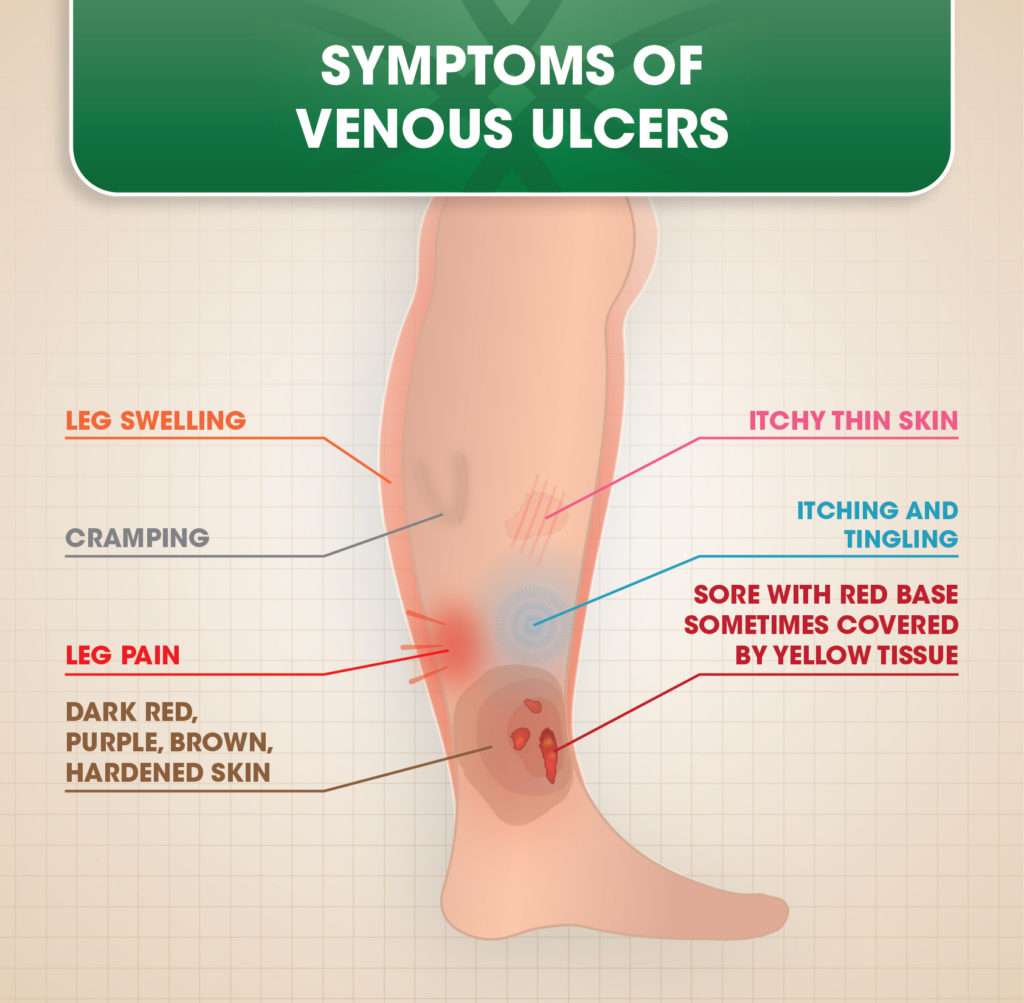
Common Signs And Symptoms Of Chronic Venous Insufficiency And Venous Leg Ulcers
- Venous ulcers are may be circumferential and are often located over medial malleolus or gaiter area of leg
- Ulcers are usually shallow and moist
- Edema may be pitting or firm
- Exudate from wound may be minimal or copious
- Skin changes may include hyperpigmentation, atrophie blanche, lipodermatosclerosis, dermatitis , woody fibrosis and corona phlebectatica
Table 2 – Signs and Symptoms of Venous Disease
How Venous Leg Ulcers Are Treated
Most venous leg ulcers heal within 6 months if they’re treated by a healthcare professional trained in compression therapy for leg ulcers.
But some ulcers may take longer to heal, and a very small number never heal.
Treatment usually involves:
- cleaning and dressing the wound
- using compression, such as bandages or stockings, to improve the flow of blood in the legs
Antibiotics may also be used if the ulcer becomes infected, but they do not help ulcers heal.
