What Causes Uc Cramping
Common causes of UC cramping, according to Ha, are flare-ups, lack of sufficient control of the condition , eating foods that are high in saturated fat or sugar, and adverse reactions to medication.
Cramping due to gas and bloating can also be caused by irritable bowel syndrome , a separate condition from ulcerative colitis that can cause symptoms even when your disease is in remission. IBS can be linked to certain gas-causing foods, including dairy if youre lactose intolerant.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
When Should You Call Your Doctor
If youre experiencing certain symptoms, chances are, your current treatment is not working and its time to consider a change in therapy, says Ha. Call your doctor if:
- Cramping is severe
- Youre experiencing a significant amount of abdominal pain that requires medication
- You have a fever that lasts longer than a couple of days
- You experience nausea or vomiting
- You have ongoing diarrhea or blood in your stool
Also Check: Symptoms Of Crohn’s Disease And Ulcerative Colitis
What Causes Back Pain In Ulcerative Colitis
- Fatigue
- Weight loss
A person having backaches may not realize its related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
What Your Physician Isnt Telling You And What They Dont Know

Diagnosing tight hip flexors is tricky.
If youve seen a therapist or physician, chances are they werent able to pinpoint the issue.
Buried so deep within your abdomen, its no wonder identifying it as the root cause of any of your symptoms is difficult to do.
Its why tight hip flexors are left undiagnosed and untreated for far too long, as physicians look for a simpler explanation.
So understand that this its not your fault.
However, knowing this hands you the power to finally do something about it before its too late.
You May Like: What Foods To Avoid With Ulcerative Colitis
He Had Recurring Pain For Nearly A Decade
- Read in app
The pain woke the 52-year-old physician from a dead sleep. It was as if all the muscles in his right leg, from those in the buttock down his thigh to the very bottom of his calf, were on fire. He shifted slightly to see if he could find a more comfortable position. There was a jag of pain, and he almost cried out. He glanced at the clock: 4 a.m. In just three hours he would have to get up. He had a full day of patients to see. Massage didnt help. He couldnt get comfortable lying flat, so finally he moved to the living room, to a recliner. Only then, and only by lying completely still, did he manage to get the pain to abate. He drifted off, but never for long. The searing pain in his leg and buttock slowly eased, and by the time his alarm went off, he could stand and walk though his muscles still ached and he had to baby his right leg, causing a limp.
Between patients, he arranged to see his own doctor. Hed had pain off and on in his buttocks, one side or the other, for more than a year. The pain was in the middle of each cheek and was worse when he was sitting and at the end of the day. Walking to and from his car on the way home was brutal. And then, as mysteriously as it came, it would disappear only to come back a week or two later.
