Questions To Ask Your Health Care Provider
- How often do I need to see a gastroenterologist?
- How often do I need to undergo testing?
- What are my risks for colon cancer?
- Are there symptoms that should cause worry? If so, what are they?
If you dont know something at any point, ask for more information! For some, hearing that they have ulcerative colitis is a relief, a reason for symptoms and a light at the end of the tunnel. For others, it can be scary and daunting. Many will have a mix of feelings.All of this is completely normal.
What Are The Long
The long-term outlook for ASUC is guarded. There is a 20% chance that you’ll need colectomy surgery after your first hospitalization, but that chance rises to 40% after two hospital admissions for ASUC. Severe flares are linked to a 1% risk of death.
Older age is linked with higher death rates. The death rate from ASUC is over 10% in people over 80 compared to fewer than 2% for people between the ages of 50 and 59.
UC is a chronic disease with no cure. Developing acute, severe symptoms is a risk for up to 20% of those diagnosed with the disease. With hospitalization, medical management, and a knowledgeable health care team, you can recover from a bout of ASUC and go into remission, but new flares are possible.
Show Sources
What Is Ulcerative Colitis
Dont Miss: Is Ulcerative Colitis Genetically Inherited
Read Also: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
How Can You Help Your Doctor Determine Ibd Severity
Your doctor will want to know what IBD symptoms you have experienced over the past several days or weeks. You can prepare by keeping a written record of these before your next doctors visit.
Your doctor may ask you about:
- The number of your daily bowel movements
- Any change in the number of daily bowel movements
- The number of loose stools or diarrhea per day
- Whether you have needed to use antidiarrheal medication
- Whether you have blood in your stool, including how much and how often
- How often you have abdominal pain and how severe it is
- Any changes in your body weight
- Any complications, including fevers, joint pain, skin rashes, and eye problems
- Whether symptoms have limited your ability to eat or drink
- Whether symptoms have limited your ability to perform activities of daily living
- Your overall sense of well-being and whether symptoms are improving or worsening
Your doctor may want to evaluate your symptoms using a standard questionnaire. Two common indexes for assessing IBD symptoms include the Crohns Disease Activity Index and the Mayo Score for Ulcerative Colitis Activity.
For children, slightly different scales are used, including the Pediatric Crohns Disease Activity Index and the Pediatric Ulcerative Colitis Activity Index. While there are small differences between these and other methods to assess IBD, they all focus mostly on changes in bowel habits, the presence of complications, and overall quality of life.
Newly Diagnosed With Ulcerative Colitis
No matter what you may be feeling upon hearing you have ulcerative colitis, it is of great value to know that you are not alone. Many places have support groups, both in-person and online, for people all ages that can be very helpful.Talk to your health care provider about support groups at their office or the hospital or do your own research to get involved with the ulcerative colitis community.
If you are overwhelmed by your new diagnosis, dont wait toreach out to a mental health expertto talk through the changes. Relaxation techniques, such as yoga, meditation or mindfulness, may be very helpful.
Working together with your health care team, you can make a treatment plan just for you, to help control your symptoms andput you in charge of your ulcerative colitis.
Recommended Reading: Medicines Used To Treat Ulcerative Colitis
When To Contact A Medical Professional
Contact your provider if:
- You develop ongoing abdominal pain, new or increased bleeding, fever that does not go away, or other symptoms of ulcerative colitis
- You have ulcerative colitis and your symptoms worsen or do not improve with treatment
- You develop new symptoms
Recommended Reading: Stomach Ulcer Treatment Over The Counter
Why Does Severity Matter
Assessing the severity of IBD at the time of diagnosis is essential to determine which therapies are most likely to achieve remission of symptoms and healing of affected bowel tissue.
Different treatments are more effective for different levels of CD and UC disease activity. Your doctor needs to know what treatments will work best for you and your individual situation. For example, treatments like biologics are more likely to be prescribed if your Crohns or colitis is determined to be moderate to severe. Surgical treatments are generally reserved for severe disease.
