How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Clinical Trials Of Budesonide Foam
Two randomized, placebo-controlled trials were conducted to evaluate the efficacy and safety of budesonide foam in inducing remission in patients with mild to moderate UC.2 The studies enrolled 546 patients with mild to moderate ulcerative proctitis and ulcerative proctosigmoiditis extending at least 5 cm, but no more than 40 cm, from the anal verge. Patients were randomly assigned to budesonide foam 2 mg or placebo administered rectally twice daily for 2 weeks, followed by once daily for 4 weeks. Patients were permitted to receive concomitant oral 5-ASAs at a dosage of up to 4.8 g/day.
At week 6, the proportion of patients in remission was significantly higher with budesonide foam vs placebo in both study 1 and study 2 .2 The observation of substantial clinical activity after 6 weeks indicates the rapid onset of activity with budesonide foam. Budesonide foam was also superior to placebo as assessed by the proportion of patients with complete resolution of rectal bleeding in study 1 and study 2 .2 Multiple other endpoints, including endoscopic improvement, mucosal healing, and reduction in stool frequency, were all significantly superior with budesonide foam vs placebo. More than half of patients in the 2 trials were receiving concurrent 5-ASAs, with the budesonide foam added on as an adjunctive therapy. Notably, budesonide foam appeared to have similar efficacy regardless of the use of concomitant 5-ASA.2
Gastroenterology.
Other Foam Preparations
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Don’t Miss: Snack Ideas For Ulcerative Colitis
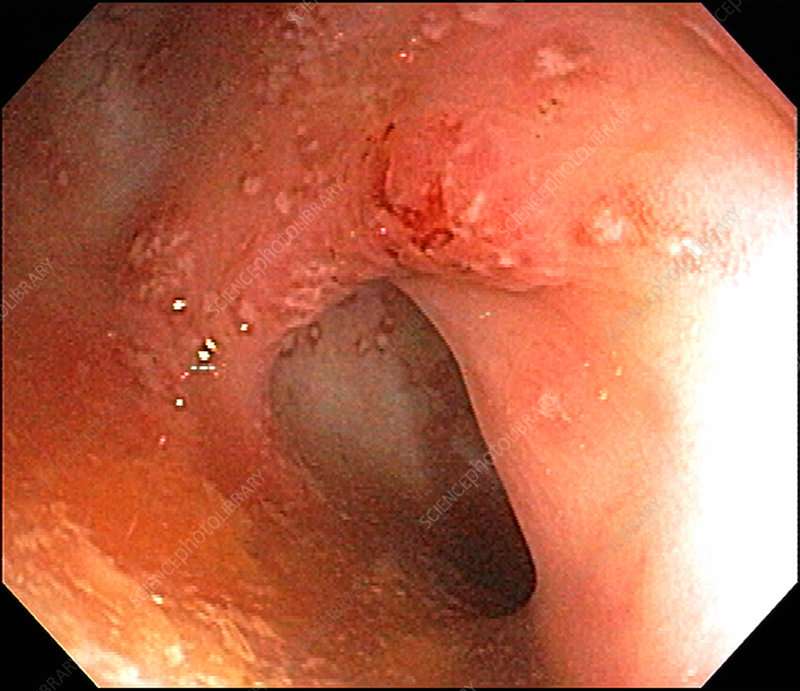
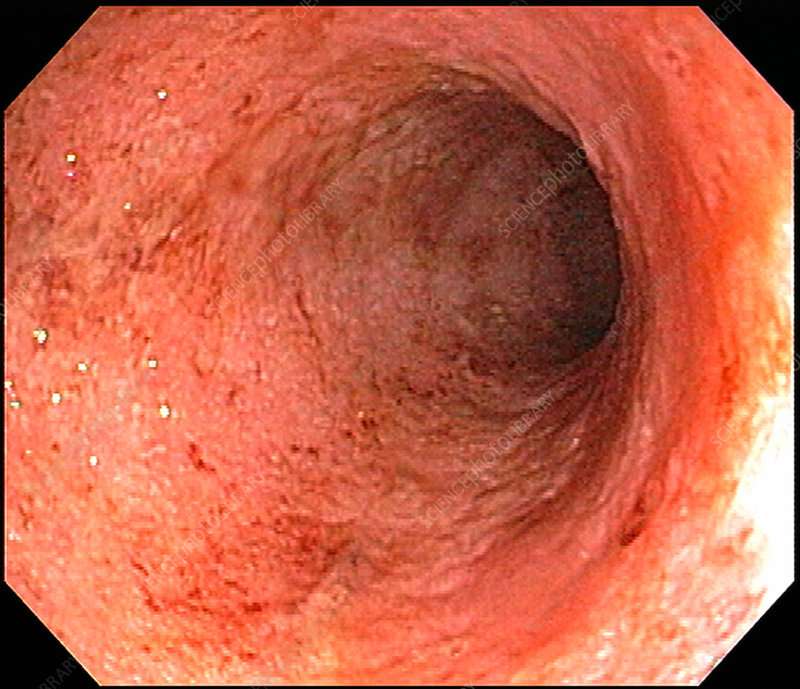
How Does Endoscopy Help Determine Severity
Endoscopy is an extremely important part of determining how severe your IBD is. Using endoscopy, doctors can visually assess the damage to your bowels by identifying and measuring lesions, looking for bleeding, and taking biopsies.
