Popular Diet Plans With Patients
The Paleo Diet is another popular diet amongst patients with IBD. It recommends avoidance of processed food, refined sugars, legumes, dairy, grains and cereals, and instead it advocates for grass-fed meat, wild fish, fruit, vegetables, nuts and healthy saturated fat . While it makes sense that a diet that promotes avoidance of refined and extra sugars and processed energy dense food would have health effects, there are no clinical trials that have examined the efficacy of this diet for IBD. Randomized controlled studies are required to determine whether the Paleo diet has beneficial effects over other diet advice.
Can Food Cure Crohns Or Colitis
You may come across diets that claim to cure Crohns or Colitis, but there isnt any evidence to prove that these work. A healthy, balanced diet will give you nutrients that are important to help you stay well.Some people find that making small changes to their diet, for example avoiding spicy food, helps them cope with their symptoms. If cutting out a food makes no difference to your symptoms, make sure you start eating it again to avoid missing out on important nutrients.There are times when your IBD team or dietitian may advise you to change your diet, for example, after surgery or if you have a narrowing in your small intestine, called a stricture. Some people, such as children or people with Crohns, may benefit from a liquid diet, called exclusive enteral nutrition.Always speak to your GP or a dietitian before making any big changes to your diet.
Ive tried just about all the different diets for Ulcerative Colitis and just gone round in a complete circle, not finding any success, only causing problems and stress! I now realise the most important thing is to eat a balanced diet and enjoy my food!
Trevor
Should I Change My Diet During A Flare
During a period of active inflammation, any food can make pain, bloating, cramping, and diarrhea worse. However, you still need to eat during a flare. You also need to drink plenty of fluids with salt and water so that you absorb and retain fluid. Many people switch to a bland diet or to an all-liquid diet during a flare. Bland foods like rice, toast, bananas, applesauce, and nutritional drinks like Carnation® Instant Breakfast, Boost® or Ensure® can help.
A low-residue diet limits the amount of fiber and other material that cannot be digested as it passes through your small intestine. A low-residue diet reduces the size and number of your stools and helps relieve abdominal pain and diarrhea.
You May Like: How Do You Treat A Foot Ulcer
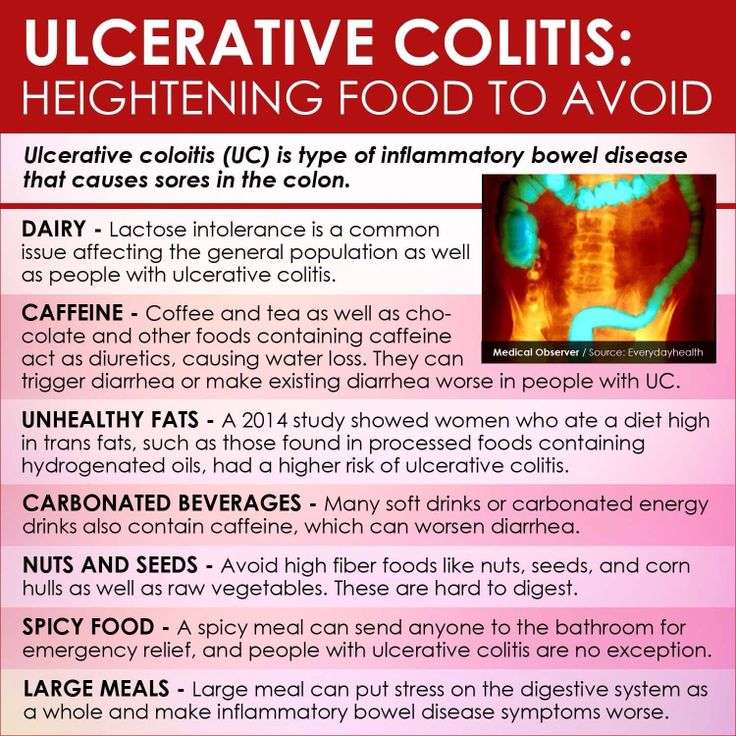
Foods To Avoid During Flares
Diet doesnt cause flares, but your food choices can make symptoms worse if your IBD becomes active.
How foods affect people who are flaring varies from person to person. But here are some of the foods that may worsen symptoms of a flare and cause complications:
- Beverages containing alcohol or caffeine.
