Managing Depression At Home
There are several things you can do at home to cope with negative feelings while you are getting treatment for depression.
Remember that feeling better takes time, and that your mood will likely improve gradually, not immediately. These tips have been adapted from the National Institute of Mental Health booklet on depression:
-
Set realistic goals, keeping your depression in mind, and take on a reasonable amount of responsibility in your daily life.
-
Set your priorities and break big tasks into smaller ones, doing the best you can to tackle them.
-
Make a point to spend time around other people. Confiding in a trusted friend or family member usually feels better than being alone and secretive.
-
Participate in activities that may make you feel better, such as mild exercise, seeing a movie, watching a sporting event, or participating in religious or social events.
-
Postpone major life decisions until your depression has lifted. These decisions may include changing jobs, getting married, or filing for divorce. Discuss important decisions with trusted friends or family members who may have a more objective view of your situation.
-
Dont expect to snap out of it. Instead, expect to feel a little better each day.
-
Ask for and accept help from your family and friends.
-
Know that positive thinking will eventually replace negative thinking as your depression responds to treatment.
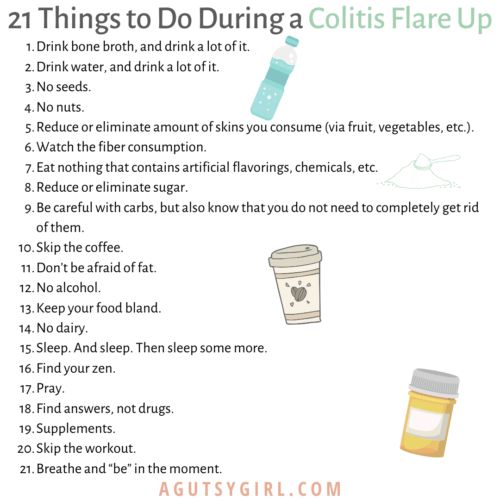
How To Prevent Ulcerative Colitis Flare
What are actionable steps you can take to make your symptom-free stretches last as long as possible? and stress management are probably the two biggest things as far as prevention goes, says Cohen. Parsley Health providers and health coaches often work with members who have ulcerative colitis to find a diet that helps them minimize flares and a stress management routine. Below, well dive into some specific ways to optimize your diet with natural remedies and make adjustments to your lifestyle while living with ulcerative colitis.
Read Also: What Should You Eat When You Have Ulcerative Colitis
How Long Do Flares Last
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment.
Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
The Crohns & Colitis Foundation recommends waiting to become pregnant until UC has been in remission for at least 3 months.
If you conceive during a flare-up, you may have more symptoms during pregnancy.
Youre likely to have a healthy pregnancy if you have UC, but youll still have a higher chance of complications than someone without the condition. Particularly if your UC is active, you may have a greater risk for:
In general, UC medications can be taken during pregnancy.
Talk with your doctor about any possible changes to your medications while pregnant.
Ideally, having a conversation with your doctor prior to getting pregnant can allow them to prepare a UC treatment plan in advance that can be revised, if and as needed, during your pregnancy.
Read Also: What Foods Irritate Stomach Ulcers
What Are The Symptoms Of An Ulcerative Colitis Flare
The main symptoms of an Ulcerative colitis flare-up include an increase in many digestive complaints.
These include:
- Bloody diarrhoea
- Abdominal pain that often improves after a bowel movement
The area of pain in the abdomen can be related to the region of the intestine that is inflamed. This can lead to a range of foods becoming more problematic and increasing the sensation of pain and discomfort in the gut. These are generally higher fibre foods that can increase symptoms during an Ulcerative colitis flare which include nuts, seeds as well as some fruits and vegetables
Before a flare in ulcerative colitis, symptoms can be stable but then increase gradually over a period of time which often leads to a flare-up.
Identify Daily Stressors And Put Your Health First
The second tip to help you prevent an ulcerative colitis flare-up is to ensure that you learn how to identify daily stressors so that you may eliminate them. Stressors for many people come up on a daily basis, whether it be work based, family based, or even relationship/friends based. I think that always keeping in mind that your health comes first no matter what. In other words, no issue is as important as your own health. By always keeping this in mind I find that it helps me mentally to filter things that brings stress instead of peace.