Read Also: Ulcerative Colitis When To Go To Er
How Can You Use This Information
You dont need to become an expert in the tools your doctor uses to determine the severity of your condition. However, it is helpful to understand how this information is used.
Determining severity helps your doctor know how to best treat your IBD. Following changes in severity over time helps you and your doctor know if treatments are working.
There are two separate goals of treatment: improving your symptoms and healing your bowels. While the two usually go hand in hand, your health care provider may see improvement in your bowels before you experience an improvement of your symptoms, or vice versa. If youre not seeing improvement in symptoms or in your bowels, it may be time to discuss different treatment options.
It is important to discuss your treatment goals with your doctor, so you can work together to meet those goals.
Remember Tell Your Doctor Right Away If You Have An Infection Or Symptoms Of An Infection Including:
- Fever, sweats, or chills
- Warm, red, or painful skin or sores on your body
- Diarrhea or stomach pain
- Urinating more often than normal
- Feeling very tired
HUMIRA is given by injection under the skin.
This is the most important information to know about HUMIRA. For more information, talk to your health care provider.
Uses
HUMIRA is a prescription medicine used:
- To reduce the signs and symptoms of:
- Moderate to severe rheumatoid arthritis in adults. HUMIRA can be used alone, with methotrexate, or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Moderate to severe polyarticular juvenile idiopathic arthritis in children 2 years of age and older. HUMIRA can be used alone or with methotrexate.
- Psoriatic arthritis in adults. HUMIRA can be used alone or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Ankylosing spondylitis in adults.
- Moderate to severe hidradenitis suppurativa in people 12 years and older.
US-HUM-210186
Reference: 1. HUMIRA Injection . North Chicago, IL: AbbVie Inc.
Also Check: Low Fiber Foods For Ulcerative Colitis
Uc Symptoms Can Get Worse Over Time
Because UC is a chronic disease, symptoms can change or get worse over time. Many people go through periods when they experience few or no symptoms, known as remission, as well as periods of flare-ups when they experience frequent and/or more intense symptoms.
If youre still experiencing symptoms, even while being treated for UC, it could be a sign that your symptoms are not under control.
Experiencing uncontrolled symptoms could mean its time to consider a new treatment.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Read Also: Over The Counter Ulcer Treatment For Horses
Overview Of Biologic Agents
Multiple factors are weighed when considering the use of biologic therapy for patients with UC. Patient-related factors include current and prior therapies disease activity, location, and extent demographics and comorbidities. Treatment-related factors include the therapys efficacy, safety, cost, and convenience. Biologic therapy is indicated for UC patients with:
- Corticosteroid-refractory disease.
- Corticosteroid-dependent disease.
- Disease that is refractory to or intolerant of immunomodulators.
- Disease that is refractory to or intolerant of anti-tumor necrosis factor agents .
Patients with clinical predictors of a poor outcome at diagnosis might also benefit from biologics. Biologic therapy for patients with UC includes the anti-TNF agents infliximab, adalimumab, and golimumab and the integrin inhibitor vedolizumab .
Biologic agents approved for Crohns disease or ulcerative colitis.
What Is The Most Important Information I Should Know About Humira
You should discuss the potential benefits and risks of HUMIRA with your doctor. HUMIRA is a TNF blocker medicine that can lower the ability of your immune system to fight infections. You should not start taking HUMIRA if you have any kind of infection unless your doctor says it is okay.
- Serious infections have happened in people taking HUMIRA. These serious infections include tuberculosis and infections caused by viruses, fungi, or bacteria that have spread throughout the body. Some people have died from these infections. Your doctor should test you for TB before starting HUMIRA, and check you closely for signs and symptoms of TB during treatment with HUMIRA, even if your TB test was negative. If your doctor feels you are at risk, you may be treated with medicine for TB.
