What To Do If You Notice A Problem
The signs of diabetic ulcers on the foot should never be left untreated. If you have any of the symptoms mentioned above or think you might have a foot sore or ulcer, you should be seen by a doctor as soon as possible to avoid further damage and possible infection. The earlier you seek medical help, the less chance of complications further down the line.
Here at the Midwest Institute for Non-Surgical Treatment , we have qualified podiatrists who can provide you with the right treatment for your diabetic foot ulcer. We’ll also advise you on how best to look after your feet to prevent reoccurrences.
Book an appointment with Dr. Akinwande and the team who can treat you at one of our convenient locations in the St Louis area. Call us today, and we’ll get you back on your feet and the path to recovery.
About Foot And Leg Wounds And Ulcers
Most of the time, leg ulcers cause pain. If, however, you get leg ulcers due to nerve problems , you may not feel any pain. And because there is no pain, people tend to ignore the ulcer, which can lead to a leg infection.
In addition to non-healing wounds and pain, you may also have these symptoms in your legs:
- Change of color
There are several types of foot and leg wounds and ulcers.
- Venous ulcers are the most common type of foot and leg wounds and ulcers. They usually affect people with varicose veins or deep vein clots. They usually affect the inner part of the leg, above the ankle and may be irregularly shaped, reddish, and covered with yellow fibrous tissue. They also might have discharge.
- Arterial ulcers affect people who have poor circulation, high blood pressure, diabetes, or are smokers. These ulcers usually appear on the outer part of the leg and on the heels, tips of toes, and between the toes where the toes rub against each another. These ulcers vary in color and do not bleed. Often, patients report decreased pain after they dangle their feet over the edge of the bed.
- Neurotrophic ulcers/diabetic ulcers affect people who are diabetic, have nerve problems in their feet, or have had some sort of trauma to their legs or feet. These ulcers usually appear on the heels at the pressure points and may bleed. The surrounding skin is typically calloused.
- Diabetes mellitus
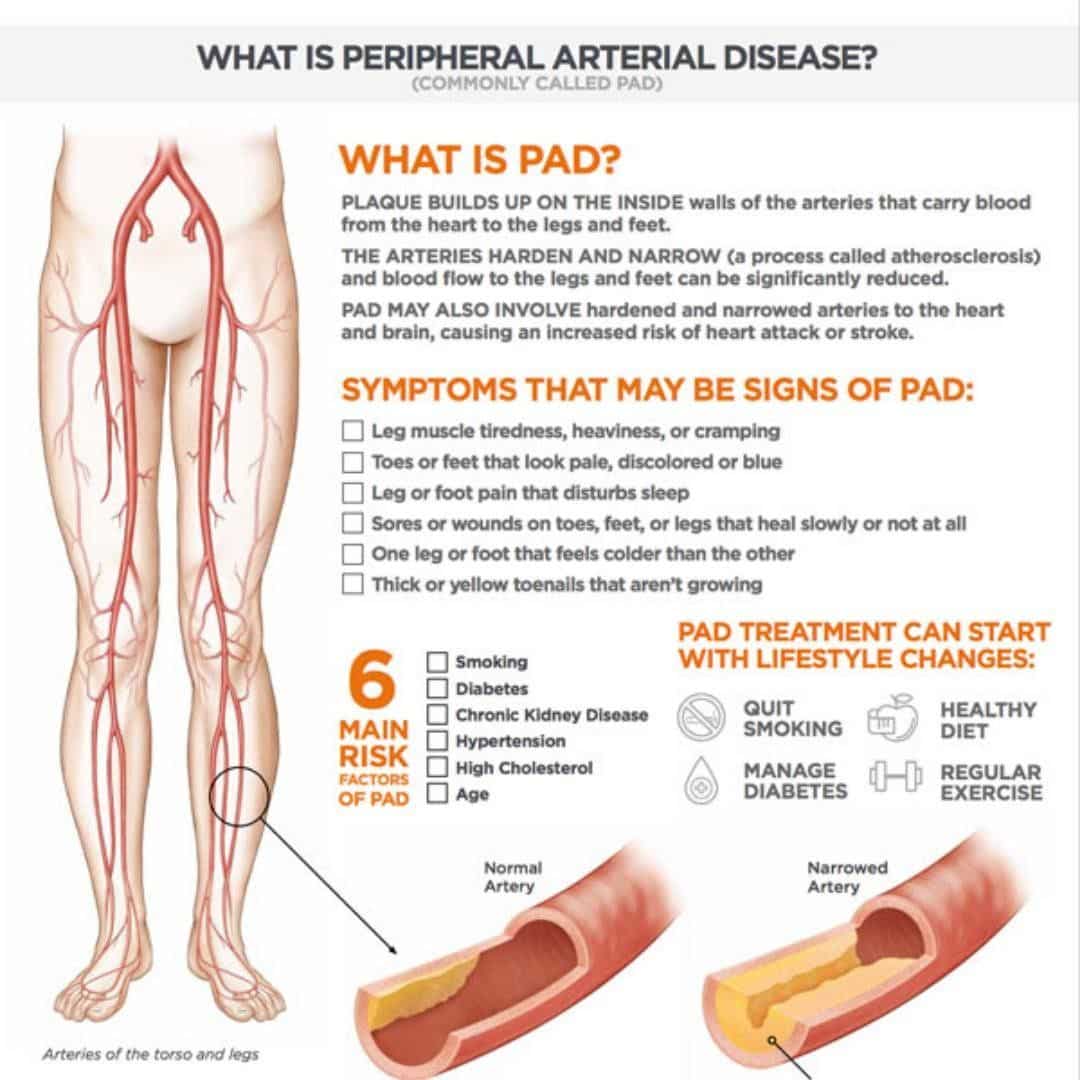
How Does Peripheral Artery Disease Cause Arterial Ulcers
Peripheral artery disease can develop when excess fats and cholesterol circulate in the blood. These substances can begin to build up on the walls of the arteries, forming plaque. This plaque can lead to a narrowing or complete blockage. When the blocked arteries involved are responsible for delivering blood, oxygen, and nutrients to your lower extremities, you may develop PAD symptoms like leg pain, cramping, and fatigue.
Although PAD symptoms affecting mobility are most common, there are other issues to look out for, too. When blood is unable to reach your legs and feet, you may notice problems like regional numbness, coldness, poor hair or nail growth, and skin discoloration. Over time, areas of the skin can become inflamed, break open, and form PAD ulcers.