How Uc Affects The Entire Body
Medically reviewed by Matthew J. Hamilton, MD
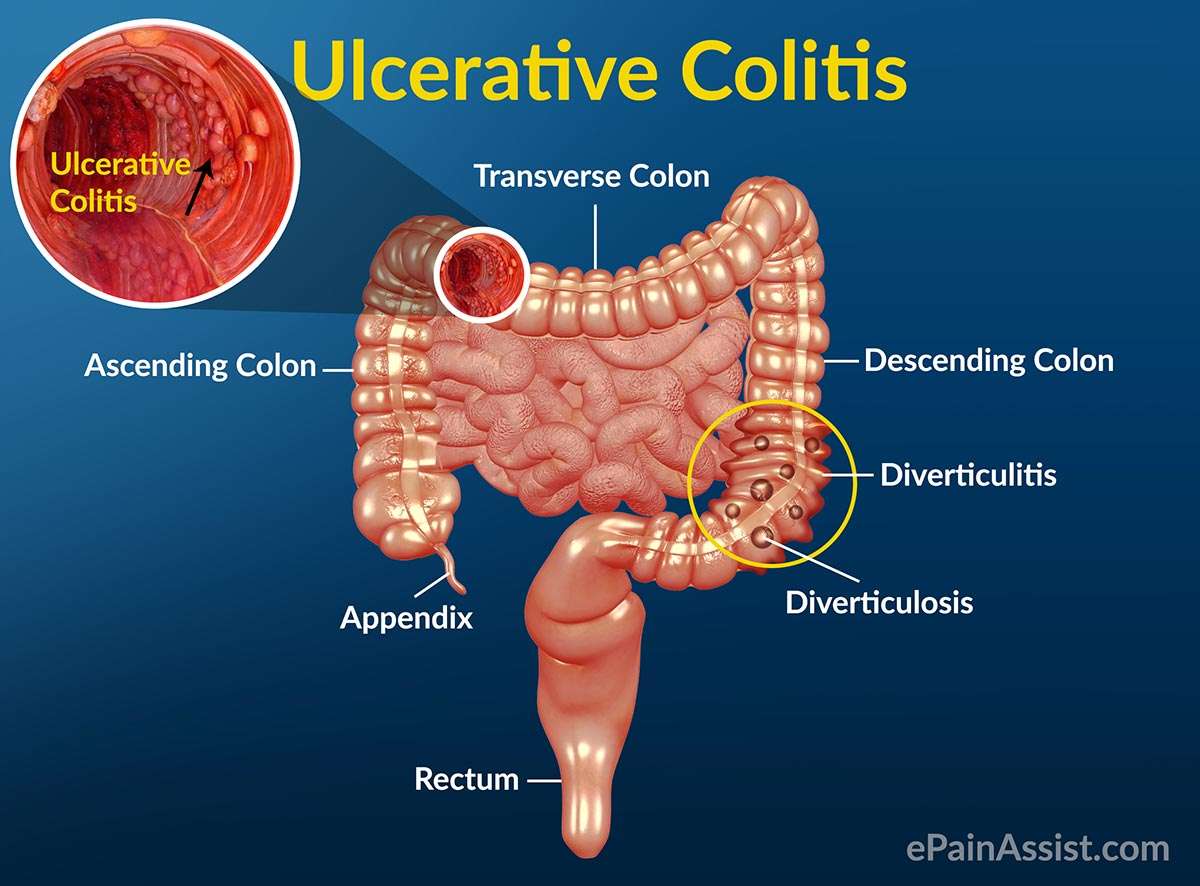
Ulcerative colitis is a type of inflammatory bowel disease, or IBD, that causes chronic inflammation in the large intestine. This can lead to gastrointestinal symptoms ranging from abdominal pain and cramping to frequent bowel movements.
However, inflammation and associated symptoms can go beyond your gutits estimated that up to 40 percent of people with IBD experience one or more non-GI symptoms.
Ulcerative colitis can be more systemic in the way it affects the body, explains David T. Rubin, MD, professor of medicine and chief of gastroenterology at the University of Chicago, and chair-elect of the national scientific advisory committee for the Crohns and Colitis Foundation. Meaning, ulcerative colitis can affect the entire body. Find out what you should watch for, plus ways to take control of your health.
Read Also: How To Treat Pressure Ulcers On Buttocks
How Common Is Cramping Among Those Who Have Uc
Inflammatory bowel disease, which includes both UC and Crohns, affects about 1.6 million Americans of all ages, according to the Crohns and Colitis Foundation. More than half of those with UC experience abdominal pain.
The frequency and persistence of cramping can help determine the severity of UC, according to Faten N. Aberra, MD, MSCE, co-director of the Inflammatory Bowel Disease Center at the Joint Penn-CHOP Center and an associate professor of medicine at the Hospital of the University of Pennsylvania, in Philadelphia. Pain that comes and goes with bowel movements may indicate a moderate level of UC. Constant cramping and frequent, bloody stools, on the other hand, may indicate a more serious condition, says Dr. Aberra, such as a dilated colon.
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with ulcerative colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 138,000 members come together to ask questions, give advice, and share their stories with others who understand life with ulcerative colitis.
Are you living with ulcerative colitis pain? What has helped you to manage it? Share your experience in the comments below, or start a conversation by posting on your Activities page.
You May Like: Surgical Management Of Ulcerative Colitis Ppt
How Does Ibd Affect Other Parts Of The Body
IBD can also cause problems outside the gut. Some people with IBD develop conditions affecting the joints, eyes or skin. These can be known as extraintestinal manifestations and often occur during active disease, but they can develop before any signs of bowel disease or during times of remission. Many of these are not very common.
JOINTS
Inflammation of the joints, often known as arthritis, is a common complication of IBD.
It is most common in those with Crohns Colitis and also affects about one out of 10 people with UC.
