Natural Remedies For Ulcerative Colitis
The most effective way of treating ulcerative colitis is to consult a doctor.
But besides that, you can use natural remedies to alleviate the symptoms of this condition.
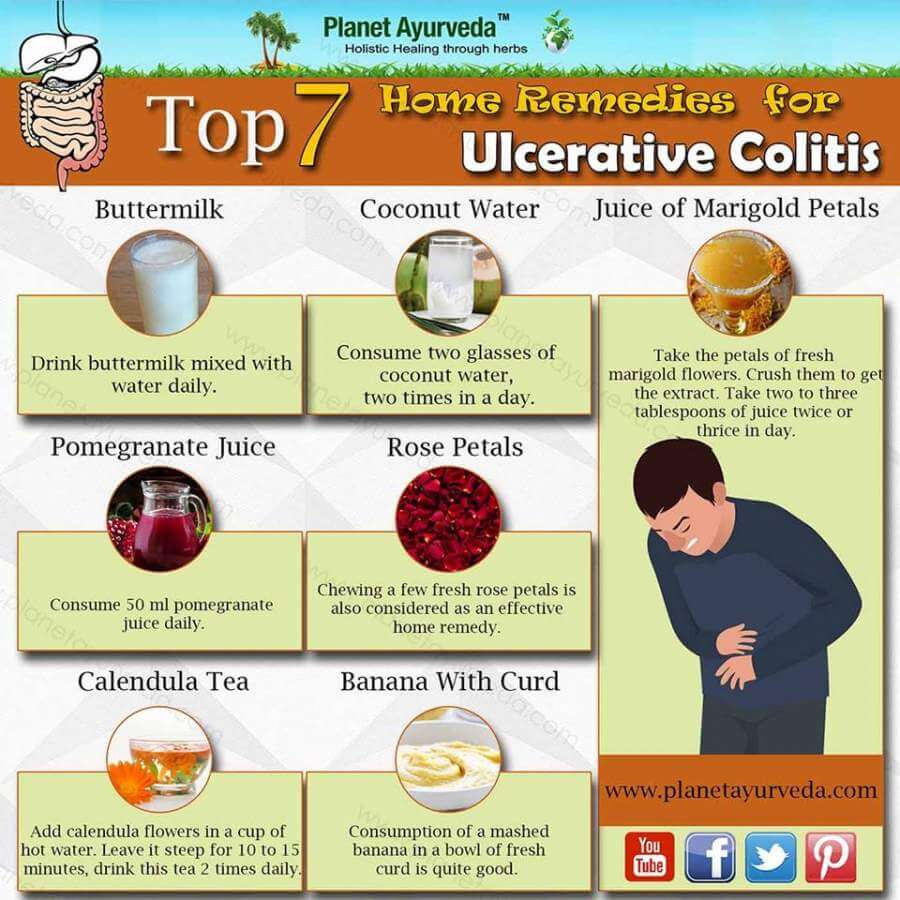
Remedies are usually taken orally and include drinking plenty of water to avoid dehydration, probiotics and fiber to restore the natural flora in your stomach, turmeric and ginger for their anti-inflammatory properties, and many other natural herbs.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
You May Like: Is Alcohol Bad For Ulcerative Colitis
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
Don’t Miss: Is Ulcerative Colitis An Inflammatory Bowel Disease
Avoid Food That Triggers Or Flares Up The Symptoms Of Ulcerative Colitis
- Insoluble fiber food: Exclude insoluble fiber food from the diet as they are very hard to digest like cruciferous vegetables eg. Broccoli, cauliflower, other raw green vegetables, fruits with seed and skin, whole grains, whole nuts, etc.
- Sugary foods: Avoid all kinds of sugary food like pastries, canned juice, candies, etc.
- Non- absorbable sugar: Avoid certain types of fruits and juices like prunes, peaches, pears, etc. Sorbitol, mannitol alcohols that are found in candies, ice- creams, etc.
- Spicy food: Avoid spicy food, pickles, etc.
- Alcohol and caffeinated drinks: Avoid wine, beer, liquor, soda, etc.
- Avoid high-fat foods like coconut, and butter, as well as greasy food, fatty, fried food.
Aahara And Vihara For Ulcerative Colitis
Aahara:
- At an appropriate time, when the patient feels hungry, he should be given light food to eat . This helps the patient to regain their appetite, his Agni gets stimulated, and strength is promoted immediately.
- In the initial stage, depending upon the wholesomeness, the patient should take light food along with buttermilk, Avanti-Soma or Kanji , Yavagu , Tarpana , wine, honey.
- Then gradually, the patient should be given Yavagu , Vilepi , Khada Yusha , and boiled rice mixed with meat soup, which is prepared by adding digestive stimulants and astringent drugs.
