Treatment Of Mouth Sores And Pain
Dental checkups before treatment, and especially before head and neck radiation therapy, can help prevent and minimize mouth sores. Dentists can help show you how to care for your mouth and can treat cavities or oral infections before cancer treatment starts. It’s important to talk to your cancer care team about the best treatment for your situation. Although more research is needed to find the best treatment plan to manage mouth sores and pain, some options might include good mouth care and mouth rinses, reducing treatment doses, cryotherapy, or laser therapy.
Types Of Mouth Ulcers
There are different types of mouth ulcers there are three main types which include the following:
How To Treat Mouth Ulcers
Mouth ulcers dont usually need to be treated, because they tend to clear up by themselves within a week or two.
However, treatment can help to reduce swelling and ease any discomfort. This may help if you keep getting mouth ulcers or your mouth ulcer affects eating and drinking.
Self care
Things you can do to speed up healing include:
- applying a protective paste recommended by your pharmacist
- using a soft toothbrush to brush your teeth
- using a toothpaste that doesnt contain sodium lauryl sulphate, as this may be irritating
- avoiding hard, spicy, salty, acidic or hot food and drink until the ulcer heals
- using a straw to drink cool drinks
- avoiding things that may be triggering your mouth ulcers see causes, below
Pharmacy medicines
You can get several types of mouth ulcer treatment from a pharmacy. Speak to your pharmacist about the best treatment for you. Options include the following:
Medicines from your dentist or GP
If necessary, you may be prescribed a course of stronger corticosteroids to help reduce pain and swelling, and speed up healing.
Corticosteroids are available on prescription as tablets, mouthwash, paste or spray, but are not suitable for children under 12.
Also Check: How To Self Treat An Ulcer
What Causes Mouth Ulcers
The exact cause of mouth ulcers is unknown. But there are several factors that can contribute to the development of these sores:
- Minor tissue injury from dental work, such as having a cavity filled.
- Accidentally biting your cheek or tongue.
- Allergic reaction to certain bacteria.
- Viral, bacterial or fungal infections.
How To Diagnose Throat Ulcers
When diagnosing a throat ulcer, a doctor will begin by performing a physical examination and evaluating the persons symptoms. They may then take a throat swab to test for bacterial or fungal cultures.
Depending on the suspected cause of the throat ulcer, a doctor may also order one or more of the following tests :
Don’t Miss: Numbing Mouthwash For Mouth Ulcers
Key Points About Herpangina In Children
-
Herpangina is an acute viral illness in children.
-
Common symptoms are small blister-like bumps or sores in the mouth and fever.
-
It is caused by a virus. The most common ones are coxsackie viruses A and B.
-
Treatment may include fluids and medicine for fever and pain.
-
Correct handwashing can prevent the spread of herpangina.
Ulcers With Other Causes
study from 2012 , H. pylori and NSAIDs are the most prevalent causes of peptic ulcers. However, a newer review in the Asian Pacific Journal of Cancer Prevention states that ulcers without H. pylori infection or NSAID involvement are increasing.
The study, which took place in Thailand, suggests that other factors such as alcohol, other infections, medications, or diseases including stomach and intestinal cancer, may be to blame.
Quickly treating peptic ulcers, especially bleeding peptic ulcers, is the best way to avoid complications. If a person does not seek treatment for the ulcers, certain conditions can arise, such as:
- Severe internal bleeding: This can lead to hemorrhaging and is a medical emergency.
- Perforation: This is when the lining of the stomach splits open. This rare and severe complication can lead to stomach bacteria infecting the lining of the abdomen. This is called peritonitis.
- Gastric outlet obstruction: This is when a scarred or swollen stomach ulcer stops food from getting into the digestive system.