- Cancer. For children and adults taking TNF blockers, including HUMIRA, the chance of getting lymphoma or other cancers may increase. There have been cases of unusual cancers in children, teenagers, and young adults using TNF blockers. Some people have developed a rare type of cancer called hepatosplenic T-cell lymphoma. This type of cancer often results in death. If using TNF blockers including HUMIRA, your chance of getting two types of skin cancer may increase. These types are generally not life-threatening if treated tell your doctor if you have a bump or open sore that doesnt heal.
Recommended Reading: Ulcerative Colitis And Apple Cider Vinegar
Ulcerative Colitis Vs Crohns Disease Vs Irritable Bowel
Other gut diseases can have some of the same symptoms.
- Ulcerative colitis affects only your large intestine and its lining.
- Crohnâs disease causes inflammation, but it affects other places in your digestive tract.
- Irritable bowel syndrome has some of the same symptoms as UC, but it doesnât cause inflammation or ulcers. Instead, itâs a problem with the muscles in your intestines.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Also Check: How Do You Cure Mouth Ulcers
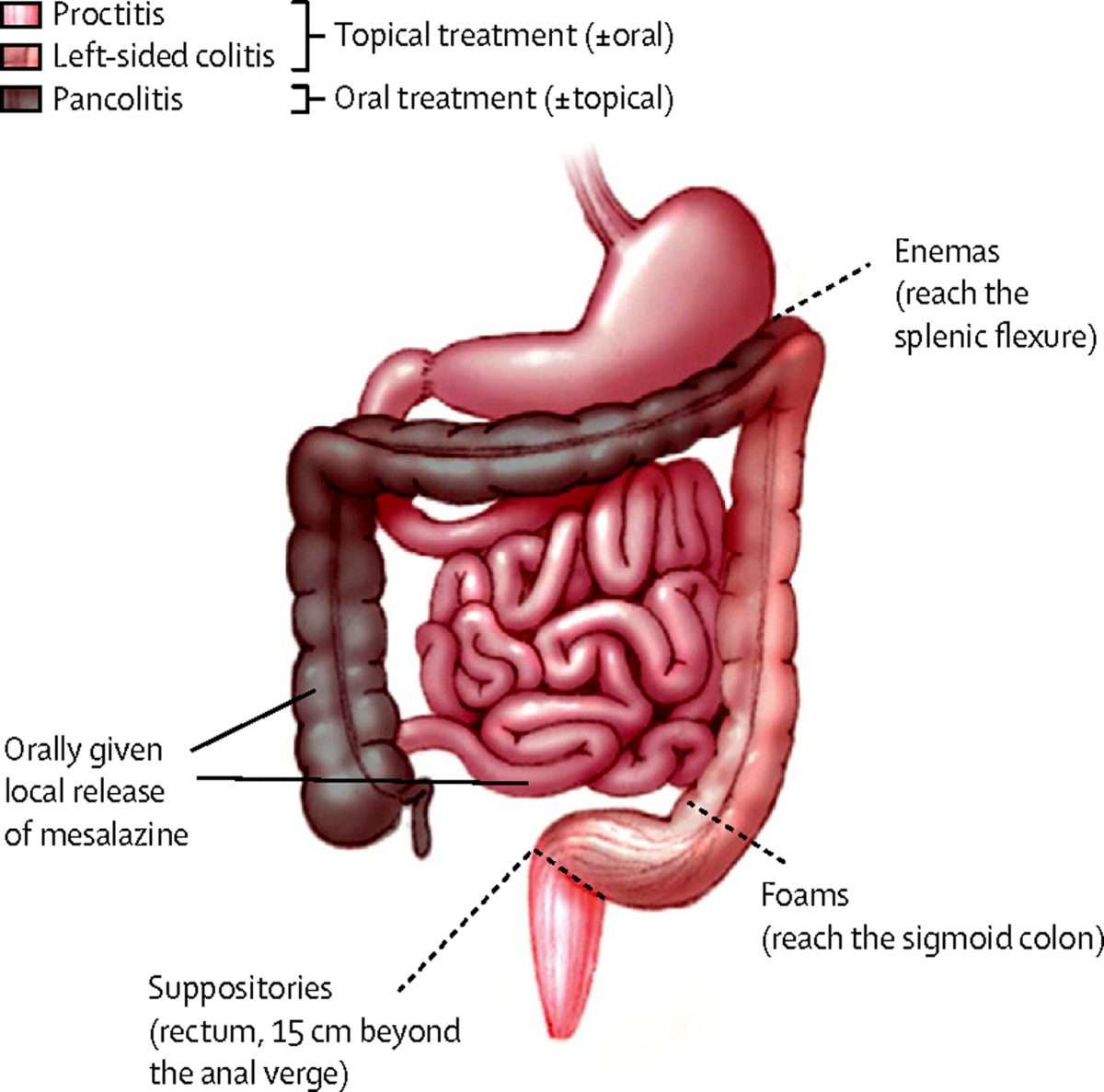
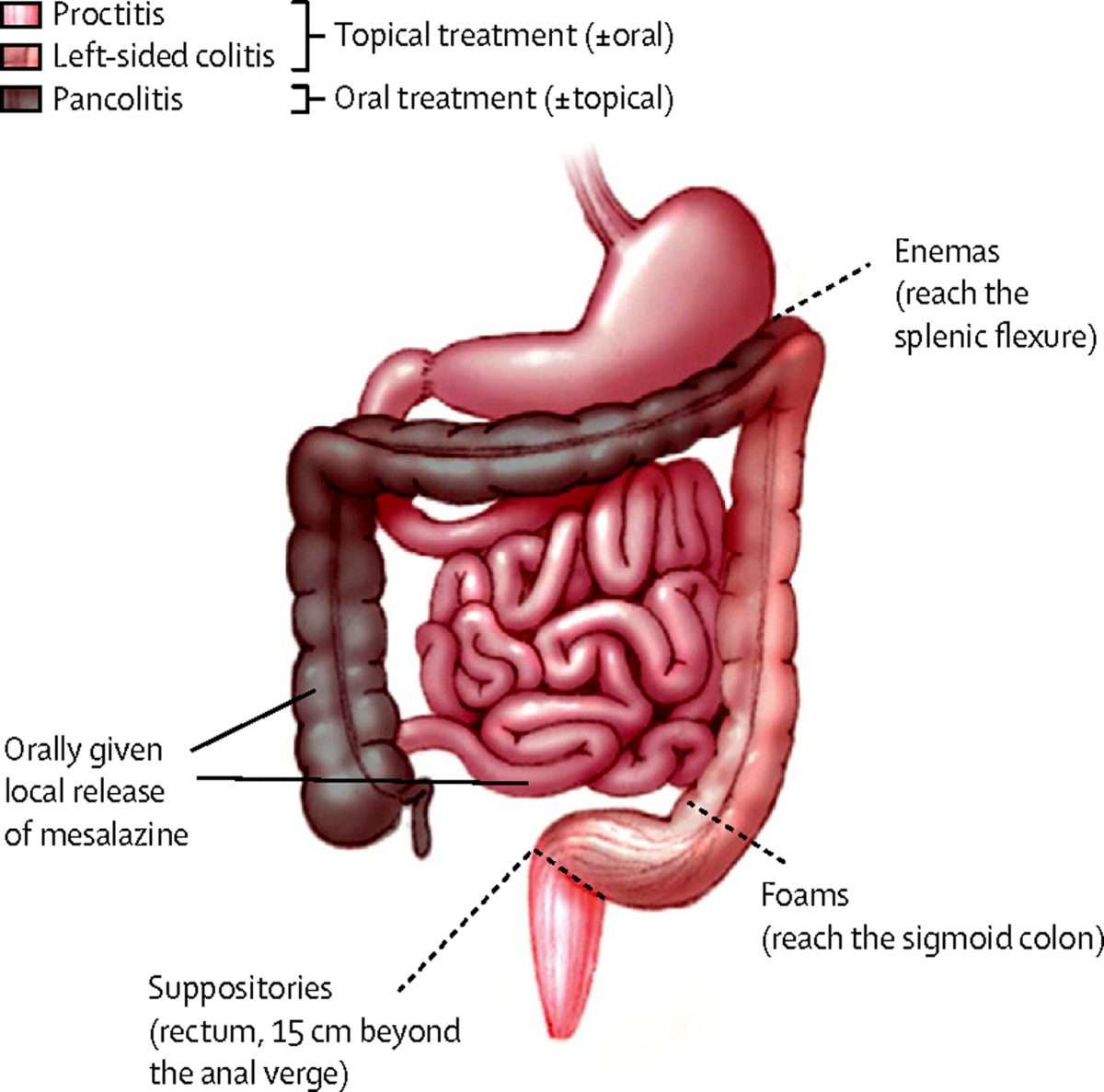