- If the patient is hungry, he should be given light food to eat. Peya prepared by boiling with appropriate drugs, or fried paddy or roasted-corn flour mixed along with water is also useful for him.
- The Manda can also be taken by the patient.
Vihara:
Vata gets aggravated soon, even by fear and grief , thats why Vatas mitigating factors are beneficial and it should be done by providing pleasure & courage to the patient as per the patients need.
Don’t Miss: Diabetic Foot Ulcer Treatment Ointment
Who Develops Ulcerative Colitis
About 2 in 1,000 people in the UK develop ulcerative colitis. It can develop at any age but most commonly first develops between the ages of 10 and 40. About 1 in 7 cases first develop in people over the age of 60 years. Non-smokers are more likely than smokers to develop ulcerative colitis. However, smoking brings other dangers to health which far outweigh this benefit.
How Do You Calm A Colitis Flare Up
Read Also: What To Use For Stomach Ulcer
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
Recommended Reading: How To Soothe Mouth Ulcers
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
You May Like: What Causes Tongue Ulcers In Adults
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
What Is The Prognosis For A Person With Colitis
Patients with infectious diarrhea tend to get better relatively quickly with supportive care. Most infections will resolve with or without specific treatment and often do not require antibiotics. Those decisions depend on the patients diagnosis.
Patients with inflammatory bowel disease probably will require lifelong treatment to help control their symptoms. The goal, as with any long-term illness, is to allow the patient to live a normal life with minimal symptoms from the disease.
Patients with ischemic colitis need to minimize their risk factors for progressive narrowing of the arteries. These are the same risks as for heart disease and require the same treatment approach, including controlling high blood pressure, diabetes, high cholesterol, and smoking cessation. Patients with severe ischemia that leads to a dead colon require surgery to remove the gangrenous segment.
Also Check: Zinc Oxide For Stage 2 Pressure Ulcer
How To Reduce Flare
While flare-ups often dont have a single, identifiable cause, several factors may contribute to them or make them worse, including:
- Missing your UC medications or taking the wrong dose
- Taking non-steroidal anti-inflammatory drugs or antibiotics
If flares occur even when a patient takes their medications as prescribed, it may be a sign that a change in medication type, dosage or frequency is needed.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Recommended Reading: Best Antibiotic For Strep Throat
You May Like: What Do You Do If You Have A Stomach Ulcer
Abbvies Rinvoq Granted Nice Recommendation As Ulcerative Colitis Treatment
The recommendation is for adults living with the condition in England and Wales
AbbVie has received positive Final Draft Guidance from the National Institute for Health and Care Excellence recommending Rinvoq , within its marketing authorisation, as a once-daily pill treatment for those with moderate-to-severely active ulcerative colitis .
The recommendation is specifically for adults with the immune-mediated inflammatory bowel disease, for whom conventional or biologic treatments cannot be tolerated, or for those who have found that the condition has not responded well enough or have stopped responding to treatments.NICEs decision is based on data taken from the induction studies, U-ACHIEVE and U-ACCOMPLISH, as well as the phase 3 U-ACHIEVE maintenance study and covers treatment access for patients in England and Wales. The three studies showed the efficacy of Rinvoq compared to placebo in its ability to achieve clinical remission at weeks eight and 52.
The recommendation allows for further access for UC patients across the UK, as the decision closely follows the Scottish Medicines Consortiums acceptance of Rinvoq in October 2022.
In the UK, UC affects approximately 300,000 people and the burden of disease is considerable because of the severity of the symptoms and uncertainty surrounding flares.
It is good news for people with ulcerative colitis that NICE has recommended as an additional treatment option that can be taken as a once-daily pill.
Article by
Bms’ Zeposia And Abbvie’s Skyrizi Shake Up First
Takeda’s Entyvio, Janssen’s Stelara, and AbbVie’s Humira leave the most on the table when first-line biologic or small molecule agents are prescribed in inflammatory bowel disease
EXTON, Pa., Nov. 30, 2022 /PRNewswire/ — US gastroenterologists estimate that just under 60% of their ulcerative colitis and 55% of their Crohn’s disease patients treated with a biologic or small molecule are on their first-line advanced systemic therapy. Over the past eighteen months, the US inflammatory bowel disease market has become increasingly competitive with the market entry of BMS’ Zeposia and AbbVie’s Rinvoq for the treatment of UC and AbbVie’s Skyrizi in CD, which have had material changes to new start IBD treatment patterns.
Spherix Global Insights has been tracking the newly initiated IBD patient segment for the past five years via their RealWorld Dynamix service. Data from the 2022 update, which includes analysis of 1,013 charts of IBD patients initiated on a biologic or small molecule therapy for the first time, reveals that TNF inhibitors are substantially less likely to be used first-line compared to prior years, while newer brands with alternative mechanisms of action have become increasingly popular.