You May Like: What To Eat During A Ulcerative Colitis Flare
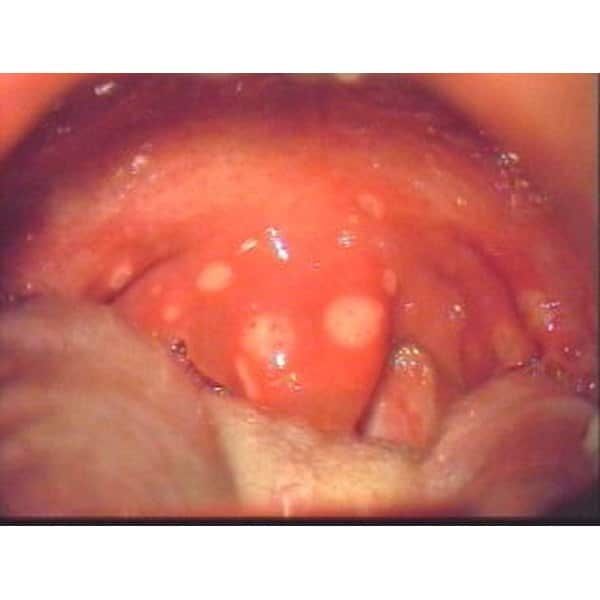
What Is Herpangina In Children
Herpangina is a sudden viral illness in children. It causes small blisterlike bumps or sores in the mouth. They are often in the back of the throat or the roof of the mouth.
Herpangina is often seen in babies and children younger than 10. It’s seen most often in the summer and fall. But it can occur anytime of the year.
Case Study: Tonsil Ulcer
In a case study published in 2020, researchers examined a 38-year-old male with COVID-19 who developed an ulcer on his left tonsil, among other symptoms. Heres how the symptoms developed:
- Day 1. The man developed fatigue and body aches.
- Day 2. He found he had a low-grade fever.
- Day 3. He developed a rash near his groin.
- Day 4. The rash spread and he developed a sore throat. Medical examination revealed redness and an ulcer on his left tonsil.
- Day 5. The man lost his sense of smell and taste.
- Day 6. The results of a swab taken on the fourth day came back positive for COVID-19.
The man didnt develop any respiratory symptoms and had only mild symptoms. Doctors prescribed Tylenol for the pain and recommended drinking plenty of fluids, resting, and social distancing.
Don’t Miss: Over The Counter Meds For Ulcers
New Onset Crohn’s Disease
Crohn’s disease is an inflammation of the bowel. It is caused by a faulty immune system response which makes the body attack the lining of the intestines.
The disease usually appears before age thirty and can affect anyone. Those with a family history may be most susceptible. Smoking is a known risk factor.
Aggravating factors include stress, poor diet, and nonsteroidal anti-inflammatory drugs such as ibuprofen and aspirin.
Early symptoms usually develop gradually, but can appear suddenly. These include fatigue, loss of appetite, fever, mouth sores, diarrhea, abdominal pain, and blood in stool.
Untreated Crohn’s disease can cause ulcers throughout the digestive tract as well as bowel obstruction, malnutrition, and deteriorating general health.
Diagnosis is made through blood test and stool sample test. Colonoscopy, CT scan, MRI, endoscopy, and/or enteroscopy may also be used.
Crohn’s disease cannot be cured, but can be managed through reducing the inflammation. Antibiotics, corticosteroids, and immune system suppressors may be tried. Excellent nutrition, vitamin supplements, smoking cessation, and reduction in stress can be helpful.
Rarity: Rare
Top Symptoms: fatigue, stomach bloating, loss of appetite, constipation, abdominal cramps
Urgency: Primary care doctor
How Are Mouth Ulcers Diagnosed
Your doctor can usually diagnose a mouth ulcer by simply looking at it.
Your doctor may also ask you questions about your symptoms, diet, medical history and what medicines you regularly take.
If your doctor thinks that your mouth ulcer is infected, they may swab the ulcer to confirm an infection and help determine the right treatment.
Recommended Reading: Things Not To Eat If You Have An Ulcer
Questions For Diagnosing The Cause Of Throat Ulcers
To diagnose your condition, your doctor or licensed healthcare practitioner will ask you several questions related to your throat ulcers, including:
- How long have you had your throat ulcers?
- Do you have any other symptoms?
- Have you had a cough? If you are coughing up mucus, what color is it?
- Are you having any congestion or difficulty breathing?
- Are you having difficulty swallowing or speaking?
- Have the glands in your neck felt swollen or tender to the touch?