Recommended Reading: Foam Boots For Pressure Ulcers
You May Like: Can Ulcerative Colitis Cause Body Aches
Prevent An Ulcerative Colitis Flare By Following A Diet That Works For You
To prevent flare-ups, I think that all the stress management techniques combined with DIET make a huge difference for me. My amazing GI has talked to me about a diet eliminating as much sugar and refined carbs as possible. I will definitely talk more in-depth about diet and a breakdown of my diet in the future, but here are some diet based tips to help you prevent an ulcerative colitis flare
Make Less Stress A Priority
Another way to help prevent a flare or intercept one thats already begun? Destress. Theres a lot of research on the role of stress in this condition, Dr. Farhadi says. Like a recent study in Frontiers in Pediatrics where researchers found that stress might promote relapses in inflammatory bowel disease . In a stressful moment, have in mind that all measures to manage stress are very important, he says. He recommends finding your own best way to manage stress. The next slides offer a few options to try.
Also Check: How To Treat Stress Ulcers
Anxiety And Control Over Activities
Participants acknowledged a large amount of anxiety resulting from a pattern of their symptoms controlling their lives and the resulting effects of their disease on their quality of life.
Ive got a full-blown flareup, and uh, I try and schedule things around when Ive got to go to the bathroom in a half hour, so lets not start this meeting or lets get this meeting over, um, excuse me, Ive gotta go.
if I dont go in the morning, then its in the back of my head, Ok, whens it going to hit? But if I go in the morning, right after I get up, I have no worries the rest of the day.
You end up planning your whole life around what your gut is doing.
I mean, you plan your life around it .
When it started, I just had to stay home because so often I couldnt handle it and it had absolutely no control, and when you teach, you cannot have that in the classroom.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
You May Like: How Can You Get Ulcerative Colitis
Read Also: What Age Does Ulcerative Colitis Start
Acute Psychological Stress And Animal Models Of Ibd
As in humans, experimental models of psychological stress have been developed to allow the study of the role of psychological stress in animal models of IBD. A period of restraint stress or wrap restraint stress, where an animals movements are restricted by gentle binding, is the commonest technique used in the rodent to simulate acute stress. This can be combined with either a cold environment or partial immersion in water. The water avoidance stress, where an animal is placed on a small platform surrounded by water, is another model used for acute stress. Prolonged maternal separation is used to simulate chronic stress and depression. A confounding factor, which requires use of appropriate control groups in all animal experiments, is that routine handling is inherently stressful.
Chronic stress appears to render an animal with colitis more vulnerable to the effects of acute stress. Adult rats which underwent previous prolonged maternal separation and which were then subjected to a series of inescapable foot shocks, experienced a greater severity of dextran sodium sulphate induced colitis than did controls.
Probiotic For Ulcerative Colitis Flare
Probiotic supplements have been shown to help maintain longer periods of remission and also reduce the risk of a flare-up.
A probiotic supplement was prescribed to Ulcerative colitis patients who were not responding to conventional medical approaches. This led to a remission/response rate of 77% of the patients prescribed the probiotic with no adverse reactions reported.
Don’t Miss: Does Turmeric Help Ulcerative Colitis
How Common Is It
If you have UC and experiencing diarrhea, youre not alone.
According to the Crohns & Colitis Foundation of America, about 907,000 people are currently living with UC in the United States. Among them:
- 48 percent are in remission
- 30 percent have mild disease activity
- 20 percent have moderate disease activity
- 1 to 2 percent have severe disease
During a flare-up, a person with UC may experience more frequent bowel movements. They may find their stools to be loose and very watery.
According to Crohns and Colitis Canada, people who have extensive inflammation of the colon are more likely to have:
- persistent diarrhea and urgency
What Triggers An Ulcerative Colitis Flare

Triggers of ulcerative colitis flare-ups vary from person to person. It is helpful to identify factors that trigger or worsen your symptoms in order to try and avoid them. You may want to use a symptom diary or tracking app. Some of the most common include:
- **Diet. **Certain foods may trigger flares or worsen symptoms. Try to identify any foods that impact your ulcerative colitis.
- Medications. Pain relieving medications such as non-steroidal anti-inflammatories or antibiotics can worsen symptoms of ulcerative colitis
- Not taking medication as prescribed. Missing ulcerative colitis medications or taking an incorrect dose can lead to a flare-up.
- Stress. In some people, stress may impact ulcerative colitis symptoms.
Recommended Reading: What Is A Duodenal Ulcer And How Is It Caused
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medication such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. However, more severe flare-ups need to be treated in hospital to reduce the risk of serious complications, such as the colon becoming stretched and enlarged or developing large ulcers. Both of these can increase the risk of developing a hole in the bowel.
If medications aren’t effective at controlling your symptoms, or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
Read more about:
How Long Do Flare
UC is a condition that is unique to every individual. Some people experience flare-ups that last a few days, while others experience flare-ups that last weeks. Likewise, individuals may go from a mild flare-up to a severe one and then back again.
If a person is experiencing a severe flare-up that persists, they should speak with a doctor. The doctor will help them get their symptoms under control and improve their quality of life.