But unless the underlying cause of the ulcer is addressed, there’s a high risk of a venous leg ulcer coming back after treatment.
Underlying causes could include immobility, obesity, previous DVT or varicose veins.
Associated Changes In The Leg
4. Regular documentation to compare results before and after treatment and progression with time
5. Assess comorbidities like obesity, malnutrition, intravenous drug use and coexisting medical conditions prior to surgery. Reduced calorie and protein intake hampers ulcer healing
6. Rule out complications including severe infections, osteomyelitis and malignant changes .
7. If no improvement after 12 weeks or in case of recurrence or no response to treatment after 6 weeks: Reassess
Also Check: Peptic Ulcer Treatment At Home
C1 Disease Spider Veins Or Telangiectasias
Spider veins are usually classified as the first level in the grading system, C1 disease. These veins are the small purple, blue or red vessels close to the skin. Additionally, spider veins are very common such that over half the US population has spider veins.
Also called telangiectasias, spider veins, occur in both women and men. They are much more common on the lower legs than anywhere else on the body.
Many patients seek care for spider veins or telangiectasias because they do not like the appearance. This young woman sought care at Lakeshore Veins for the spider veins on her left thigh. These veins had no associated symptoms and were treated with sclerotherapy to improve the cosmetic appearance.
However, not all telangiectasias are treated for cosmetic reasons. This patient had underlying venous insufficiency and developed spontaneous bleeding. She noted a large amount of blood on the bathroom floor after stepping out of the shower. No trauma occurred in the area. Spontaneous bleeding after a shower can occur because the warmth of the shower causes the vessels to dilate and the skin to soften. Spider vein treatment can be covered by insurance if symptoms are present. It is important to seek medical advice if you have symptoms.
Medical History And Examination
Your GP or practice nurse will ask whether you have any other symptoms associated with venous leg ulcers, such as:
- swelling in your ankles
- discoloured or hard skin
They’ll try to determine the cause of the ulcer by asking about underlying conditions or previous injuries, such as:
Read more about how venous leg ulcers are treated.
You May Like: How To Treat An Ulcer In Your Mouth
Can Leg Ulcers Be Prevented
To prevent and promote healing of ulcers:
- Avoid injury, particularly when pushing a supermarket trolley. Consider protective shin splints.
- Walk and exercise for at least an hour a day to keep the calf muscle pump working properly.
- Lose weight if you are overweight.
- Check your feet and legs regularly. Look for cracks, sores or changes in colour. Moisturise after bathing.
- Wear comfortable well-fitting shoes and socks. Avoid socks with a tight garter or cuff. Check the inside of shoes for small stones or rough patches before you put them on.
- If you have to stand for more than a few minutes, try to vary your stance as much as possible.
- When sitting, wriggle your toes, move your feet up and down and take frequent walks.
- Avoid sitting with your legs crossed. Put your feet up on a padded stool to reduce swelling.
- Avoid extremes of temperature such as hot baths or sitting close to a heater. Keep cold feet warm with socks and slippers.
- Consult a chiropodist or podiatrist to remove a callus or hard skin.
- Wear at least Grade 2 support stockings if your doctor has advised these. This is particularly important for the post-thrombotic syndrome, leg swelling or discomfort, and for long-distance flights.
- Have a vascular ultrasound assessment and consult a vascular surgeon to determine whether any vein treatment should be carried out.
- Horse chestnut extract appears to be of benefit for at least some patients with venous disease.
Swelling In The Legs And Ankles
Venous leg ulcers are often accompanied by swelling of your feet and ankles , which is caused by fluid. This can be controlled by compression bandages.
Keeping your leg elevated whenever possible, ideally with your toes at the same level as your eyes, will also help ease swelling. You should put a suitcase, sofa cushion or foam wedge under the bottom of your mattress, to help keep your legs raised while you sleep.
You should also keep as active as possible and aim to continue with your normal activities. Regular exercise, such as a daily walk, will help reduce leg swelling. However, you should avoid standing or sitting still with your feet down. You should elevate your feet at least every hour.
Also Check: Ulcerative Colitis And Anxiety Attacks
Venous Insufficiency Picture Summary
The picture guide of the clinical classification of venous insufficiency shows how the vein disease is categorized from the mildest to the most severe disease. There are many available treatments to address venous insufficiency. Therefore, it is important to discuss any symptoms or concerns with a health care provider or vein specialist near you.