Recommended Reading: How Does One Get Ulcerative Colitis
Other Tips To Get Rid These Sores
Here is more to tips to prevent or treat the bottom of foot sores:
- Protect your foot from harsh weather i.e. cold or hot weather
- Wash your feet daily
- Wear shoes and shocks almost every time if possible
- You are able to examine every part of your feet daily
- You should also not forget good foot hygiene
- In case you suffer corns and calluses, you should consult the doctor for good care
- You should drink plenty amount of water daily to stay hydrated
- Avoid extreme sweating by removing your tight shoes or socks at some points
- You should avoid hot showers, this robs the skin its moisture
Metatarsal Heads And Sores

According to certain medical study, One of the most common areas for blisters is under the ball of the foot. This includes big or little toe knuckles. Actually, this is where metatarsal heads occur. This is weight-bearing bones that are usually subjected to high pressure.
During the time when the metatarsal skids over the skin and moves backward, the skin is stretched and compressed. Though this is normal to shear here, excessive shear may become unbearable. If this occurs near the surface of the skin, skin blisters may form at the bottom.
The best solutions are to resolve to cushioned insoles, ENGO blister patches, donut pads, etc. For severe conditions please see you GP.
Also Check: Ulcerative Colitis Bad Smelling Gas
Take Pressure Off The Area
If a wound continues to reopen or experience damage, it wont heal quickly and may get much worse. So avoid putting stress, pressure and weight on wounds.
This can be tricky for some wounds like ones on your feet. If you need help, talk to your doctor about ways to protect your wounds while maintaining mobility. Special shoes and customized foot padding are common options.
When Is Surgery Needed
Sometimes, more serious cases of venous insufficiency require surgery. Your doctor may suggest one of the following:
- Surgically repairing veins or valves.
- Removing the damaged vein.
- Minimally invasive endoscopic surgery .
- Laser surgery .
Surgical procedures include:
Also Check: What Are The Signs Of A Bleeding Ulcer
What Should I Do At My Appointment
Remember to remove any nail polish from your toenails before your appointment.
When you see the nurse or doctor, they should:
- Ask about your symptoms and how long you have had problems
- Examine your lower legs
- Do a simple test called a Doppler Ultrasound. This test compares blood flow in your ankle with that in your arm to find out if there are arterial blood flow problems in your lower leg. You may have to come back to have your Doppler test on another day or at another clinic.
- You may also be offered some other tests to check for other health problems that can affect your legs such as diabetes and anaemia.
You may hear different words to describe your wound such as ulcer, leg ulcer, sore, laceration, chronic wound and maybe others. Ask your nurse to explain their choice of word and what this may mean for you.