- Have you experienced a fever or any chills?
- Have you had an earache or headache?
- Have you had any unexplained weight loss?
How Can I Prevent Mouth Ulcers

While you cant prevent mouth ulcers altogether, there are things you can do to reduce your risk. For example:
- Brush your teeth twice daily and floss once daily for optimal oral health.
- Use a soft-bristled toothbrush to avoid tissue irritation.
- Eat a healthy diet, rich in fresh fruits and vegetables.
- Visit your dentist regularly for checkups and cleanings.
If your healthcare provider determines that your mouth ulcers are connected to an underlying health issue, managing your condition can reduce the risk of ulcers returning.
Recommended Reading: What Is Crohn’s Disease And Ulcerative Colitis
What To Expect At Your Office Visit
The provider will examine you, and closely check your mouth and tongue. You will be asked questions about your medical history and symptoms.
Treatment may include:
- A medicine that numbs the area such as lidocaine to ease pain.
- An antiviral medicine to treat herpes sores.
- Steroid gel that you put on the sore.
- A paste that reduces swelling or inflammation .
- A special type of mouthwash such as chlorhexidine gluconate .
Sore Throat With Blisters & Ulcers: Coxsackievirus In Adults Or Kids
Most commonly, a sore throat with blisters or ulcers is due to a virus called coxsackievirus. Coxsackievirus causes a wide variety of symptoms, and while it typically affects children, adults can get it as well.
Symptoms of coxsackievirus include:
- Abdominal discomfort
Coxsackievirus can also cause several different conditions that affect different parts of the body, such as:
- Hand, foot and mouth diseaseHand, foot, and mouth disease is a viral illness that typically affects children under 5 years old however, it can sometimes occur in adults. Symptoms include fever, mouth blisters, and a skin rash.
- HerpanginaHerpangina is a contagious childhood throat infection that causes blisters and ulcers on the tonsils of the roof of the mouth.
- Hemorrhagic conjunctivitisHemorrhagic conjunctivitis is a highly contagious eye infection that causes eye pain followed by red, watery eyes with swelling, light sensitivity, and blurred vision.
Coxsackievirus is highly contagious, but children and adults often recover without treatment within a few days.
Other Causes of Throat Ulcers and Blisters
Coxsackievirus isnt always to blame for a sore throat with ulcers or blisters. Sometimes sores in the back of the throat white patches or red patches due to a virus like mono or bacteria like strep throat can be mistaken for these same symptoms. The only way to know for sure is to visit your local FastMed Urgent Care and be seen by one of our caring medical professionals.
Also Check: Low Dose Naltrexone Ulcerative Colitis
How Can I Tell If Throat Or Mouth Ulcers Are A Symptom Of Covid
Some case studies have reported people with COVID-19 developing ulcers in their mouth or throat. Its not clear whether COVID-19 directly causes ulcers or if it weakens your immune system and makes you more susceptible to developing other infections.
Ulcers of the mouth and throat are potential symptoms of many viral, bacterial, and yeast infections and are thought to be possible symptoms of COVID-19 infection, too. Its thought that infections are responsible for about of mouth ulcers, and theyre especially common in viral infections.
First, its important to recognize the most common reported symptoms of COVID-19, including:
So far, only a handful of case studies have reported people with COVID-19 developing ulcers of the throat.
More studies report people developing ulcers on their tongue, cheeks, lips, and palate. A review of studies in Dermatology Therapy found 22 cases of people with COVID-19 who developed aphthous ulcers.
Also known as canker sores, aphthous ulcers developed between 0 to 10 days after the start of COVID-19 symptoms. The most common sites were the tongue and lips.
A December 2020 review of studies found that advanced age and severity of COVID-19 infection are the most common factors that predict the severity of ulcers.
Its still not clear if COVID-19 directly leads to ulcers or weakens your immune system and makes you more vulnerable to secondary infections.
What Are Mouth Sores
Mouth sores are common ailments that affect many people at some point in their lives.
These sores can appear on any of the soft tissues of your mouth, including the lips, inside of your cheeks, gums, tongue, and floor and roof of your mouth.