C2 Disease Venous Insufficiency With Varicose Veins
Varicose veins are the large bulging veins under the skin usually in the legs. Often, varicose veins are symptomatic causing heavy, tired, sore, itchy legs. But, they can also be have no associated symptoms. Once present, varicose veins will not usually go away. However, varicose veins are not usually dangerous and usually only require treatment if symptoms are present.
Varicose veins can occur in the thigh as in this picture. Although, they can be present in the lower leg or both.
Varicose veins can occur in young patients as early as their teens. Additionally, varicose veins can be present in active patients with a normal body weight. Generally, there is a strong genetic cause to varicose veins. Therefore, you are much more likely to have varicose veins if your mother or father has varicose veins.
Sometimes the varicose veins can clot and cause pain. Note the redness in the calf of this patient who also noted a hard lump. Clotted superficial veins are called superficial thrombophlebitis or phlebitis for short. Mild phlebitis will usually resolve after several weeks. However, it is important to seek medical attention if the area of phlebitis is larger than 5 cm in size, is located in the upper thigh, or is getting larger. Additionally, consult a physician if you have any medical conditions that makes your blood clot abnormally . Patients with recurrent phlebitis should have an ultrasound to evaluate for an anatomical cause of the phlebitis.
Recommended Reading: What Causes Stomach Ulcers In Horses
Treatment For Leg Ulcers
- cleaning the wound using wet and dry dressings and ointments, or surgery to remove the dead tissue
- specialised dressings a whole range of products are available to help the various stages of wound healing. Dressings are changed less often these days, because frequent dressing changes remove healthy cells as well
- occlusive dressings ulcers heal better when they are covered. These dressings should be changed weekly
- compression treatment boosts internal pressure, using either elasticised bandages or stockings. This is particularly effective if multiple layers are used
- medication includes pain-relieving medication and oral antibiotics if infection is present
- supplements there is evidence that leg ulcers may heal faster with mineral and vitamin supplements, but only if the person suffers from a deficiency. Zinc, iron and vitamin C may be used
- skin graft is a surgical procedure, where healthy skin is grafted onto the prepared wound site
- skin cancer and infection if ulcers fail to heal or if they increase in size, both these conditions will need to be ruled out
- hyperbaric oxygen this is now an accepted treatment for ulcers that resist other methods of healing, such as diabetic ulcers.
Looking After Yourself During Treatment
To help your ulcer heal more quickly, follow the advice below:
- Try to keep active by walking regularly. Sitting and standing still without elevating your legs can make venous leg ulcers and swelling worse
- Whenever you’re sitting or lying down, keep your affected leg elevated with your toes level with your eyes
- Regularly exercise your legs by moving your feet up and down, and rotating them at the ankles. This can help encourage better circulation
- If you’re overweight, try to reduce your weight with a healthy diet and regular exercise
Read more about preventing venous leg ulcers.
Recommended Reading: Corneal Ulcer Dog Home Remedy
Similar Articles Being Viewed By Others
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
21 November 2022
D. M. Anisuzzaman, Yash Patel, Zeyun Yu
19 April 2021
Yoo Jin Choo, Jeoung Kun Kim, Donghwi Park
08 November 2021
Dylan M. Richards, MacKenzie J. Tweardy, Stephan W. Wegerich
volume 12, Article number: 17962
How To Heal Venous Leg Ulcers
This article was co-authored by . Marsha Durkin is a Registered Nurse and Laboratory Information Specialist for Mercy Hospital and Medical Center in Illinois. She received her Associates Degree in Nursing from Olney Central College in 1987.There are 7 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 90% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 29,804 times.
A venous skin ulcer is a shallow wound that occurs when veins dont return the blood back to the heart the way theyre supposed to. These ulcers usually form on the sides of the lower leg, above the ankle, and below the calf. They can heal over time with proper care, but without it, they can return and/or cause serious complications. It’s very important to see a doctor or wound care nurse when you have an ulcer, then to keep them dressed and bandaged, take the right medications, and alter some of your habits at home.
