Significance Of The Project
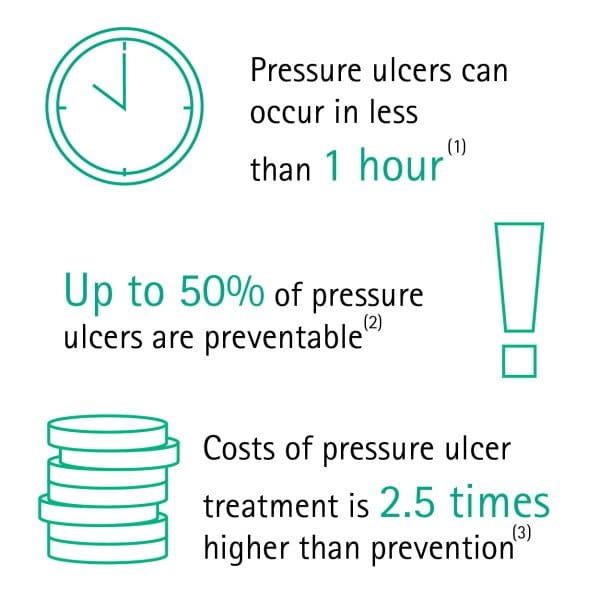
The project will significantly contribute to the current literature on the topic. It is expected that the DPI project will offer useful information to address the financial burden of HAPUs, which is discussed by Padula and Delarmente . Then, a massive body of literature that focuses on the preventable nature of pressure ulcers will also be enriched.
The project will stand together with the articles by Gray and Giuliano , Latimer et al. , Lin et al. , and others regarding this topic. Finally, the project will add to Rondinelli et al. and Lemmer et al. since it comments on effective interventions to reduce the HAPU incidence rate.
The project will also contribute to the literature on the theory of planned behavior. It relates to the fact that the project will answer whether specific measures of behavior control can promote the expected behavior, which refers to turning and repositioning every two hours. In other words, it will be shown whether Ajzens approach is a useful way to improve health outcomes and prevent HAPUs.
The project is also significant because addressing the problem will have practical value. On the one hand, the project has the potential to reduce healthcare expenditures on pressure ulcer management . It means that the government will have the opportunity to allocate these funds to address other essential issues.
Can Bedsores Be Prevented
Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas. Other methods of preventing bedsores and preventing existing sores from getting worse include:
- Turning and repositioning every 2 hours
- Sitting upright and straight in a wheelchair, changing position every 15 minutes
- Providing soft padding in wheelchairs and beds to reduce pressure
- Providing good skin care by keeping the skin clean and dry
- Providing good nutrition because without enough calories, vitamins, minerals, fluids, and protein, bed sores cant heal, no matter how well you care for the sore
Sample Of Materials Related To Elder Law
We sampled legal and policy materials such as cases, legislation, government reports, guidelines, regulations, and principles that were relevant to aged care and elder abuse. These materials broadly fall into an area of law called elder law. We also included secondary source commentary on the legal and policy documents that we subsequently identified. We reviewed these documents to assess the legal implications of two-hourly repositioning and the use of restraints.
You May Like: How To Prevent Sacral Pressure Ulcers
Purpose Of The Project
The purpose of this quantitative quasi-experimental project is to determine if or to what degree the implementation of turning and repositioning patients every two hours impacts the HAPU prevalence rate when compared to doing so once in four hours among hospitalized patients with a Braden Scale of less than 15 in medical inpatient units in Coney Island Hospital over six months.
The independent variable of turning and repositioning will be measured by identifying the frequency of these interventions turning and repositioning every two, three, and four hours are used today . The independent variable of the HAPU incidence rate will be measured by comparing the number of pressure ulcers before and after the intervention. These variables form the basis of the clinical question that guides the project.
Why Is Turning And Repositioning Important

A proper turn and repositioning reduces the chances of tissue breakdown and wound formation. If the tissue breakdown occurs on the outside of the body, a wound may develop. If the wound becomes infected, infection could spread. It is critical to avoid wounds whenever possible.
Repositioning For Success
There are a few things that must be done in order for repositioning to be successful. Before any business can be successful, it must first develop a business plan and commit to sticking to it. Following that, it is critical that the customer base approves of the changes. Furthermore, the repositioning must be carried out in a simple and effective manner that does not disrupt the customers routine. The following tips can help businesses improve their repositioning efforts.
Don’t Miss: Ulcerative Colitis Mouth Sores Pictures
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
Recommended Reading: How To Treat An Eye Ulcer
Key Points About Bed Sores
- Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period.
- Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile.
- Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas.
You May Like: Low Sulfur Diet Ulcerative Colitis
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Action Steps
How To Prevent Pressure Ulcers In Hospitals
Pressure ulcers can be prevented by adhering to simple guidelines in hospitals, where they are a serious problem. Make sure that your patients are properly positioned in bed and receive sufficient nutrition, as well as monitor their skin on a regular basis. In addition, mobility should be improved, as should the amount of pressure applied to patients.
Recommended Reading: Treatment For Skin Ulcers On Legs
How Often Should A Bed Bound Residents Be Repositioned
A person who is bedridden or in a wheelchair should be repositioned or shifted at least once a day, according to various medical institutions, including Johns Hopkins and the Mayo Clinic.
Repositioning Patients: When, How Often, And Why
To determine whether a patient needs to be repositioned, several factors must be considered, including immobility and the patients age, weight, and health. Patients are generally advised to be repositioned every two hours while laying down, but this may vary depending on the circumstances of the patient. If a patient spends a lot of time in a wheelchair, the repositioning should occur every hour, for example.
How Can Friends And Family Help
Caregivers might sometimes provide too much help. For instance, they might turn someone over in bed although the person is actually still capable of turning over in bed themselves, perhaps with just a little assistance. It is better to only help as much as needed, so the person stays as independent as possible, helping to prevent pressure ulcers.
If you are caring for a family member at home or go to visit them in the hospital or at a nursing home, you can help them move short distances, for instance when taking a few steps to the table to sit down and eat.
If someone needs to lie in bed for a long time, a nursing care plan is usually made together with nursing professionals. This may include information such as how many times a day a person needs to be repositioned. It is important for everyone to make sure that the plan is followed properly. This also includes regularly changing diapers or incontinence pads.
You should tell the nurses or doctors immediately about any red or sore areas of skin. They can then take a closer look at the affected area. It is always important to take pressure off that part of your body.
Read Also: Can Ulcerative Colitis Go Into Remission
What Do The Australian Wound Management Associations Official Guidelines Say
Professor Geoff Sussman, Chairman of Wounds Australia, told HelloCare that the Australian Wound Management Associations Pan Pacific Clinical Practice Guideline for the Prevention and Management of Pressure Injury give the evidence based and the most widely accepted guidelines in the region for preventing pressure sores.
The key recommendations for prevention of pressure injuries for those who have been assessed as being at risk of developing them include:
- Add high protein oral nutritional supplements to a regular diet.
- Use a high specification reactive support foam mattress on beds, or active support mattresses as an alternative.
- Reposition patients to reduce the duration and magnitude of pressure over vulnerable areas, including bony prominences and heels.
- Frequency of repositioning will depend on the patients risk of pressure injury development, skin response, comfort, functional level, medical condition, and the support surface used.
Who Is Most Likely To Get A Pressure Ulcer
Anyone living in a care home can develop a pressure ulcer, but some factors make it more likely.
Risk factors include:
- Limited mobility or being unable to change position without help.
- A loss of feeling in part of the body.
- Having had a pressure ulcer before, or having one now.
- Not having eaten well for a period of time.
- Thin, dry or weak skin.
- A significant cognitive impairment.
Recommended Reading: What Are The Symptoms Of A Stomach Ulcer Uk
Why Is Turning So Important To Prevention Of Bed Sores
Turning is the universally acknowledged best method for bed sore prevention. Turning refers to repositioning a hospital patient or bedridden nursing home resident to relieve pressure on one area of the body. Turning can restore regular blood flow to an area, keeping the skin tissues healthy and alive and effectively preventing bed sores. It is a nursing staffs responsibility to turn patients who could be at risk of developing bed sores. Failure to do so could constitute elder neglect or medical malpractice.
Why do Bed Sores Form?
Bed sores form because of inadequate blood circulation. Blood circulation is what keeps the organs working and the body alive. Blood circulation is necessary for skin tissue growth and health. When something interrupts blood circulation in the skin, such as a buildup of pressure against the skin surface, it can be detrimental to the skins processes. Prolonged loss of blood circulation can lead to tissue damage, and eventually necrosis, or tissue death.
The Importance of Turning
Since interruption to blood circulation can cause a bed sore, maintaining circulation can prevent one. Turning helps an individual maintain proper blood circulation to all areas of the body especially bony protrusions that are more likely to develop bed sores. Turning can relieve pressure and restore blood flow in the skin of the heels and ankles, backs of the calves, buttocks, hips, back, shoulder blades, elbows, and the back of the head.