Mouth sores, which include canker sores, are usually a minor irritation and last only 1 or 2 weeks. In some cases, they can indicate an infection from a virus, such as herpes simplex, or more severe causes, such as mouth cancer.
Sores in your mouth caused by a common or short-lasting condition such as:
- pemphigus vulgaris
Keep reading to learn about the causes and symptoms of mouth sores and how to recognize and get rid of them.
Read Also: Bleeding Ulcer Blood In Stool
Using Otc Pain Relievers
Using OTC pain relievers can relieve swelling and a sore throat, making a person more comfortable throughout the day.
In addition to using medications specifically for a sore throat, people can also use generic pain relievers, such as acetaminophen or ibuprofen.
Although some people use aspirin to relieve laryngitis symptoms, children should never use this medication. In children, aspirin can cause a potentially life threatening complication called Reyeâs syndrome.
There are two different types of laryngitis: acute and chronic. Infections and illnesses, usually an upper respiratory infection, can cause acute laryngitis. It tends to last for a few days, until the illness goes away.
Chronic laryngitis, on the other hand, occurs when it lasts for longer than 3 weeks .
Causes of chronic laryngitis include smoking, heavy alcohol use, GERD, exposure to irritating chemicals, and overusing or abusing the voice .
Laryngitis occurs when the larynx, or voice box, becomes inflamed or irritated. In most cases, the condition is short lived and easily manageable using home remedies.
If sore throat pain or laryngitis do not go away within using these remedies, it is best to see a doctor, as acute laryngitis usually resolves within this time.
A doctor can help determine if further diagnostic testing or prescription medication is necessary.
Shop for home remedies
Some of the home remedies listed in this article are available to purchase in stores, pharmacies, or online. These include:
Acute And Recurrent Infection
- Candida albicans infection: oral thrush in babies, elderly and debilitated
- Herpes simplex: primary or recurrent cold sores
- EpsteinBarr virus and cytomegalovirus
- Varicella-zoster virus: chickenpox or sometimes, shingles
- Various consequences of human immunodeficiency virus infection
- Secondary syphilis: snail track ulcers
You May Like: Good Foods To Eat With Stomach Ulcer
What Can Cause Throat Ulcers In Children