Endoscopy will reveal different findings based on whether you have Crohns disease or ulcerative colitis. Two commonly used indexes to measure endoscopy results are the Simple Endoscopic Score for Crohns Disease and the Ulcerative Colitis Endoscopic Index of Severity.
Some of the important measures for Crohns disease include:
- Whether there are ulcers
- How much bowel surface is involved
- How much bowel surface has ulcers
- Whether there are strictures, or narrowings, of the intestines
- How narrow any strictures are
Some of the important measures for ulcerative colitis include:
- Whether normal intestinal blood vessels are visible or obliterated
- Whether there is blood or visible bleeding
- Whether there are erosions or ulcers
Management Of Moderate To Severe Ulcerative Colitis
- Gastroenterology
Youve saved your first item
You can find your saved items on your dashboard, in the saved tab.
Youve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
Youve subscribed to your first topic alert
What does that mean?
Don’t Miss: Managing Ulcerative Colitis Flare Ups
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
You And Your Care Team Are In Control
While there is no cure for UCwhile also knowing it can progress and symptoms can get worse over timeits important to remember that you and your doctor can get your disease under control. Recognizing the signs early and getting treatment right away is key. Thats why having open conversations with your doctor and being prepared for every appointment is crucial to managing your UC.
Speak openly with your doctor about how much your UC is truly impacting you. Make a personal action plan to see how much of your time your disease is affecting and get customized steps to help you and your doctor get control of your disease.
Also Check: Can Ulcers Cause Chest Pain And Shortness Of Breath
What Are The Different Types Of Ulcerative Colitis
While ulcerative colitis severity describes the level of your symptoms, the type of your condition refers to how far itâs spread and which parts of your body it involves. The types of this condition tie to different levels of severity.
Your doctor will perform a colonoscopy with a biopsy to find out which you have. There are four main types of ulcerative colitis:
Ulcerative proctitis. If you have this form, it means the disease is only in your rectum. Your symptoms will most likely be more mild.
Ulcerative proctosigmoiditis. With this form, your ulcerative colitis affects your rectum and sigmoid colon . But it doesnât involve your descending colon . This type may happen with more severe symptoms.
Left-sided colitis. In this group, it goes beyond your sigmoid colon. It may go as far as your splenic flexure or 60 centimeters past your anal verge . Left-sided colitis is usually more severe than the previous two types.
Extensive colitis or pancolitis. This form extends around your splenic flexure or 60 centimaters past your anal verge. If the condition affects your entire colon, experts call it âpancolitis.â This form has more intense symptoms.
Your doctor may also look at how intense your inflammation is. Theyâll use the endoscopic evaluation for mucosal ulcerations and disease extent to do this. There are a few different scores to review this, but the Mayo endoscopic score of activity is common. This ranges from 0 to 3.
Assessing Severity Of Disease In Patients With Ulcerative Colitis
Ulcerative colitis is a chronic disease that can present at various stages of disease activity and severity. Traditionally, severity scoring has focused on disease activity during a single moment with various tools, including patient-reported symptoms, as well as clinical, laboratory-based, endoscopic, histologic, and imaging variables. Optimal delivery of care depends on the accurate assessment of disease severity, which must take longitudinal variables into account. This article reviews the history of severity scoring in UC and provides a concise, clinically oriented approach to assessing disease severity.
Keywords: Clostridium difficile
Recommended Reading: How To Use Aloe Vera Gel For Ulcerative Colitis
Recommended Reading: What Does An Ulcerative Colitis Flare Up Feel Like
Assessing Ulcerative Colitis Disease Severity
Multiple factors are used to assess disease severity in UC, including the frequency of bowel movements, the extent of rectal bleeding, the endoscopic appearance, and the effects of the condition on a patients quality of life and day-to-day activities. Mild disease, which is typically considered to be fewer than 5 bowel movements per day, does not negatively affect daily life, as patients are able to adapt to the bowel frequency. Moderate to severe disease is characterized by more frequent bowel movementsup to 10 per daywith bleeding. This degree of severity may interfere with patients attendance at work or school.