Crohn’s disease new start patterns have also been altered by the newest CD market entrant, Skyrizi.
About RealWorld Dynamix
About Spherix Global Insights
To learn more about Spherix Global Insights, visit spherixglobalinsights.com or connect through and .
Also Check: Stage 4 Pressure Ulcer Dressing
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Ulcerative Colitis And Alcohol: Your Guide
When you have an inflammatory bowel disease like ulcerative colitis , dietary and lifestyle changes may become critical for managing your symptoms and preventing flare-ups. Although drinking alcohol isnt a risk factor for developing UC, alcohol use can sometimes damage the gastrointestinal tract and make existing symptoms worse. As one MyCrohnsAndColitisTeam member stated, I had three Angry Orchard ciders last night. It caused me to have loose stool and rectal pain after.
The decision to consume alcoholic drinks is up to you. Knowing the risks involved may help you make the best decision for your body and your UC.
Also Check: Best Cream For Leg Ulcers
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Read Also: Lionâs Mane Ulcerative Colitis
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Don’t Miss: Why Did I Get Ulcerative Colitis
Why Its Crucial To Act Immediately
If its not clear by now, this condition contains the word toxic because left untreated, toxic megacolon is potentially deadly. Dr. Murray underscores, Toxic megacolon is a potentially life-threatening condition that requires prompt diagnosis and treatment. Left untreated, toxic megacolon will eventually lead to these complications:
The bottom line, according to Dr. Murray: If you suspect you have toxic megacolon, you must take it seriously. When in doubt, you should get to the hospital or contact your gastroenterologist for further instruction. It can be difficult to distinguish toxic megacolon from other intra-abdominal conditionsevaluation by an emergency medicine physician can help determine if you do or do not have the condition, Dr. Murray says.
Avoiding Certain Pain Relievers
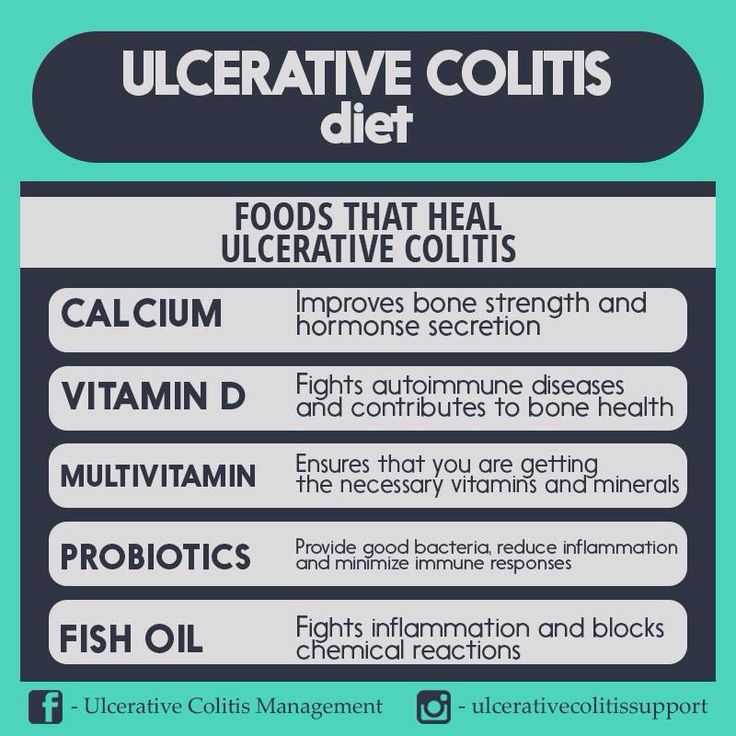
The authors also found that participants accessed health services less often after receiving vitamin D supplements.
Vitamin D supplements are available for purchase online.
Probiotics
Research from 2018 suggests that an imbalance in intestinal bacteria may cause the inflammation that occurs in people with UC.
In a meta-analysis from 2019, researchers found that people who took probiotics and an aminosalicylate had higher remission rates than those who only took an aminosalicylate.
Probiotics may help reduce UC symptoms by:
- preventing the growth of harmful gut bacteria
- regulating the immune system
- reducing inflammation in the colon
- improving the function of the intestinal barrier, which prevents toxins and harmful bacteria from entering the bloodstream
Probiotics are available for purchase online.
Curcumin
Some plants in the ginger family produce the chemical curcumin.
In a 2012 review , researchers investigated whether curcumin could help maintain UC remission.