Getting A Specialist Vascular Referral
If you have venous hypertension / insufficiency, intervention to your veins might help with healing and stop your wound or sore from coming back. Sometimes varicose veins can be treated by laser therapy. But if you have peripheral arterial disease, you may require further investigations and the vascular team will be able to assess the need to improve the blood supply to your leg or whether your ulcer can be managed in other ways such as reduced / modified with compression.
Ask your nurse or GP for a referral to your local vascular team to talk about how their input might help you.
Don’t Miss: Can Ulcers Cause Black Stool
How Are Foot And Toe Ulcers Diagnosed
Your healthcare provider can tell what type of ulcer you have based on four observations:
- The appearance of the ulcer.
- Location of the ulcer.
- The appearance of the borders.
- The appearance of the surrounding skin.
Your primary healthcare provider can diagnose an ulcer, but they might send you to a specialist for treatment. You might see a podiatrist, a provider who works with feet, or a wound specialist. For more complicated cases that require surgery, you might also see a plastic surgeon, anesthesiologist, orthopedic surgeon and/or vascular surgeon.
How Are Ankle Ulcers Diagnosed
Your doctor will begin by asking you about your medical history and symptoms. Make sure to keep a record of all your symptoms since they will help your doctor make a proper diagnosis. If youve had the ulcer for a long time, your doctor may want to take a tissue sample to make sure theres no cancer. MRIs, CT scans, and radiography can also check the depth of your ulcer and if its affected bone. Your doctor will also check your ulcer for infection.
The primary goal of venous stasis ulcer treatment is to heal the wound, treat any infection, and relieve pain.
Don’t Miss: What Does Ulcerative Colitis Look Like On A Colonoscopy
Conditions Such As Peripheral Artery Disease Kidney Failure Diabetes High Cholesterol Or High Blood Pressure
Ulcers are an indication that a severe stage of a condition such as peripheral artery disease, kidney failure, diabetes, high cholesterol, or high blood pressure is present. This is because these conditions impair circulation and damage nerves, increasing the risk for developing ulcers. A primary care physician or PAD specialist can offer strategies on managing these conditions medication, healthy diet, exercise, and proper weight management can often significantly decrease the risk for ulcers.vi
What Do Foot Or Toe Ulcers Look Like
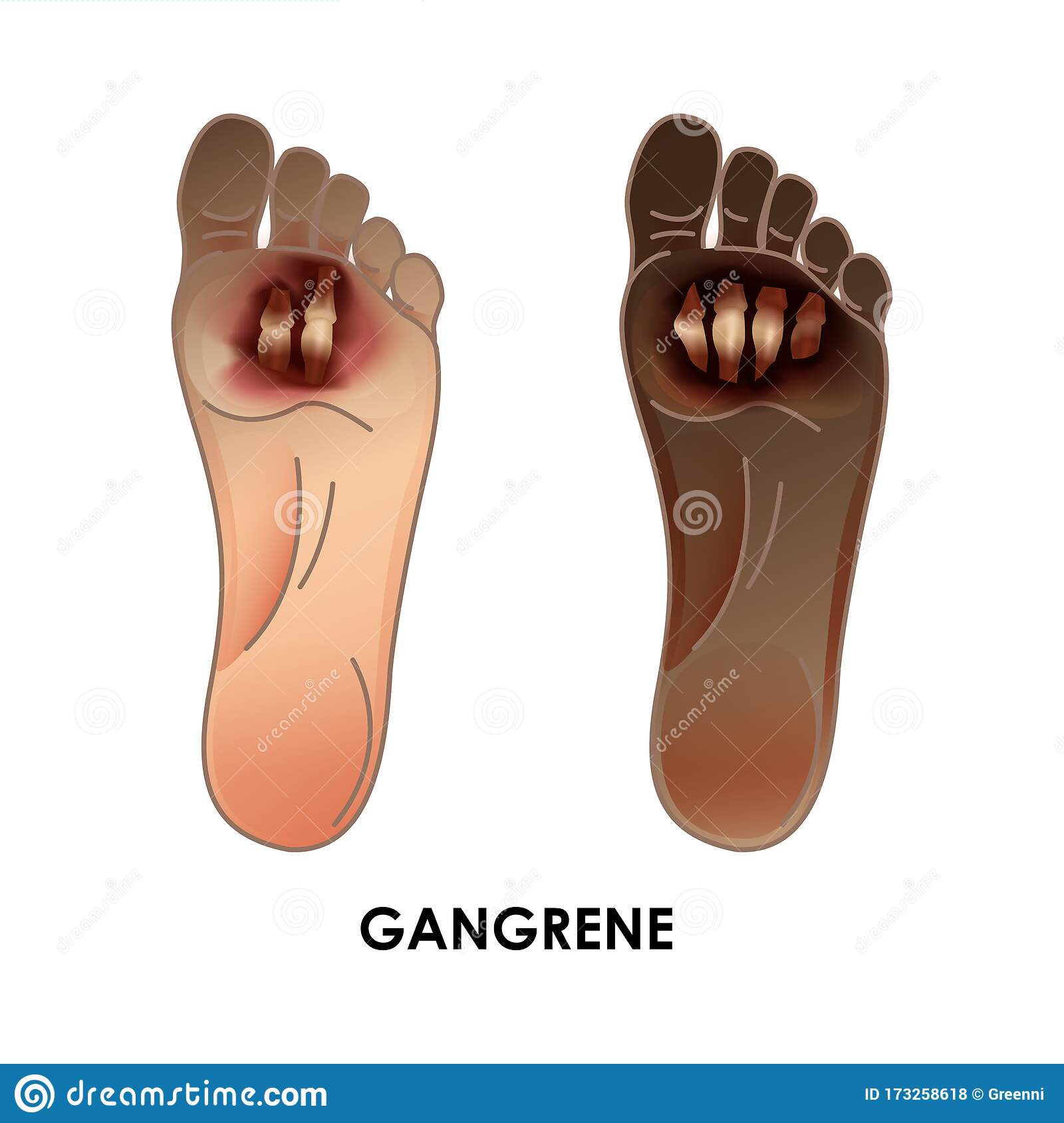
Foot and toe ulcers can take any shape, but theyll commonly look like a wedge or crater. They can range in color and either be yellow, red, pink, or gray. If an ulcer turns black, this means that the tissue has died . Peripheral artery disease can cause gangrene, so if you notice a black ulcer on your foot or toe, seek emergency medical care to prevent further damage.