The inflammation usually affects the large joints of the arms and legs, including the elbows, wrists, knees and ankles. Fluid collects in the joint space, causing painful swelling, although pain may occur without obvious swelling. Symptoms usually improve with treatment of intestinal symptoms, and there is generally no lasting damage to the joints. A few people develop swelling and pain in the smaller joints of the hands or feet. This may be longer lasting and persist even when the IBD is in remission.
Sometimes, the joints in the spine and pelvis become inflamed a condition called ankylosing spondylitis . This can flare-up independently of IBD. It often causes pain over the sacroiliac joints, on either side of the lower part of the spine. Stiffness and pain in the spine itself may eventually lead to loss of flexibility.
SKIN
MOUTH
EYES
BONES
KIDNEYS
LIVER
Some complications are related to the liver and its function.
BLOOD CIRCULATION
ANEMIA
Switching To A Biosimilar: Effies Experience
At the start of 2020 the government announced that coverage was changing for people who take Remicade® for the treatment of Crohns disease or ulcerative colitis. This meant that patients receiving the biologic drug infliximab, marketed as Remicade®, would see this coverage discontinue with new coverage for the biosimilar version: Inflectra and Renflexis.
Ulcerative colitis advocate Effie was one of those people. In this self-produced video, Effie talks all about her experiences with switching to a biosimilar, takes us through her first Inflectra infusion, and answers some of the same questions you may be asking yourself if you will be going through the same process:
- What is a biosimilar?
Read Also: Can Ulcers In The Colon Be Cancerous
Find Relief From Ulcerative Colitis Constipation
Ulcerative colitis is a form of inflammatory bowel disease that causes the lining of the colon to become inflamed. Ulcers can form in the large intestine and produce pus and mucus.
Symptoms can vary among people but may include bloody stools, abdominal pain, loose or urgent bowel movements, and persistent diarrhea.Constipation may also occur in people living with ulcerative colitis.
Read on to learn about the link between ulcerative colitis and constipation, how to manage it, and when to see a healthcare provider.
Bottom Line On Uc Pain Relief
You may be battling UC pain today but that by no means predicts your future. Complete remission should be a shared goal between you and your doctor. It may take patience to find the best treatment but living your life without UC pain is an achievable goal.
Pain Prevalence:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Over the Counter Medications: Mayo Clinic. Ulcerative Colitis.
How Imodium Works: Imodium. How IMODIUM Products Work.
How Tylenol Works: Tylenol. What Is Acetaminophen?
NSAIDs: Therapeutic Advances in Gastroenterology. Pain Management in Patients With Inflammatory Bowel Disease: Insights for the Clinician.
Prescription Medications:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
You May Like: Vitamin E And Ulcerative Colitis
Univariate Comparison Of Muscle Strength Physical Performance Tests And Habitual Physical Activity Between Uc Patients And Controls
The results for HGS, QS, ST, GS and the HPA evaluation for UC patients and controls are summarized in . QS was significantly decreased in UC patients compared with controls . UC patients were significantly slower than controls at the ST and at the GS test . In addition, HPA levels were significantly decreased in UC patients compared with controls . There was no significant difference in HGS between both groups.
Whats A Good Plan To Manage Uc Cramping
Monitor your medications. Talk to your doctor about any prescription, over-the-counter, or herbal medications youre taking. Iron deficiency is common with UC, but oral iron supplements have been shown to increase the risk of inflammation and cramping. Some antibiotics and pain relievers, such as ibuprofen, may also increase flare-ups and cramping.
Review your diet. Keep a food diary and note the connection between the foods you eat and your UC symptoms. In general, its smart to stay away from processed foods and those high in saturated fat and sugar. High-fiber foods and dairy products can also cause UC cramping, but check with your doctor before eliminating foods from your diet, to ensure youre getting the nutrients you need.
Eat frequent, small meals. Instead of two or three large meals, eat four to six smaller meals spaced more closely throughout the day. Also, take your time while eating and chew thoroughly.
Skip caffeine and carbonated drinks. Caffeine can cause gas, intensifying abdominal cramping. It is also a stimulant, which can make cramping and diarrhea worse.