- Sugar alcohols used to sweeten in sugar-free foods
- Raw fruits and vegetables
- Whole grain and high-fiber breads and cereals
- Fruits with seeds and skins
How Can I Track Foods That Cause Flare
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Don’t Miss: Pressure Relieving Mattress For Pressure Ulcers
Eating In Periods Of Remission
If youre in remission and your symptoms are light or even gone, give yourself the best chance at maintain that state by continuing to eat a nutritious and diverse diet. Consider the food you eat as the most powerful of medicines!
With all ulcerative colitis diets, we need to be sure work new foods in very slowly. Stay hydrated. Talk to your nutritionist, dietitian or healthcare professional before making any drastic changes to your diet, and of course, remember to keep up with your food journal.
These are examples of foods that may help you stay healthy, hydrated and in remission:
Inflammatory Bowel Disease And The Balanced Dinner Plate
All together, a familiar message is beginning to come through: a balanced diet that is rich in fruits, nuts, and vegetables, and not heavily based on certain types of meat might decrease an individuals risk for developing IBD and might also help those who already have it to limit the occurrence of disease flares.
Inflammatory bowel disease is a collective term for a number of intestinal conditions, primarily Crohns disease and ulcerative colitis. In the search for a fuller understanding of IBD, numerous recent studies have looked at the effects of specific foods on the development of the disease and management of its associated flares.1 Along the way, researchers have found that while some foods do appear to be associated with an increased risk of IBD and flares, others may actually have a protective effect.
Read Also: Total Contact Casting For Diabetic Foot Ulcers
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
Also Check: Stelara Dosing For Ulcerative Colitis
Eating During Remission From Uc
During remissionthat blissful time when your insides arent rioting against youyou may wonder if you can relax a little bit more about the foods you eat. In general, move slowly when adding new foods to your diet during remission. In fact, its best to do it one at a time so you can monitor any reaction. Otherwise, aim to hit the main points of a Mediterranean diet to get the nutrients you need. Your doctor or R.D. can offer more advice too. In the meantime:
-
Prioritize whole grains, non-cruciferous vegetables and low-fiber fruits, and healthy fats
-
Incorporate poultry, fish, beans, and eggs weekly
-
Add moderate portions of dairy if you can tolerate lactose
-
Limit your consumption of red meat
-
Limit processed foods
Also Check: What Kind Of Yogurt Is Good For Stomach Ulcer
Recommended Reading: How To Heal Ulcerative Colitis With Food
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Ulcerative Colitis Diet: What To Eat In A Flare Up
A low residue diet is often recommended to manage symptoms of ulcerative colitis. The Canadian Society of Intestinal Research outlines residue as the solid contents that stay in the bowel after digestion, with the goal of reducing the number of bowel movements that happen in a day. Residue includes fiber, which is limited to 10-15g per day, but the low residue diet differs from the low fiber diet by including foods that may stimulate frequent bowel movement, such as dairy, caffeine, alcohol and gristly or fatty meat.
Dr Deborah Lee, of Dr Fox Online Pharmacy, recommends the following foods for a low residue diet:
- Low fiber fruit and veg such as melon and bananas, as well as stewed fruit
- Lean protein such as white meat, eggs and tofu
- Refined grains such as white bread, white pasta and oatmeal
- Cooked seedless and skinless vegetables such as cucumber, potato and squash.
Cooking your food may also break down some of the dietary fiber to make it more digestible, as seen in a study in the journal of Plant Foods for Human Nutrition , which indicates that the process of cooking decreases the amount of insoluble dietary fiber in some vegetables.
- Related: 4 dairy free diet benefits
Read Also: What Foods Irritate An Ulcer
Foods To Eat With Colitis Flare Up
Since ulcerative colitis cause diarrhea, most experts recommend you to limit your fiber intake when you have colitis flare. However, it is good to replace high fiber foods such as nuts, seeds, raw fruits, and vegetables with more easily digestible diet.
Here are some foods to eat with colitis and the reasons how they can help.
1. Cooked Vegetables
For many people with ulcerative colitis, cooked veggies such as carrot and spinach can be a great source for getting important nutrients like Vitamins A and K.During a colitis flare-up, ensure that the carrots are cooked until they are soft and tender. Cooked carrots are not just easy to digest, but also contain antioxidants that may help ease ulcerative colitis symptoms.
2. Yogurt
Live and active culture yogurt can be a good source of protein if you have colitis flare. The probiotics in this form of yogurt have good bacteria that help ease gastrointestinal problems. Also, moderate amounts of dairy products will not lead to diarrhea but if milk causes bloating or stomach discomfort, turn to lactose-free milk.
