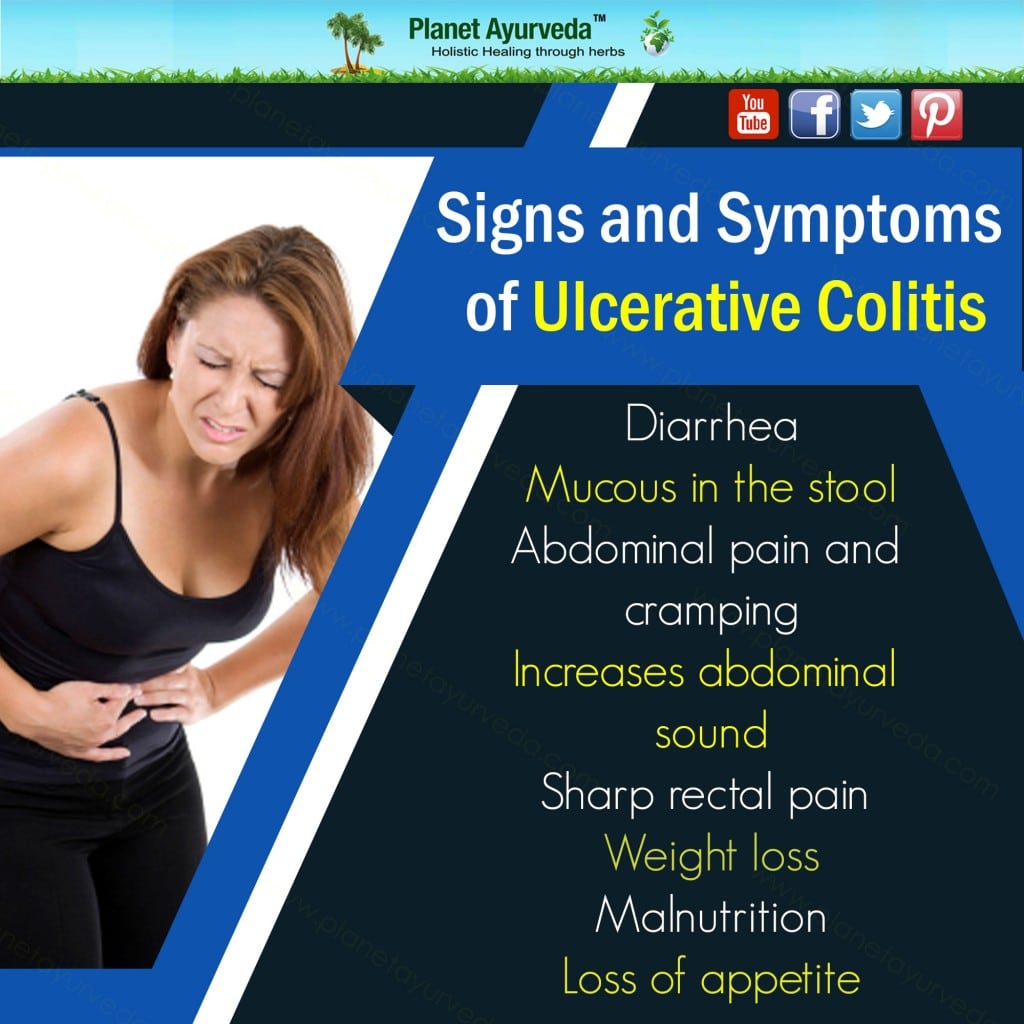
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Read Also: Removable Cast Walker Diabetic Foot Ulcers
What Are Ulcerative Colitis Flare
Ulcerative colitis is a condition which affects thousands of people across the UK. Luckily, many people with ulcerative colitis flare-ups receive advice and treatment, meaning the condition has minimal impact on their quality of life.
This doesnt mean flare-ups are completely avoidable though. Depending on whether you have proctitis, distal or total colitis, a flare-up may have different effects on the individual. Knowing how to recognise and manage these effects is very important.
In this short blog post, we will discuss what happens during a flare-up and how best to alleviate problems when it does.
Also Check: Wound Care For Stage 4 Pressure Ulcer
Ways To Stop Ulcerative Colitis From Flaring

Eleven years of living with ulcerative colitis has taught me several ways to stop flare ups. Most are natural and easybut one is a pain in the butt. Literally!
You want to stop ulcerative colitis from flaring for many reasons, including your summer vacation plans. You want to enjoy road trips without making pit stops every 10 minutes, right? Heres what Cynthia says about summer road trips and ulcerative colitis she blogs about living with inflammatory bowel disease .
For those of us with IBD/IBS the fear of not getting to a bathroom in time anywhere, at anytime is concerning enough but when we are in an unfamiliar territory it can be a tremendously anxious time. While everyone else is enjoying the trip and all that it entails, we may be panicking that we may not find a bathroom, in time! While everyone else is enjoying the sights, the smells, the food We are looking around for the nearest bathroom.
Ugh Ive always made it to the washroom in time, but Ive some close calls.
If you have colitis, Crohns Disease, or other bowel issues, read Living with Crohns & Colitis: A Comprehensive Naturopathic Guide for Complete Digestive Wellness. Even if you have a gastrointestinal doctor, like I do, its important to understand and learn how to control IBD naturally.
I like that this book offers both a medical doctors and a patients perspective of inflammatory bowel disease and symptom management. The best of both worlds, yah?
Also Check: Vegetarian Diet For Ulcerative Colitis