Drink enough water. People with UC may be at increased risk of dehydration, so be sure to drink plenty of H2O. A good rule of thumb, according to the Crohns and Colitis Foundation, is to aim for about 64 ounces or eight 8 oz glasses per day.
Also Check: Symptoms Of Intestinal Ulcers In Humans
Inflammatory Bowel Diseases And Sarcopenia: The Role Of Inflammation And Gut Microbiota In The Development Of Muscle Failure
- 1Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy
- 2Department of Medicine and Translational Surgery, Fondazione Policlinico Universitario A. Gemelli IRCCS, University Cattolica del Sacro Cuore, Rome, Italy
Sarcopenia represents a major health burden in industrialized country by reducing substantially the quality of life. Indeed, it is characterized by a progressive and generalized loss of muscle mass and function, leading to an increased risk of adverse outcomes and hospitalizations. Several factors are involved in the pathogenesis of sarcopenia, such as aging, inflammation, mitochondrial dysfunction, and insulin resistance. Recently, it has been reported that more than one third of inflammatory bowel disease patients suffered from sarcopenia. Notably, the role of gut microbiota in developing muscle failure in IBD patient is a matter of increasing interest. It has been hypothesized that gut dysbiosis, that typically characterizes IBD, might alter the immune response and host metabolism, promoting a low-grade inflammation status able to up-regulate several molecular pathways related to sarcopenia. Therefore, we aim to describe the basis of IBD-related sarcopenia and provide the rationale for new potential therapeutic targets that may regulate the gut-muscle axis in IBD patients.
Pain Prevalence And Associated Factors
Slightly more than half of the entire group endorsed at least some pain over the previous two weeks before or during their index visit, with 108 people reporting a SIBDQ Pain Score of at least 4 . Considering the emphasis on frequency rather than severity, we correlated the SPS with the pain severity rating of the Colitis Activity Index, which showed a significant relationship between the two measures . Significantly more women than men described their pain as more frequent . Of note, 16 patients used opioids at the time of their index visit. Abdominal discomfort was the main reason for opioid use in 6 of these individuals, with the remaining patients receiving pain medications for joint, back, bone or muscle pains or chronic pancreatitis . In the remaining patients, no reason for opioid therapy could be identified. Opioid use was significantly more common in patients rating their pain as frequently or constantly present compared to those with no abdominal pain .
Abdominal Pain Prevalence in UC Patients with SIBDQ Scores. The histogram shows the distribution of pain scores, which are inversely related to pain frequency. The insert defines the fraction of patients with and without pain.
Don’t Miss: How Do They Diagnose A Stomach Ulcer
Predictors For Impaired Muscle Strength And Poorer Physical Performance
Multivariate binary logistic regression results evaluating predictors for decreased muscle strength and impaired physical performance can be found in . In this analysis, in the total population of UC patients and controls, having the diagnosis of UC was independently associated with a decreased QS and a slower ST. No factor was independently associated with decreased HGS and HPA was found to be protective against an impaired GS.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Read Also: Can You Take Imodium With Ulcerative Colitis
Reducing Your Arthritis Risk When You Have Ulcerative Colitis
Arthritis is the most common complication outside the gut for people with ulcerative colitis. These dos and donts will help you protect your joints.
As if gut pain from ulcerative colitis weren’t enough, as many as 30 percent of people with an inflammatory bowel disease , including ulcerative colitis, will develop problems with their joints, according to the Crohns and Colitis Foundation. Indeed, arthritis is the most common complication that occurs beyond the intestines.
Although it’s not fully understood, there seems to be a link between the gut and joints, says Harry D. Fischer, MD, the chief of rheumatology at Lenox Hill Hospital in New York City. For example, a bacterial infection in the digestive tract can cause a reactive type of arthritis, he notes. In addition, both arthritis and ulcerative colitis have a genetic component.
According to the Crohns and Colitis Foundation, people with ulcerative colitis tend to have one of three forms of arthritis:
- Peripheral arthritis , which affects large joints such as the knees, ankles, elbows, or wrists when IBD is properly treated and controlled, PA joint pain and symptoms typically improve
- Axial arthritis, which causes pain and stiffness in the spine and lower back
- Ankylosing spondylitis, a more severe type of arthritis that affects the spine and can lead to joint damage. Its an uncommon complication that affects between 2 and 3 percent of people with IBD.