3. Salmon
Salmon is good for colon which is rich in omega 3 fatty acids, have health benefits beyond the digestive tract and reduce inflammation. By adding salmon to the foods they eat, people with ulcerative colitis get more protein to their diet and ease symptoms of colitis flare-ups.
Try baking or grilling fish, as frying fish lose a lot of its nutritional value.
4. Applesauce
What Are Some High

Whole-grain breads, cereals, and pasta, whole vegetables and vegetable sauces, whole fruits, including canned fruits, yogurt, pudding, ice cream, or cream-based soups with nuts or pieces of fruits or vegetables, tough or coarse meats with gristle and luncheon meats or cheese with seeds, peanut butter, salad dressings with seeds or pieces of fruits or vegetables, seeds or nuts, coconut, jam, marmalade.
You May Like: How Do You Get Mouth Ulcers
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Read Also: What To Eat When You Have Ulcerative Colitis
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Canned Or Cooked Seedless Skinless Vegetables And Fruits
As mentioned above, its important to avoid high-fiber fruits and vegetables during a flare-up. However, its still important to give your body the nutrients it needs. For this reason, youll want to make sure that you eat plenty of cooked or steamed fruits without skins or seeds. You can also safely eat pureed soups and sauces made from vegetables.
Don’t Miss: How To Cure Colon Ulcers
Foods To Avoid With Ulcerative Colitis
Although there are foods that are common triggers during both Ulcerative Colitis flares and remission, the list expands when youre experiencing active Ulcerative Colitis symptoms. Keep in mind that Ulcerative Colitis triggers differ from person to person, so the real key to long-term Ulcerative Colitis management is identifying what works for you. Easier said than done, right?
If youve ever searched on your own to figure out how to manage your Ulcerative Colitis, youve probably found a ton of information. The challenge is that the information on the internet can be contradicting and confusing. If youre struggling with Ulcerative Colitis, we recommend enlisting the help of a registered dietitian. They will be able to help you better understand your UC and determine what foods and behaviors most trigger your symptoms.
Remember to limit fiber when you are experiencing an Ulcerative Colitis flare. High fiber foods are part of a healthy, well-rounded diet. However, when UC symptoms are active, you may need to temporarily limit fiber intake to reduce inflammation and allow your gut to heal. High fiber foods are harder to digest and can trigger UC symptoms. High fiber foods include whole grains, fruits with skin and seeds, vegetables with skin and seeds, raw vegetables, cruciferous vegetables, nuts, seeds, beans and legumes.
Treating Ibd And Anxiety
The study authors say it is important for physicians to determine whether patients with IBD also have a functional disorder. Differentiating symptoms between the two can be difficult, so they suggest that doctors first look for signs of inflammation, treat those, and then if symptoms remain it could indicate a functional disorder, at which point they should consider treatment for this disorder as well.
Physicians typically involved in caring for IBD patients, such as general practitioners and gastroenterologists, sometimes dont have much formal training in psychological disorders, and since patients are often hesitant to bring up psychological symptoms due to social stigma, they typically remain undiagnosed and untreated for too long. When IBD patients with an anxiety disorder experience stigma and therefore dont seek treatment, it can lead to further disability. It is very important that physicians are aware of the increased risk of anxiety in IBD patients, and should be prompt in detecting and treating any coexisting anxiety disorders. Patients also have a responsibility to speak up and ask for help if they perceive that anxiety is a problem for them.
If you are an IBD patient and are concerned that you might have anxiety or a functional gastrointestinal disorder, speak with your doctor.
First published in the Inside Tract® newsletter issue 195 2015
Email News Sign Up
Don’t Miss: Foam Boots For Pressure Ulcers
What To Eat During A Ulcerative Colitis Flare
Research shows that nutrition cant cause or cure ulcerative colitis. There are no foods that can cause someone to develop ulcerative colitis, and there is no miracle diet that will cure people of the condition. However, good nutrition does play an important role in the management of ulcerative colitis symptoms, especially during a flare.
Ulcerative colitis flare-ups are uncomfortable and frustrating. Pain, bloating, cramping, fatigue, rectal bleeding, and diarrhea are common symptoms during flare-ups. If youre in the midst of the flare, changes in your diet can help control your symptoms and allow your intestine time to heal. If you have a flare
While carefully watching what you eat can help ease symptoms of ulcerative colitis, there are very few treatments for ulcerative colitis currently available. Participating in research is one of the best ways to actively search for a cure. Research helps increase the understanding of ulcerative colitis and trial new treatment options.
If you or a loved one has ulcerative colitis, fill out the form below to learn more about a clinical trial that you may qualify for.