You May Like: Over The Counter Drugs For Ulcers
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
When You’re In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Recommended Reading: Signs Of Having An Ulcer
Take Some Deep Breaths To Calm Your Gut
Breathing deeply can help reduce UC gut pain and cramping, says Sara Kinsinger, PhD, director of behavioral medicine for the digestive health program at Loyola University Health System in Maywood, Illinois.
Deep breathing elicits a parasympathetic relaxation response that physiologically helps the body relax by increasing blood flow and oxygen to the gut, she says.
Experiment with different deep breathing techniques, including diaphragmatic breathing and alternate nostril breathing, to learn what helps you relax.
Failure To Have A Gastroenterology Specialist On Your Side
Your primary care physician can only do so much for you. In order to adequately manage and treat your Crohns or ulcerative colitis, you will need to see a specialist for regularevaluation. In fact, you should have a whole team of doctors working for you, from surgeons to radiologists to nutritionists however, your gastroenterologist should be your main point of contact when it comes to your condition.
We treat patients with Crohns and ulcerative colitis as well as a variety of other gastrointestinal diseases, including colon cancer, hepatitis, biliary diseases, esophageal disorders, and peptic ulcer disease. Our specialists can offer you more tips on how to best manage your condition, and work with you one-on- one to develop a workable treatment plan.
Please note, the information provided throughout this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and video, on or available through this website is for general information purposes only. If you are experiencing related symptoms, please visit your doctor or call 9-1-1 in an emergency.
GET OUR FREE NEWSLETTER
Read Also: Can A Heating Pad Help Ulcerative Colitis
What Should I Eat During An Ulcerative Colitis Flare
There is no specific type of diet that has been proven to relieve symptoms in people with ulcerative colitis. However, you may find that particular foods make symptoms worse.
It is important to identify and limit any foods that lead to worsening of your symptoms. Keeping a food journal may help you track how your diet relates to your symptoms.
Some suggestions that may help during a flare-up include:
- Reduce dairy products containing lactose
- Avoid high-fat foods
- What remedies help during an ulcerative colitis flare-up?
In addition to taking medication as prescribed and eating a well balanced diet, maintaining a healthy lifestyle can be beneficial for managing ulcerative colitis. Regular exercise and mindfulness strategies have been shown to improve overall health and quality of life.
Arastéh, K., Baenkler, H. W., Bieber, C., Brandt, R., & Chatterjee, T. T. . Duale Reihe Innere Medizin. Georg Thieme Verlag.
Dignass, A., Preiß, J. C., Aust, D. E., Autschbach, F., Ballauff, A., Barretton, G., … & Jantschek, G. . Aktualisierte Leitlinie zur Diagnostik und Therapie der Colitis ulcerosa 2011Ergebnisse einer Evidenzbasierten Konsensuskonferenz. Zeitschrift für Gastroenterologie, 49, 1276-1341.
Elizabeth Oliver, PhD
Assessing Response To Medical Treatment
The FBC, U+Es, albumin, CRP and stool frequency should be checked on a daily basis. The AXR should be repeated daily if there is severe extensive colitis, dilatation on the previous AXR, fever, tachycardia or abdominal tenderness otherwise repeating it every other day will suffice. In patients without evidence of toxic dilatation and impending perforation, a decision to continue with standard therapy, to commence rescue therapy, or to proceed to a colectomy should be made by the consultant gastroenterologist in conjunction with a colorectal surgeon at the end of 72 hours of intravenous hydrocortisone. In patients who respond to standard therapy, intravenous hydrocortisone should be continued for a minimum of five days before switching to prednisolone 40 mg daily, which can be tapered by 5 mg every week provided the patient remains in remission. Furthermore, topical and/or oral 5-ASA therapy can be restarted or commenced once the patient is improving.
You May Like: Ulcer Of Esophagus Without Bleeding
Eye Problems Associated With Ibs
Since IBS is a chronic condition, there are some potential impacts on other parts of the body, including the eyes. These include the following:
- Light sensitivity
- Painful, red eyes
One survey found that eye problems occurred in 4 to 10 percent of people with IBS and seemed to be more common in Crohns disease than ulcerative colitis.
The list of eye conditions associated with IBS includes:
These conditions could develop before or after the diagnosis of IBS, but they tended to be associated with the onset of other symptoms.
Corticosteroids are the first choice for reducing inflammation associated with many autoimmune conditions, including IBS. These can help reduce swelling associated with parts of the eye too.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Dont Miss: Snack Ideas For Ulcerative Colitis
Don’t Miss: Is Constipation A Symptom Of Ulcerative Colitis