Appendix 6 Assessment Of Risk Of Bias
1. Was the allocation sequence randomly generated?
Low risk of bias
The investigators describe a random component in the sequence generation process such as: referring to a random number table using a computer randomnumber generator coin tossing shuffling cards or envelopes throwing dice drawing of lots.
High risk of bias
The investigators describe a nonrandom component in the sequence generation process. Usually, the description would involve some systematic, nonrandom approach, for example: sequence generated by odd or even date of birth sequence generated by some rule based on date of admission sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process provided to permit a judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation sequentiallynumbered drug containers of identical appearance sequentiallynumbered, opaque, sealed envelopes.
High risk of bias
Unclear
3. Blinding was knowledge of the allocated interventions adequately prevented during the study?
Low risk of bias
Any one of the following.
High risk of bias
Any one of the following.
Unclear
4. Were incomplete outcome data adequately addressed?
Low risk of bias
Unclear
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a if a nursing home patient dies from an untreated bedsore.
Also Check: What Do You Do If You Have An Ulcer
Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Also Check: How To Detect A Bleeding Ulcer
Read Also: Ulcerative Colitis And Alcohol Mayo Clinic
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
-
the Cochrane Wounds Specialised Register
-
the Cochrane Central Register of Controlled Trials
Searching other resources
Potential Biases In The Review Process
This was a sparse network and there may have been smallstudy effects which impacted on the network . The STATA routines have largely been developed for and tested on larger networks, and our work has contributed to modifications for sparse networks in the netweight routine. Other STATA routines can be modified by the user to take into account smallstudy effects, but we did not explore these approaches because there was too much uncertainty in the network for us to be confident of interpreting the results. Instead, we used the standard routines for NMA and adapted the recent approach to GRADE to bring in sparseness when assessing evidence certainty.
A further effect of the sparseness of the network may have been to hide any inconsistencies. The various statistical tests for inconsistency were generally not significant, but this may have been due to a lack of sensitivity of the tests and the wide CIs around the measures. Despite this, we found inconsistencies in the network for contrasts involving phenytoin. We cannot be sure that there are no other inconsistencies, but this may not matter given the already identified large uncertainties.
Read Also: Medicine For Diabetic Foot Ulcer
Protect The Periwound Skinexpand: More
Askina® Barrier Cream acts as a protectant and moisture barrier against maceration caused by incontinence or bodily fluids, to protect sensitive, fragile skin and severely dry skin, including peri-wound areas. It is indicated for use on intact skin.
Askina® Barrier Film Swab and Askina® Barrier Film Spray are sterile liquid dressings intended to form a uniform, transparent film when applied to the skin. The film can provide oxygen and moisture permeability. Both dressings are indicated for use on intact or damaged skin.
Description
- Manage bacterial load and odor
- Manage exudate and promote moist healing
- Protect the periwound skin
Stage 4 Decubitus Ulcers
This is the most severe type of decubitus ulcer stage and has the deepest wound. Not only is the skin damaged, but joints, muscles and tendons around the skin can also be damaged and are often exposed. This deep open wound is a problem, because it leads to severe infections and diseases that can ravish the immune system of patients. Once the bone becomes infected during this stage, it can lead to death or the need for amputation.
The stages of decubitus ulcers progress quickly and must be managed before they reach stage 4. These sores are often preventable and measures must be taken to ensure that infection, death and amputation do not occur.
You May Like: Signs You Might Have An Ulcer
Read Also: How To Know If You Have An Ulcer
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
What Is A Stage 2 Bedsore
If a stage 1 bedsore is not treated promptly or properly, it may progress into a stage 2 bedsore. At this stage, the bedsore has broken into the top layers of skin, looks like an open blister, and generally causes pain and discoloration.
Nursing home residents may be at risk of bedsores if they have limited mobility or underlying health problems. Untreated stage 2 bedsores can worsen, causing serious health problems or even death. Fortunately, proper medical care can help older adults recover.
You need to know that stage 2 bedsores may be a sign of nursing home abuse or neglect. Staff members are trained to prevent bedsores if they fail to do so, you may be able to hold them accountable through legal action.
Also Check: What Can You Do For A Bleeding Ulcer
Recommended Reading: What Does Ulcerative Colitis Affect
The Icd Code L89 Is Used To Code Pressure Ulcer
Pressure ulcers, also known as pressure sores, bedsores and decubitus ulcers, are localized injuries to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. The most common sites are the skin overlying the sacrum, coccyx, heels or the hips, but other sites such as the elbows, knees, ankles or the back of the cranium can be affected.
| Specialty: |
Quality Of The Evidence
We have explored the application of a new approach to GRADE analysis, alongside NMA in STATA . We applied the GRADE approach separately to effect estimates for different contrasts and to the ranking of interventions, but the two aspects are closely interrelated and, in this review, are a consequence of the sparse network and the high risk of bias through much of the network. The effect estimates were exemplified by contrasts of interventions versus saline gauze.
Across the network as a whole, the evidence was of very low certainty. There was overall high risk of bias and overlap of the ranking probability distributions, and no clearcut results. The evidence was of such poor quality that we consider it inappropriate to focus on which treatments had the highest probabilities of healing .
You May Like: What Not To Eat When You Have Ulcerative Colitis
Stage 1 Decubitus Ulcers
These types of ulcers refer to sores where the skin is still intact, which means that an open wound is not visible. This stage is best identified with a redness color on the skin and pain to the touch. The redness color often only appears when pressure is applied, which is known as blanching. It is important to keep an eye on patients with darker skin coloring, because it is difficult to identify decubitus ulcers in this stage in these types of patients.
