Assessment Of Other Variables
Using a self-administered demographic and medical questionnaire, subjects were able to report required information including age, sex , marital status , education , smoking status , family size, homeownership , and medical history including existence of hyperlipidemia, hypertension, gallstone, Crohn’s disease, and diabetes. Data on dietary habits including meal regularity , fluid consumption during meals , chewing efficiency , fried foods intake , and fatty meals intake were collected through a pretested dietary habit questionnaire. To examine physical activity of study participants, General Practice Physical Activity Questionnaire was applied. Based on the guideline of this questionnaire, we classified study subjects as having no activity, having activity as < 3 h per week, 35 h per week, 57 h per week, and 7 h per week. Required information about anthropometric variables was collected through the use of a self-administered questionnaire. Body mass index was calculated as weight divided by height squared. Our previous study had shown that self-administered questionnaire of anthropometric measures provides valid information compared with actual measured values .
Ulcerative Colitis Diets You Might Try
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
It Can Be Challenging To Differentiate Between Crohn’s And Ulcerative Colitis
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
|
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
Recommended Reading: What Does Ulcerative Colitis Look Like On A Colonoscopy
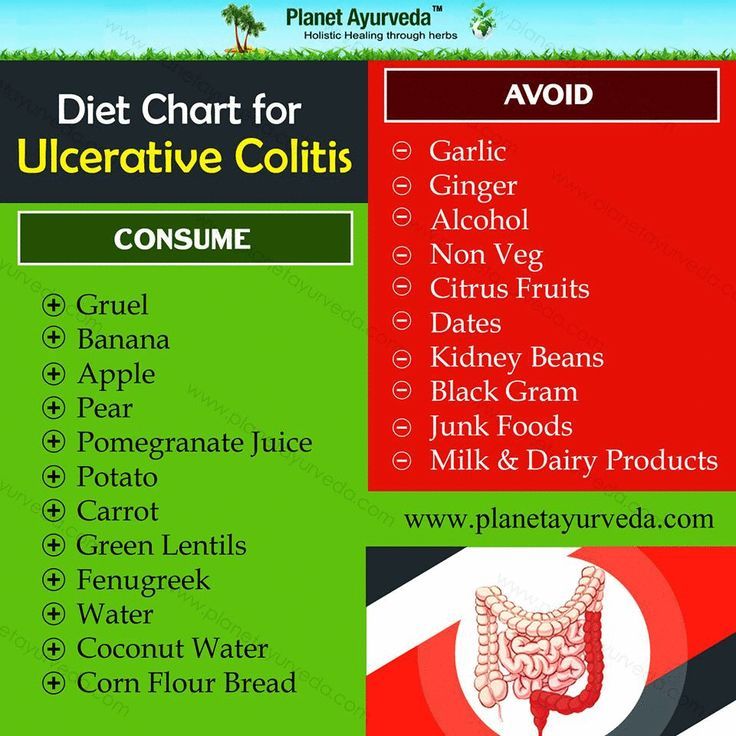
Diet For Ulcerative Colitis
Ulcerative colitis is, literally, a pain in the rear: An inflammation of the large intestine and rectum. The symptoms abdominal pain, cramping, diarrhea and bleeding can be debilitating.
And if you have ulcerative colitis, you know that sometimes it flares up, and it often depends on what youve had to eat. Its important to understand that certain foods do not cause ulcerative colitis and the Crohns and Colitis Foundation of America says diet is not a major factor in causing inflammation. However, some colitis sufferers experience issues related to what theyre eating, so its smart to have an Ulcerative Colitis Diet Plan to help control those flare-ups.
Many people do identify some food triggers and these should be avoided if possible, says Crozer Health gastroenterologist Joyann Kroser, M.D. I think patients who keep a food-and-symptoms diary have more insight into what foods may challenge them. Here is a diet plan that works for most ulcerative colitis patients:
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
Recommended Reading: Icd 10 Code Sacral Decubitus Ulcer
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
Diet Types To Consider For Ulcerative Colitis
What diet type is best for those who suffer from Ulcerative Colitis? This is a question many have pondered on and struggled with throughout the history of irritable bowel diseases. There is no single diet proven to aid in decreasing UC symptoms. We definitely know its NOT a diet filled with inflammatory foods, but a diet filled with easily digestible nutritious food for your gut. There are a plethora of recommended diet types for those who suffer from UC. Theres the Mediterranean diet, the Low-FODMAP diet, the gluten-free and dairy-free diet. The only way to know what works best for you is to try an elimination diet or stick with a diet that prevents flare-ups and doesnt upset your gut. How do you know what foods dont upset your gut, you ask. Simply put, going through a period following one diet, meal planning, tracking your symptoms, and food intake with a food diary or food journal tracker will help you pinpoint what foods make you feel good , and what foods make you feel bad.
You mightve read food diary, and immediately gotten anxious at the complexity of tracking your food and figuring out what your body can tolerate. Dont be worried, or scared! Logging your food with a food diary isnt as complex as it sounds.
These tips should not be used for anything other than educational purposes. To develop a safe, personalized meal plan, you MUST work with your doctor or a dietitian.
Don’t Miss: Foods You Can Eat With Ulcerative Colitis
An Ulcerative Colitis Diet: Summarizing The Evidence
Despite many reports online that certain diets or supplements can cure ulcerative colitis, the only known cure is total removal of the colon and rectum.
Those with digestive symptoms during remission may find relief from a low FODMAP diet to identify trigger foods.
A semi-vegetarian diet has also shown promise in maintaining remission in Crohns disease and may be helpful for ulcerative colitis, but we cannot make firm conclusions.
Even without following elimination diets, certain patterns have been shown to reduce symptoms:
- A diet that is rich in fruits and vegetables provides fiber and antioxidants, which are linked to lower disease risk. Reducing intake of high-fiber fruits and vegetables may increase comfort during flares.