Recommended Reading: How Do I Get Rid Of A Stomach Ulcer
What Is The Treatment For Leg Ulcers
Where possible, treatment aims to reverse the factors that have caused the ulcer. As an ulcer is often the result of both arterial and venous disease, careful assessment is needed first.
Venous leg ulcer, in the absence of arterial disease, is usually treated with exercise, elevation at rest, and compression. Compression must not be used if there is significant arterial disease, as it will aggravate an inadequate blood supply. Surgery, ultrasound-guided sclerotherapy or endovascular laser treatment of superficial and perforator leg veins may also help, particularly if the deep venous system is intact. Venous-return assisted calf compression devices may be of additional benefit.
A vascular surgeon should also assess patients with arterial leg ulcers as they may require surgery to relieve the narrowing of the arteries. Revascularisation is particularly important if the ABPI is less than 0.5.
It is also very important to treat underlying diseases such as diabetes and to stop smoking.
Risk Factors For Leg Ulcers
- Age peripheral circulation becomes less efficient with old age.
- Varicose veins the one-way valves that stop blood from travelling backwards in the vein stop working. The pooling of blood stretches and distorts the vein.
- Cigarette smoking tobacco is known to constrict the vessels of the circulatory system.
- Arterial disease vein problems are more likely if the person already has other diseases of the arteries.
- Certain disorders these include diabetes and arthritis.
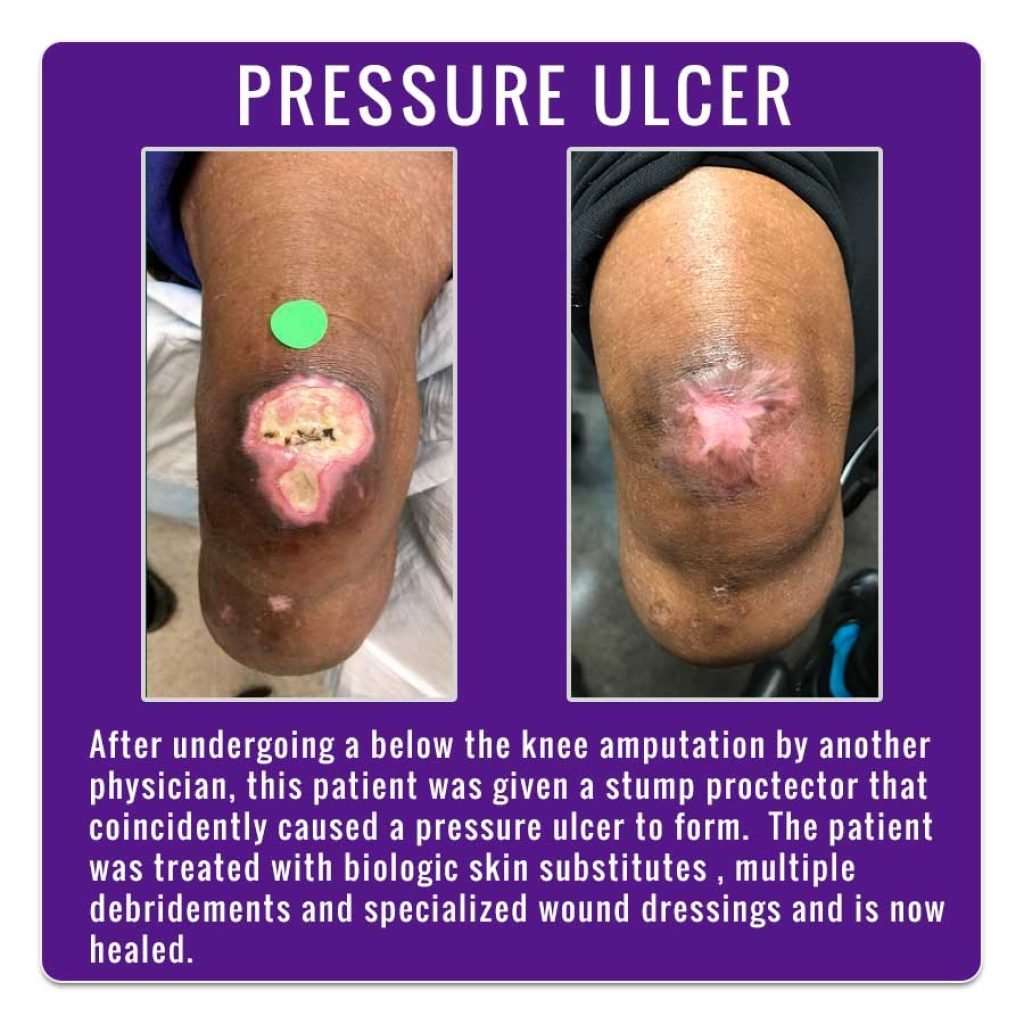
- Pressure sores bed-bound people are at risk of pressure sores, which are areas of damage to the skin caused by constant pressure or friction.