Client Reviews
Summary Of Studies Included In The Review
Clinical evidence profile: different positions for repositioning â semi recumbent position versus standard care .
9.2.1.1. Comparison between kinetic beds and conventional beds
Clinical evidence profile: kinetic treatment table versus standard care for pressure ulcer prevention.
9.2.1.2. RCT Narrative summary
The following study is summarised as a narrative because the outcomes were not appropriate for GRADE due to incomplete outcome reporting:
One study examining the effects of the 30° tilt position in reducing the incidence of non-blanching erythema compared to the use of 90° lateral and supine position reported that 5 out of 23 participants in the experimental arm were unable to tolerate the intervention. No data was provided for the individuals in the control arm.
Also Check: How Would You Know If You Have Stomach Ulcers
Recommended Change In Practice
Turning and repositioning of patient should be performed regularly in patients who are immobile. Most of the frequently used positions are lateral, prone or semi-fowlers. Patients, who suffer pain, have an increased risk of developing pressure injuries since they avoid moving. The nurse must ensure proper pain management so that turning will not cause any discomfort. They should also turn and reposition the patient regardless of the surface on which they are lying. It is important for the nurse to take care of the bony prominences, such as the pelvis, along with elbows, heels, and ankles. Massaging these sites ought to be avoided and rather pressure care can be introduced. Consulting a physiotherapist is important during the implementation and evaluation of turning and positioning .
Turning and repositioning, unlike pressure redistribution, is manual and requires sufficient nurses and caregivers engagements. With the advent of technology, there have been innovations, including continuous lateral rotation therapy and alternating pressure beds. These equipment-related changes in patients positions in bed automatically. Such inventions help to reduce the effort and time needed to turn patients in bed manually. However, they are not as effective as the manual turning because they do not remove the pressure from the skin at any given time .
Looking foressayresearch paperinterview essaycapstone projectcase study Get 15% off your first order. Code start15Order now
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Dont Miss: What Is A Good Diet For Ulcerative Colitis
You May Like: Signs And Symptoms Of Bleeding Ulcer
Myth #3 Turning Q2h Prevents Pressure Injuries
No other myth about pressure injury prevention is more half true than this one. Its not that turning every two hours doesnt work to reduce pressure injuries. The true part is that turning does work. Not turning leads pressure injuries. The untrue half is that turning every two hours works because we are doing every two hours. But time is not why it works. It works because we are removing pressure. The paradox is, if we dont do it right, we have to do it often.
What Are The Risk Factors For Bedsores
Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care. People with diabetes, circulation problems and malnutrition are at higher risk.
Read Also: Natural Ways To Heal Stomach Ulcers
What Are The Symptoms Of Bedsores
Bedsores are divided into 4 stages, from least severe to most severe. These are:
- Stage 1. The area looks red and feels warm to the touch. With darker skin, the area may have a blue or purple tint. The person may also complain that it burns, hurts, or itches.
- Stage 2. The area looks more damaged and may have an open sore, scrape, or blister. The person complains of significant pain and the skin around the wound may be discolored.
- Stage 3. The area has a crater-like appearance due to damage below the skins surface.
- Stage 4. The area is severely damaged and a large wound is present. Muscles, tendons, bones, and joints can be involved. Infection is a significant risk at this stage.
A wound is not assigned a stage when there is full-thickness tissue loss and the base of the ulcer is covered by slough or eschar is found in the wound bed. Slough may be tan, grey, green, brown, or yellow in color. Eschar is usually tan, brown or black.
Also Check: What Is A Decubitus Ulcer Why Does It Occur
Evaluation Strategies And Outcome Measures
Evaluation strategies and outcome measures are important in patient care as they enable health care providers to compare the care they provide and the results, determining the efficacy of the care. Evaluation is a part of the nursing process and, after every nursing care and management, it is important to evaluate the condition of the patient. Turning and repositioning the patient and use of pressure redistribution devices are both interventions put in place to prevent the occurrence of pressure ulcers. The first step in the evaluation strategies is the inspection of patients skin during every shift and more frequently applied for patients with increased risk of developing pressure ulcers. By performing this option, developing ulcers can be easily identified and proper interventions put in place. Such a circumstance will also help to assess whether the existing practice is effective when patients exhibit no signs of pressure ulcers on each assessment .
You May Like: Orange Juice And Ulcerative Colitis