Emerging Treatment Options In Mild To Moderate Ulcerative Colitis: Discussion
Stephen B. Hanauer, MD Dr Lichtenstein discussed the efficacy of the many different oral and topical therapies available for patients with mild to moderate UC. There is no single best approach for all patients. Although rectal therapies may be the most effective approach for patients with distal disease, they may or may not be the most desirable for every patient. Interestingly, most of the oral mesalamine drugs and oral budesonide MMX have demonstrated similar efficacy in both extensive and distal disease. Advantages of some of the new topical therapies include very good tolerance and a low adverse event profile. However, patients are not going to improve unless we select a regimen that they will adhere to.
There are other scenarios in which the budesonide foam formulation has the potential to be effective. It may be beneficial in the postoperative UC patient population. Oral budesonide is effective in the treatment of antibiotic-refractory pouchitis.2 For patients who have undergone colectomy with a stapled ileoanal anastomosis and have cuffitis , we often use mesalamine or corticosteroid suppositories. I suspect that budesonide foam would be effective for these patients. There may also be a role for budesonide foam in the treatment of Crohns proctitis, given that oral budesonide is effective against proximal CD.3
Inflammatory Indexes And Severity Of Uc
Of the 144 active UC patients, 55 and 89 were diagnosed with severe UC and mild-moderate UC, respectively. The mean NLR, PLR, SII, PAR, CAR, and CLR , but not NPR , were significantly higher in the severe group than in the mild-moderate group . NLR, PLR, SII, PAR, CAR, and CLR were significantly correlated with the severity of UC . CLR had the largest AUC , followed by CAR, PLR, SII, NLR, PAR, and NPR . The optimal cut-off value of CLR for severe UC was 7 mg/109 with a sensitivity and specificity of 65% and 73.91%, respectively . The AUC of CLR was significantly different from that of SII, NPR, and PAR , but not NLR, PLR, or CAR .
Table 4. Comparison of inflammatory indexes between severe and mild-moderate UC groups.
Figure 3. Comparison of the predictive performance of inflammatory indexes for severe UC. UC, Ulcerative colitis AUC, Area under the curve CI, Confidence interval NLR, Neutrophil-to-lymphocyte ratio PLR, Platelet-to-lymphocyte ratio SII, Systemic immune-inflammation index NPR, Neutrophil-to-platelet ratio PAR, Platelet-to-albumin ratio CAR, C-reactive protein-to-albumin ratio CLR, C-reactive protein-to-lymphocyte ratio.