PAD ulcers can start small but grow larger if it goes untreated. Before the ulcer develops, some patients notice their skin is dry, cracked, scaly, or red. Several classification systems exist to help define the severity of ulcers, and the Wagner Diabetic Foot Ulcer Grade Classification System is one of them. This system has six grades to help diagnose foot ulcers:
- Grade 0: Undamaged, intact skin with no ulcers present
- Grade 1: Ulcer is superficial and may resemble an open sore with broken skin and a skin-deep wound
- Grade 2: The ulcer progresses to more of a deep, crater-like configuration
- Grade 3: The ulcer is deep enough that the bones of your toes or feet are visible
- Grade 4: The front of the foot is gangrenous, meaning a significant portion of the foot is composed of dead tissue
- Grade 5: The whole foot is gangrenous and must be amputated to save the patients life
In addition to the descriptions outlined in these grades, you may notice drainage in your socks or brown discoloration on your foot, often accompanied by a foul odor. PAD ulcers can also resemble a callus or develop a callus on or near them.
Don’t Miss: Herbal Medicine For Stomach Ulcer
Who Gets Foot And Toe Ulcers
Foot and toe ulcers can happen to many people but might be more common in Black, Native American and Hispanic people. If you have an eye, kidney or heart disease related to diabetes, youre also at a higher risk. About 15% of people with diabetes will get an ulcer, typically on the bottom of their foot. Some of those people will be hospitalized because of complications.
Youre also at a higher risk of getting foot and toe ulcers if you have any of the following conditions:
- Blood circulation issues.
If your ulcer is black, that means cells in the tissues have died. This is called necrosis .
How Should A Diabetic Foot Ulcer Be Treated
The primary goal in the treatment of foot ulcers is to obtain healing as soon as possible. The faster the healing of the wound, the less chance for an infection.
There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Prevention of infection
- Taking the pressure off the area, called off-loading
- Removing dead skin and tissue, called debridement
- Applying medication or dressings to the ulcer
- Managing blood glucose and other health problems
Not all ulcers are infected however, if your podiatric physician diagnoses an infection, a treatment program of antibiotics, wound care, and possibly hospitalization will be necessary.
Preventing Infection
There are several important factors to keep an ulcer from becoming infected:
- Keep blood glucose levels under tight control
- Keep the ulcer clean and bandaged
- Cleanse the wound daily, using a wound dressing or bandage
- Do not walk barefoot
Off-Loading
For optimum healing, ulcers, especially those on the bottom of the foot, must be off-loaded. Patients may be asked to wear special footgear, or a brace, specialized castings, or use a wheelchair or crutches. These devices will reduce the pressure and irritation to the ulcer area and help to speed the healing process.
Applying Medication and Dressings
For a wound to heal there must be adequate circulation to the ulcerated area. Your podiatrist may order evaluation test such as noninvasive studies and or consult a vascular surgeon.