- Medication some cardiovascular medications can contribute to leg oedema and altered circulation.
You May Like: Natural Supplements For Ulcerative Colitis
Cleaning And Dressing The Ulcer
The first step is to remove any debris or dead tissue from the ulcer and apply an appropriate dressing. This provides the best conditions for the ulcer to heal.
A simple, non-sticky dressing will be used to dress your ulcer. This usually needs to be changed once a week. Many people find they can manage cleaning and dressing their own ulcer under the supervision of a nurse.
Diagnosis Of Leg Ulcers
- examine the wound
- perform some tests to measure the blood flow in your lower leg, such as the ankle-brachial index. This test compares blood pressure readings taken at the ankle and at the arm using a device called a Doppler machine
- recommend an angiogram for an arterial ulcer, to find out if the artery needs surgery to clear the blockage.
Also Check: Do Ulcers Hurt All The Time
Odds Ratio Of Venous Leg Ulcer Not Healing In 24 Weeks
Research demonstrates that several factors will influence whether the ulcer is going to heal, which include the initial size of the ulcer and the length of time that the ulcer has been present. For this reason, it may be prudent to ensure that there is a wound care specialist consult for all patients with venous ulcers that are > 5 cm² and/or if the wound is older than 6 months as these wounds will not generally heal with only moist wound healing, debridement and appropriate compression therapy.
Factors that may affect healing potential
Local
- Presence of necrosis, foreign body and/or infection
- Disruption of microvascular supply
- Cytotoxic agents
Host
- Adherence to plan of care by patient and caregivers
- Cultural and personal belief systems
Environment
- Wound base has more than 50% yellow fibrin
- Wound has been present longer than 6 months
- Wound is larger than 5cm²
- Patient had previous hip or knee surgery
- Patient has history of vein ligation or stripping
In addition, the practitioner must assess whether the person with the leg ulcer is willing to wear compression bandages and/or stockings to heal, and then to wear compression ongoing.
Other Types Of Leg Ulcer
Other common types of leg ulcer include:
- arterial leg ulcers caused by poor blood circulation in the arteries
- diabetic leg ulcers caused by the high blood sugar associated with diabetes
- vasculitic leg ulcers associated with chronic inflammatory disorders such as rheumatoid arthritis and lupus
- traumatic leg ulcers caused by injury to the leg
- malignant leg ulcers caused by a tumour of the skin of the leg
Most ulcers caused by artery disease or diabetes occur on the foot rather than the leg.