Read Also: What Is A Good Diet For Ulcers
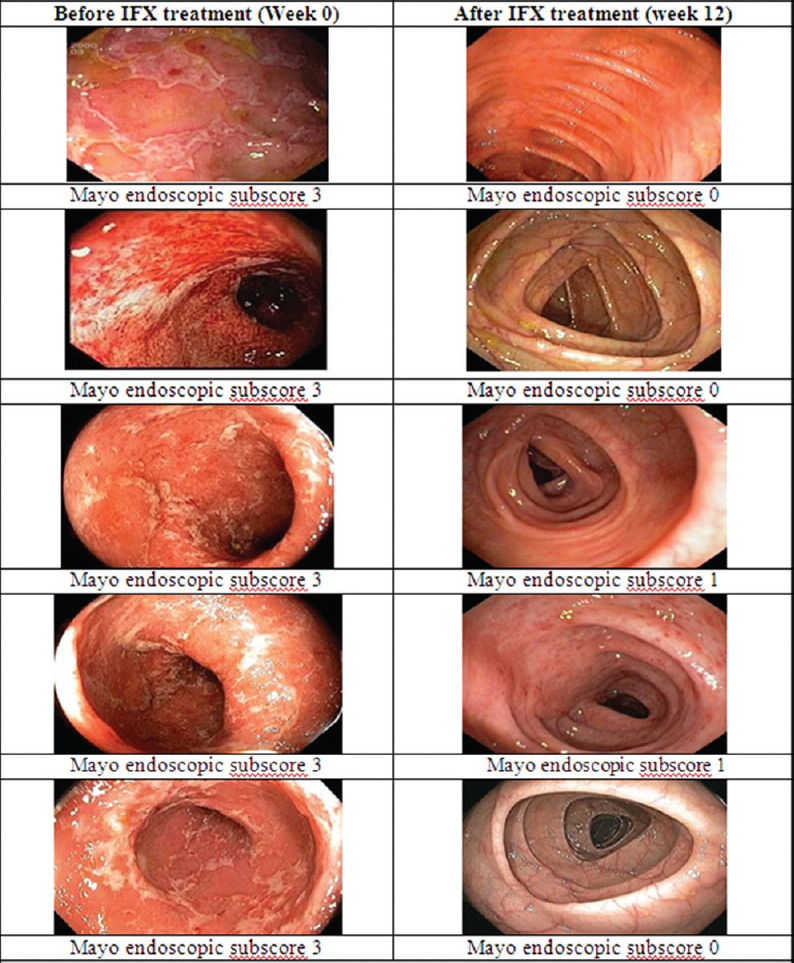
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
A Chronic Inflammatory Disease
Ulcerative colitis belongs to a larger group of illnesses called inflammatory bowel diseases that affect the large intestine in the gastrointestinal tract. It is a chronicor long-lastingdisease that can get worse over time if left untreated.
While the exact cause of UC is not fully understood, research shows that it could be the result of several factors, such as genetics, the environment, or an immune system malfunction.
Also Check: Natural Home Remedies For Ulcers In Stomach In Tamil
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Mild Moderate Or Severe: How Crohns Or Colitis Severity Is Assessed
- The information you share with your doctor, along with endoscopy, laboratory tests, and a physical exam, is used to assess the severity of Crohns disease and ulcerative colitis .
- Your level of disease severity helps determine the best treatment plan for you.
- Changes in severity are used to assess your response to treatment.
Crohns disease and ulcerative colitis are types of inflammatory bowel disease , a chronic and progressive autoimmune disease that affects the gastrointestinal tract. Determining disease severity in Crohns disease or ulcerative colitis is important for identifying the most effective treatment for you and measuring how well it is working.
Also Check: What Causes Ulcers In The Colon
Diagnosing Colitis And Chronic Ulcerative Colitis
Your gastroenterologist may suspect colitis based on your medical history and a review of your symptoms. He or she will have you undergo a colonoscopy procedure using a colonoscope to view the colon and rectum, and may take a tissue sample to help determine the cause. Other tests and procedures include:
- BLOOD TESTSBlood tests are taken to determine both red and white blood cell counts. A low red blood cell count can indicate anemia, from bleeding within the colon and rectum. Elevated white blood cells, which fight infection, indicate inflammation within the colon and rectum.
- STOOL SAMPLEA stool sample may be taken to rule out a parasitic infection that can cause colitis.
- CT SCANIn addition to a colonoscopy, a CT scan can determine what areas of the rectum and colon are inflamed.
Classification of chronic ulcerative colitis
Gastroenterologists categorize chronic ulcerative colitis based on the location and extent of inflammation within the colon and rectum. For most patients, the affected area remains the same during the course of the disease.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Recommended Reading: What Is Good For Ulcers