Herpangina is a viral illness that comes on suddenly in children. It causes small, blister-like sores at the back of the throat or on the roof of the mouth.
Herpangina usually occurs in the summer and fall, and it is most common in children ages 310 years.
It can cause symptoms besides throat ulcers, including:
Whats The Most Common Type Of Mouth Sore
Cold sores and canker sores are among the most common types of mouth lesions. About 20% of people will develop canker sores at some point in their lives. And while over half of Americans have been infected with the virus that causes cold sores, only 20 to 40% of people develop cold sores as a result.
You May Like: Classic Features Of Ulcerative Colitis
Sign Of Another Infection
If you or your child have several mouth ulcers, this can be a symptom of:
- hand, foot and mouth disease – a contagious illness that also causes a rash on the hands and feet
- oral lichen planus – a condition that causes a white, lacy pattern inside the cheeks
- thrush infection – a fungal infection that can cause white curd-like blisters
Causes Of A Sore Tongue And Throat
A sore throat is marked by pain, irritation, and scratchiness, which can be more noticeable when you swallow. If you experience swelling on the tongue and discomfort when eating or drinking certain foods , you may have a sore tongue. Some of the common reasons for a sore tongue and sore throat are:
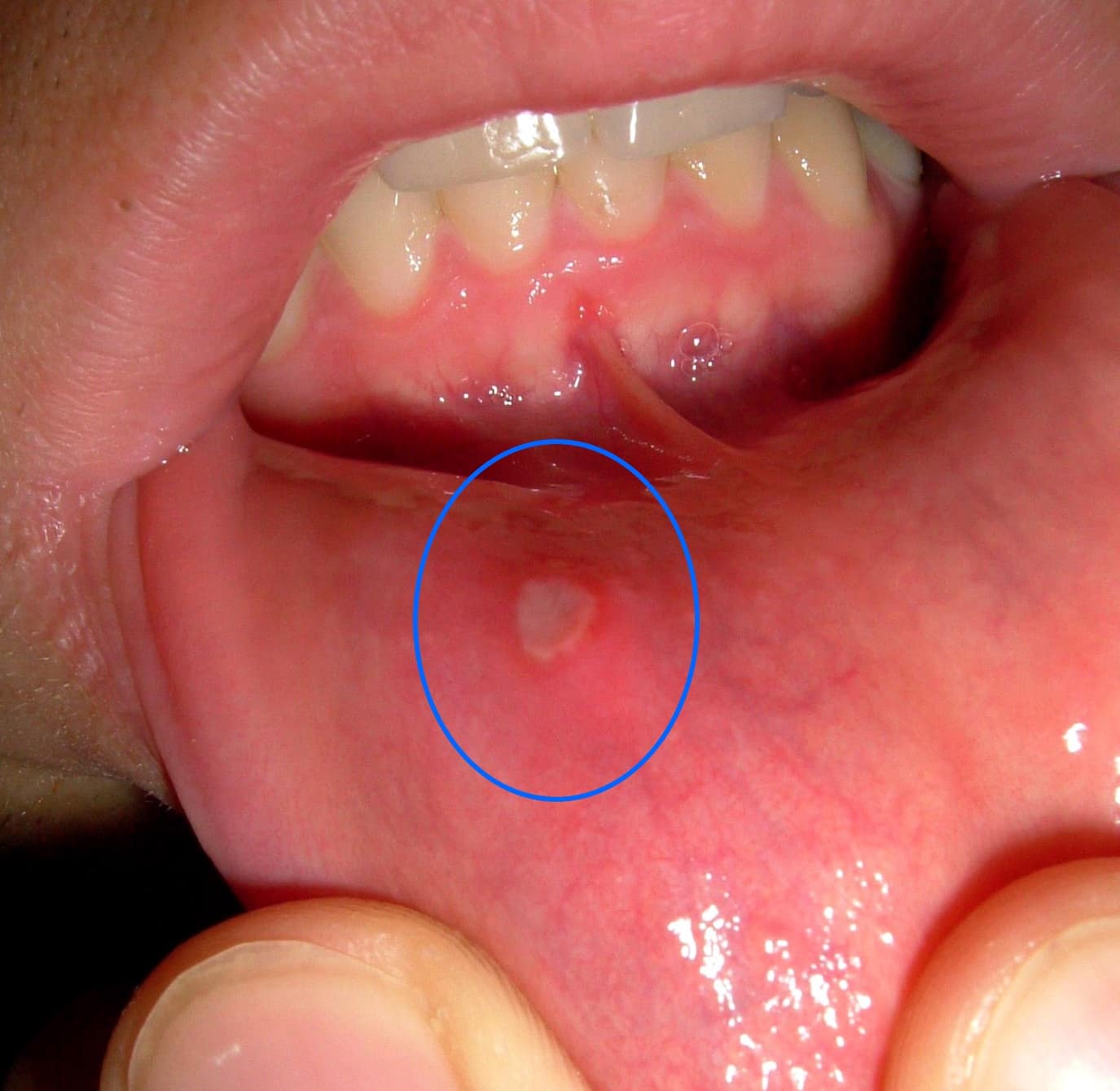
Mouth ulcers
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. Areas that can be affected include the tongue, inner cheeks, gums, and tonsil area. Mouth ulcers are white, yellowish, or grey in color and have a red border. If you experience a burning or tingling sensation on your tongue and throat, look inside your mouth to determine if there are any sores. The good news is that these will heal with minimal to no treatment. But if they persist or do not recover within 7-14 days, you should consult with your dentist or doctor.
Oral Thrush
Oral thrush, also known as candidiasis, is a condition that affects the tongue and throat too. The candida organism normally lives in the mouth, throat, and the rest of the digestive tract. An overgrowth of this organism can result in an infection. Symptoms include creamy white lesions on the tongue, inner cheeks that can spread to the palate, gums, and tonsils. You may also notice redness, a burning sensation, and soreness in the mouth and throat area that make eating and swallowing uncomfortable.
Burning Mouth Syndrome
You May Like: What Is The Best Pain Medication For Ulcerative Colitis