Page last reviewed: 16 November 2022 Next review due: 16 November 2025
You May Like: Heel Protectors To Prevent Pressure Ulcers
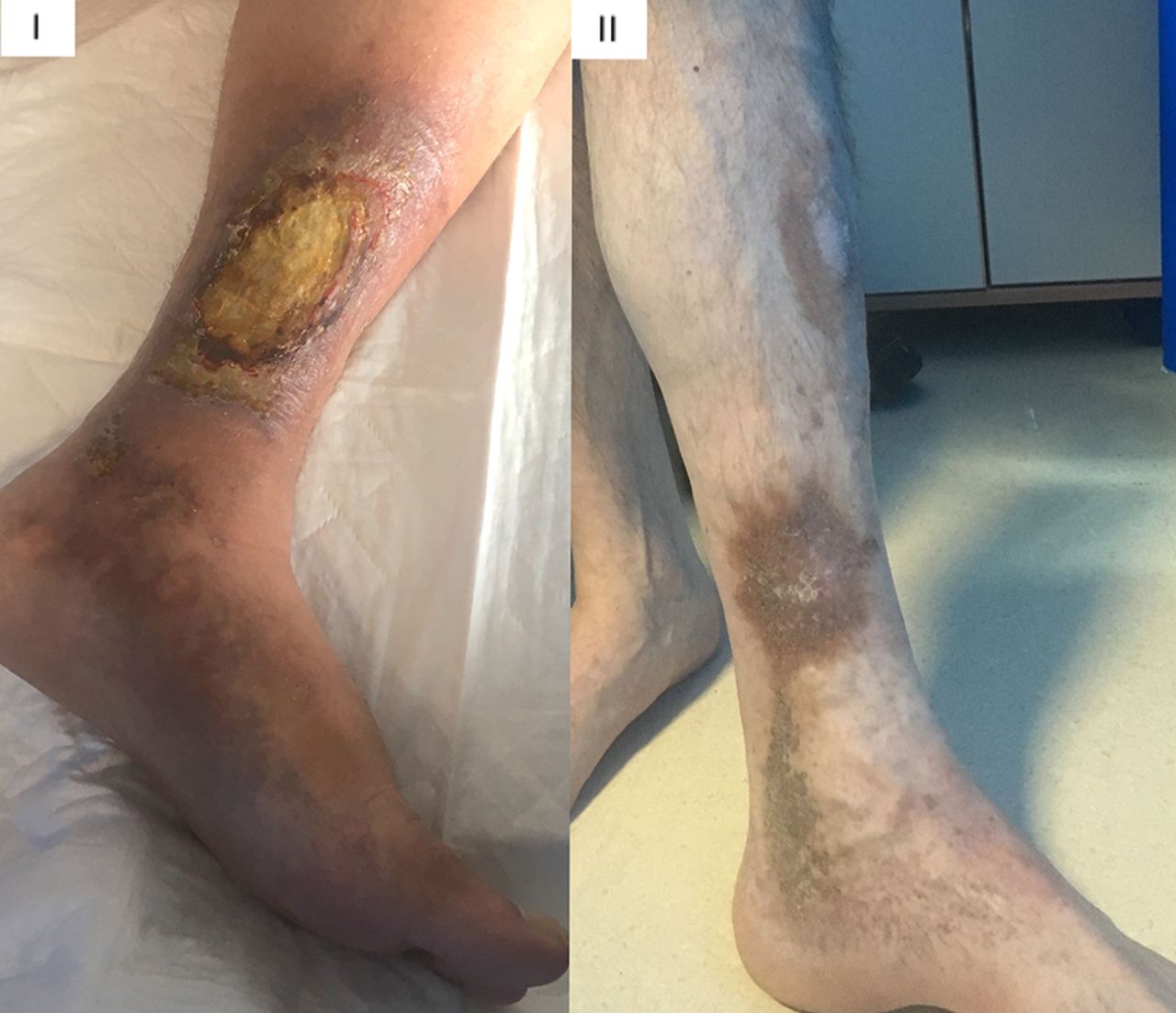
C5 Venous Insufficiency With Healed Ulcer
There are extensive venous stasis skin changes on the left leg with brown discoloration. The whiter region in the center of the brown are is in the region of the patients healed venous stasis ulcer. He was treated with ablation of his insufficient Great Saphenous vein and was able to heal a long-standing ulcer. Also, his ulcer has remained healed for several years.
Definition Rationale And Scope
Venous leg ulcers are defined as open lesions between the knee and ankle joint that occur in the presence of venous disease. They are the most common cause of leg ulcers, accounting for 60-80% of them. The prevalence of VLUs is between 0.18% and 1%. Over the age of 65, the prevalence increases to 4%. On an average 33-60% of these ulcers persist for more than 6 weeks and are therefore referred to as chronic VLUs. These ulcers represent the most advanced form of chronic venous disorders like varicose veins and lipodermatosclerosis.
Risk factors for development of VLUs include older age, female sex, obesity, trauma, immobility, congenital absence of veins, deep vein thrombosis , phlebitis, and factor V Leiden mutation.
You May Like: What Causes Ulcers On Your Lip
Referral To A Specialist
In some cases, your GP or nurse may decide to refer you to a specialist in conditions affecting the blood vessels .
For example, you may be referred to a vascular specialist if your GP or nurse is unsure about your diagnosis, or if they suspect your ulcer may be caused by artery diseases, diabetes or rheumatoid arthritis.
After taking your medical history and examining you, the vascular specialist may need to arrange further investigations to plan your treatment.