Recommended Reading: Arterial Ulcer Vs Venous Ulcer
Preparing To Go Home After Surgery

Your discharge recovery plan will be made before surgery. Your care plan will focus on doing everything possible to promote healing and prevent problems.
- You will need to be taught wound care, or your family will need to be taught if they are going to help manage your care. Normally, not much wound care is needed other than cleaning, keeping the area dry, and managing any wound drains.
- Home health care or a stay in a skilled nursing facility may be set up if needed.
- Follow-ups with your doctor as needed.
- You must have the proper equipment to promote healing and help prevent future skin problems.
- A pressure-reducing mattress . You will lie on this air or fluid bed to reduce pressure on the healing wound.
- A pressure-reducing seat cushion. Pressure mapping should be done for wheelchair users to ensure that the best cushion is used. Pressure mapping uses a thin, sensor mat on the wheelchair seat. A computer screen displays how well your weight is spread across the seat surface. Spreading weight out help reduce pressure points that are more likely to damage the skin.
You May Like: Does Ulcerative Colitis Cause Acne
+ Best Dressing For Stage 2 Pressure Ulcer On Buttocks Png
Read Also
What is the treatment for a pressure ulcer? This video discusses how to assess and provide localized wound care for a pressure injury, and includes a demonstration of how to clean and . Without treatment, they can get worse. Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury. In the early stages of bedsores, the area may heal with relief of pressure and by applying care to the affected skin.
Treatments Your Physician May Prescribe
In addition to self-care, your doctor might prescribe special pads or mattresses. Special dressings may be used, and whirlpool baths or surgery may be recommended to remove dead tissue. Infection requires antibiotic treatment. Sometimes deep wounds may require surgery to restore the tissue. Experimental work is now being done using honey preparations, high-pressure oxygen, and application of chemicals that stimulate cell growth .
Recommended Reading: Can You Drink Ensure With Ulcerative Colitis
You May Like: What Will Help Stomach Ulcer Pain
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
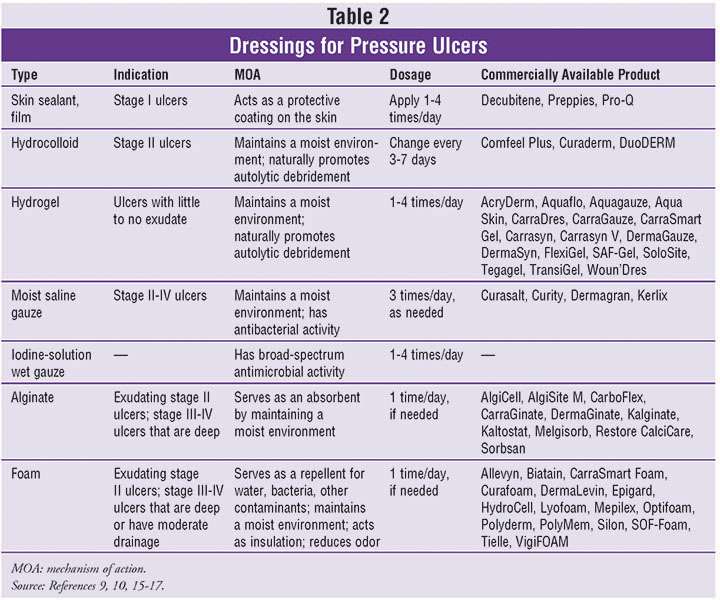
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Appendix 1 Pressure Ulcer Grading
One of the most widely recognised systems for categorising pressure ulcers is that of the National Pressure Ulcer Advisory Panel . Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury, in which wound depth and/or extent, or both, cannot be accurately determined unclassifiable pressure ulcers are generally severe and would be grouped clinically with Stage 3 or Stage 4 ulcers :
The two additional categories of unclassifiable wounds are:
- Unstageable/unclassified Obscured fullthickness skin and tissue loss: Fullthickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
You May Like: How To Cure Gastritis And Ulcers Naturally
Symptoms Of Pressure Sores
Pressure sores go through 4 stages.
- Stage 1. During this stage, the area of the sore looks red. It may feel warm to the touch. It may burn, hurt, or itch. The pressure sore may look blue or purple in people who have dark skin.
- Stage 2. During this stage, the area is more damaged. The sore may be open. It may look like a cut or blister. The skin around the sore may be discolored. The sore is painful.
- Stage 3. During this stage, the sore will have a crater-like look. This is due to increased damage below the surface. This makes the wound deeper.
- Stage 4. This is the most serious stage. Skin and tissue are severely damaged. The sore becomes a large wound. Infection is possible. Youre likely able to see muscle, bones, tendons, and joints.
Infected pressure sores take a long time to heal. Also, the infection can spread to the rest of your body. Signs of infection at the site include:
- Thick, yellow, or green pus
- A bad smell coming from the sore
- Redness or skin that is warm to the touch
- Swelling around the sore
Signs that the infection has spread include:
What Are The Risks Of This Treatment
Problems can happen during any surgery, even with the best treatment. Your surgeon will talk with you to explain what problems might happen. It is up to you to decide whether the benefits of the surgery outweigh the possible risk for problems. Here are a few examples of the more potential serious problems you will talk about with your doctor:
- The wound comes back
- The wound either does not close properly or breaks open along the row of stitches holding the flap edges together
- Harmful bacteria get into the body through an opening in the skin and leads to an infection
- The skin and tissue used for the flap dies
- Bleeding occurs under the flap that may need emergency treatment to drain
Read Also: How Do You Treat Diabetic Ulcers