- Limiting dietary fat, especially fatty meats, may be beneficial.
- Certain probiotics are helpful in bringing about and maintaining remission. Ask your doctor for a recommendation.
- A few herbal supplements show promise but lack sufficient scientific evidence to support their use.
- Avoid foods that irritate the gut during flares, including fatty foods, caffeine and alcohol.
A registered dietitian can help you identify foods that trigger your symptoms and design a well-balanced meal plan.
The Best Diet For Ulcerative Colitis
Most experts say that people with UC should simply try to eat a well-balanced diet whenever possible. This should include a variety of foods:
- Lean meat, fish, and poultry
- Low-fat dairy products
- Bread, cereal, and whole grains
- Fruits and vegetables
- Healthy fats such as vegetable oils
Keep a food diary to help you figure out which foods cause problems for you and whether or not youre getting enough nutrients.
If you lose weight because of your ulcerative colitis, try to eat five or six small meals and snacks during the day instead of two or three large meals.
When you have chronic diarrhea, drink plenty of water or other fluids to stay hydrated.
A dietitian can plan a diet that meets your calorie and nutrient needs. Before you take any dietary supplements, talk to your doctor or dietitian. Find out how to make a diet plan for ulcerative colitis.
You May Like: What Foods Help Stomach Ulcers
You May Like: What Is Best Medicine For Ulcer
Think About Vitamin Supplements
Crohns disease often limits the amount of vitamins and minerals your body can absorb from foods. Vitamin B12 is one common deficiency. According to Kennedy, this can be further depleted for those following a semi-vegetarian, vegetarian, or vegan diet, since meat, poultry, and fish are three main sources of this vitamin. If youre transitioning to a plant-based diet, be aware of this deficiency and talk to your doctor about supplementing.
Donât Miss: How To Soothe Mouth Ulcers
Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
Also Check: Natural Treatment Of Ulcer In Hindi
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say

-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
-
You may find a “Low Residue” approach helpful. We have seen it work well for some people
-
Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day
-
Some studies show that a higher fiber diet can improve IBD conditions
Also Check: Peptic Ulcer Treatment At Home
Ulcerative Colitis: This Is Why You’re Here Right
- Why did you get Ulcerative Colitis? The short answer is that scientists still don’t know. Genetics are a major risk factor, but some people without a family history develop the condition
- Ulcerative Colitis is caused by an autoimmune response from your body
- Your symptoms may include:
- GI: loose and urgent bowel movements, bloody stool, abdominal pain and cramps, persistent diarrhea
- Non-GI: appetite loss, weight loss, nausea, low energy, anemia
- There are flares and periods of remission throughout disease course UC is different from other types of colitis because tiny ulcers form, causing long term inflammation
Dietary Habits Of Uc Cases And Controls
No significant difference was observed between cases and controls in terms of dietary habits including regular meal pattern, chewing efficiency, fluid consumption during meals, fried foods intake, and fatty meals intake. This was also the case when we compared the distribution of subjects in terms of above-mentioned variables across quartiles of IPD score .
Table 2. Distribution of patients with ulcerative colitis and controls in terms of dietary habits across quartiles of inflammatory potential of the diet score.
Recommended Reading: What To Eat To Heal An Ulcer
What About A Low Fodmap Or Other Diets
FODMAP stands for fermentable oligosaccharides, di-saccharides, mono-saccharides, and polyols. They are the carbohydrates found in foods and they draw water into the colon, which can make you feel bloated and uncomfortable. FODMAPs also dont pass through your gut quickly but can ferment and hang around for a time, which can cause colitis symptoms.
FODMAPs include:
- Any foods with lactose, or dairy ingredients
- Foods with fructose, including natural fruits, honey, or processed high-fructose corn syrup
- Fructans like garlic, onions, or wheat
- Galactans, which are beans, lentils, or soybeans
- Polyols such as fruits with seeds like apples, avocados, cherries, figs, and peaches
There are other types of diets such as a specific carbohydrate diet that cuts starchy potatoes and grains. Some people have found relief on a Mediterranean diet that includes vegetables, whole grains, fruits, fish, and poultry. A gluten-free diet could also lessen your symptoms.
Read Also: Ulcerative Colitis Mouth Sores Pictures
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
You May Like: Can Stomach Ulcers Cause Blood In Stool
What Foods Should I Avoid
Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.
Which Nutrients Are Important In Crohns And Colitis
Vitamins and minerals
Your body needs vitamins and minerals to work and stay healthy. Your Crohns or Colitis may stop you absorbing enough vitamins and minerals from your food. Vitamins and minerals that you may not absorb properly include iron, vitamin B12, vitamin D and calcium.Eating a healthy, balanced diet may help improve the level of vitamins and minerals in your body. If blood tests show you have low levels of vitamins and minerals, your doctor or specialist nurse may recommend you take supplements to restore your vitamin and mineral levels.Speak to your doctor, specialist nurse or dietitian if you think you may have low levels of any of these nutrients.
Iron
Having low levels of iron is common in people with Crohns or Colitis. Possible causes include a lack of iron in the diet, blood loss and problems absorbing iron from food. Lack of iron can lead to anaemia, where there are fewer red blood cells to carry oxygen around the body.Common symptoms of anaemia include:
Calcium
Fibre
Its important to speak to a dietitian before cutting down on fibre so you dont miss out on the health benefits. For example, they may suggest that some people cut down on fibre for a short time during a flare-up, before slowly adding it back in to the diet.Fibre-rich foods include:
You May Like: When To Go To The Hospital For Ulcerative Colitis
Don’t Miss: Can You Drink Ensure With Ulcerative Colitis