Compared with the placebo group, fewer people who took curcumin experienced a relapse after 6 months. However, the results were not statistically significant, and confirming the benefits of curcumin will require more research.
Curcumin supplements are available for purchase online.
Prescription medications, as well as some lifestyle and dietary changes, can help people with UC maintain remission. A person is likely to benefit from:
- managing stress, when possible
- exercising regularly
- taking care to avoid food triggers
Don’t Miss: Anbesol Gel For Mouth Ulcers
Work With Your Doctor
Youâll need to see your doctor regularly. It may be every 6 months while youâre in remission. Youâll have routine procedures like colonoscopies and bloodwork to check on your UC.
If youâre having a flare-up, make sure to check in with your doctor. UC isnât the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Canât keep liquids down
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
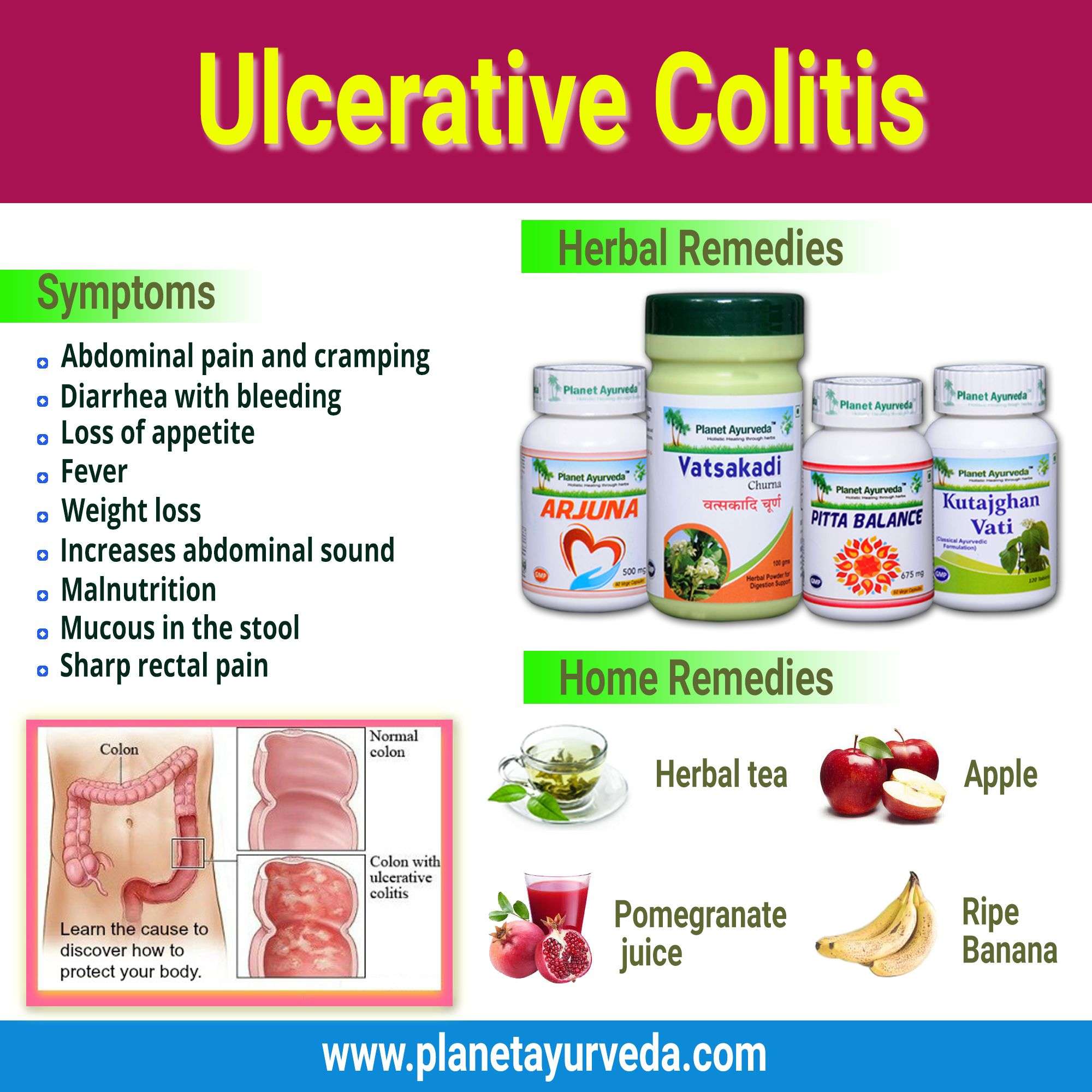
General signs of colitis can include:
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
You May Like: Bland Food Diet For Ulcers
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
Also Check: Nasal Cannula Pressure Ulcer Prevention