Managing Blood Glucose
Don’t Miss: Best Over The Counter Medicine For Ulcer Pain
When To See Your Doctor
If you begin to see blackened flesh around an area of numbness, see your doctor right away to seek treatment for an infected foot ulcer. If untreated, ulcers can cause abscesses and spread to other areas on your feet and legs.
At this point, ulcers can often only be treated by surgery, amputation, or replacement of lost skin by synthetic skin substitutes.
What Are My Treatment Options
Treatment will depend on many factors, including the reason for the condition and your health status and history. Other factors your doctor will consider are:
- Your specific symptoms.
- How severe your condition is.
- How well you can tolerate medications or procedures.
The most common treatment for venous insufficiency is prescription-wear compression stockings, she says. These special elastic stockings apply pressure at the ankle and lower leg. They help improve blood flow and can reduce leg swelling.
You also can improve blood flow by keeping your legs elevated whenever possible, which means keeping them uncrossed when you are seated and by exercising regularly.
If you need medication, the most commonly prescribed include:
- Diuretics. These medications draw extra fluid from your body through your kidneys.
- Anticoagulants. These medications thin the blood.
- Pentoxifylline . This medication helps improve blood flow.
Recommended Reading: What Does Ulcerative Colitis Poop Look Like
Getting Diagnosed With A Foot Ulcer
If you have a wound on your foot that is not healing, make an appointment at your GP practice or with a podiatrist. You may be given an appointment to see the nurse rather than the doctor as they are often responsible for caring for patients with leg and foot problems.
If you know you have diabetes and you have a wound on your foot, then you should seek advice from your healthcare professional urgently .
Make sure you remove any nail polish from your toenails before your appointment.
When you see the nurse, podiatrist or doctor, they should:
- Ask about your symptoms and how long you have had problems
- Examine your lower legs
- Do a special test called a Doppler Ultrasound. This test compares blood flow in your ankle with that in your arm to find out if there are blood flow problems in your lower leg. You may have to come back to have your Doppler test on another day or at another clinic but you should have this test within a few weeks of your first appointment
- Test how much sensation you have in your feet
You might also be offered some more tests to rule out other health problems that can affect your legs, including diabetes, anaemia, thyroid, kidney and cholesterol problems.
If your GP practice thinks you have problems with your arteries, they may refer you for further vascular tests at your local hospital or specialist clinic.
Use Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy is the ultimate proven treatment for diabetic wounds and other non-healing wounds. This safe and natural alternative therapy uses the power of pressurized oxygen to stimulate your bodys innate healing process. As a result, it can kickstart tissue repair in wounds that previously failed to heal.
During an HBOT treatment, you lie comfortably in a special hyperbaric chamber and simply inhale concentrated oxygen. As this oxygen flows through your body, it dissolves directly into all of your bodys fluids and permeates areas where circulation is reduced or blocked. Inhaling the concentrated flow of oxygen provided through regular HBOT treatments makes it possible to overcome oxygen deficiencies and stimulate a more effective healing process.
Also Check: How To Treat Stomach Ulcers Naturally
What Are Foot And Toe Ulcers
An ulcer is an open wound or sore that will not heal or keeps returning. When you have ulcers on your feet and toes, it can be related to diabetes specifically, a complication called neuropathy that causes you to lose feeling in your feet. A scrape, cut or puncture in your skin can turn into an ulcer, but you might not know its there if you have neuropathy.
Ulcers can lead to infections. Sometimes, the infection wont go away and you may need to have part of your foot or toe surgically removed . About 15% of people with diabetes will get a foot or toe ulcer. Around 14% to 24% of people with diabetes in the U.S. need an amputation after they get an ulcer.
How To Prevent Diabetic Foot Ulcers
The first line of defense in preventing diabetic wounds is to follow the guidelines recommended to keep the disease itself under control:
- Maintain healthy blood sugar levels through a healthy diet and by taking medications as instructed by your doctor.
- Keep your blood pressure within a healthy range.
- Avoid alcohol and tobacco.
You should also take measures to avoid causing sores or wounds on the feet:
- Never walk barefoot.
- Wear shoes that fit properly and dont rub the skin.
- Wash your feet daily with mild soap and lukewarm water to prevent the buildup of bacteria on the skin, which can cause infection even in the tiniest skin breaks.
Because a loss of sensation in the feet may mean theres no pain felt even when an ulcer is present, its also extremely important for those with diabetes to regularly check for any foot sores or skin irritation. This way, the ulcer can be properly treated as early as possible.
You May Like: Stage 2 Pressure Ulcer Treatment Cream