Clinical trials in UC have classically used the Mayo Score, which is based on the frequency of bowel movements, the number of bowel movements with blood, and an overall assessment of how the symptoms impact daily activities .10 There is not one simple method of evaluating a patients disease severity. One patient may develop proctitis that is severe and disabling, whereas another patient may have extensive colitis that is mild and has a limited effect on daily activities. There can also be disparities between a patients symptoms and the endoscopic appearance. There are patients with mild endoscopic disease who have severe symptoms, and there are patients with more severe colonic inflammation who have no quality-of-life impairments.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
You May Like: Symptoms Of A Bleeding Ulcer In Your Stomach
How Do You Get Diagnosed With Ulcerative Colitis
Common tests used in patients with UC are:
- Colonoscopy: this is the test used most commonly to make the initial diagnosis of UC and later for ongoing monitoring of disease severity.
- Routine blood tests: detect infection, anemia, inflammation and vitamin deficiencies.
- Fecal blood test: detects blood in your stool and bleeding in the intestines.
- Other stool tests: detect infection and monitor disease severity.
- Computerized tomography : shows different images of the bowels and surrounding tissue.
Read Also: Treating Hindgut Ulcers In Horses
Information Sources And Search Strategy
We will systematically search PubMed, Web of Science, MEDLINE, CINAHL, the Cochrane Library, Embase, China National Knowledge Infrastructure , Chinese Biomedical Literature database , and WANFANG database for related randomized controlled trials that compared one TCM intervention with another or with 5-ASA in the treatment of mild-to-moderate UC. The temporal interval is limited from the time that the databases created to February 2019.
The searches were restricted to papers that were published in English or Chinese. The search strategy will be conducted independently by 2 authors who are experienced in the information retrieval and combine free text words and medical subject headings regarding Chinese medicine,traditional Chinese medicine,Chinese herbal,Ulcerative colitis, UC,Inflammatory bowel disease,IBD, and randomized controlled trials. MeSH and subheadings were combined with AND or OR. Furthermore, we will also retrieve the WHO International Clinical Trials Registry Platform and ClinicalTrials.gov to identify ongoing trial registers. We will manually search related systematic reviews/meta-analyses and bibliographies of included studies to identify additional potential studies. The preliminary search strategy for PubMed is summarized in Table Table1,1, which will be adapted according to syntax-related requirements of other electronic databases.
You May Like: What Does A Stomach Ulcer Look Like
How Is Ulcerative Colitis Treated
In most people, mild to moderate ulcerative colitis can be treated at home simply by taking medication. This can relieve symptoms and prevent flare-ups, allowing long-term remission. These medications are aminosalicylates, corticosteroids and immunosuppressants.1
People with severe ulcerative colitis may need to be treated in a hospital. For some, the only option is to remove the colon. The small intestine will be diverted out of an opening in your abdomen, or it will be used to create an internal pouch connected to your anus.1
Diet cannot cure ulcerative colitis, but it can help manage flare-ups’ symptoms. Eating smaller meals more frequently can help control symptoms as our bodies can digest smaller amounts of food better.3
Diarrhoea caused by ulcerative colitis can cause you to become dehydrated. Dehydration can inflame the digestive tract and the colon, but upping fluid intake can help reduce dehydration symptoms.
Avoiding alcohol and caffeine is essential if you are experiencing diarrhoea, as these can make diarrhoea worse.
Getting enough vitamins and minerals is essential for managing ulcerative colitis.3 You may not be getting enough in your diet or consuming them, but your body isnt absorbing them properly.
If you are experiencing diarrhoea, this likely means your body did not correctly process the food and drink you consumed.
You can take food supplements that a Doctor can prescribe to increase the minerals and vitamins you consume.3
Some Doctors May Use The Following Table To Classify Your Symptoms*:
*A patient does not need to have all of these factors to be considered in a specific category of disease
Ulcerative colitis symptoms are considered moderate when you experience between 4-6 stools per day which include a moderate amount of blood. Severe UC is when you experience 6-10 per day with a severe amount of blood when passing.
If youre concerned about any of your symptoms, talk to your doctor immediately.
You May Like: Can Stress Cause Flare Up Ulcerative Colitis
You May Like: Pressure Ulcer Interventions And Rationales
Treatment Options For Crohns Disease
Recommended treatments may vary based on your symptoms and specific health history.
If you have mild to moderate Crohns disease your doctor may recommend:
- Aminosalicylates, like sulfasalazine
If you have moderate to severe Crohns disease, your doctor may recommend:
- Corticosteroids, such as prednisone and prednisolone
- Immunomodulators, like azathioprine and 6-mercaptopurine
- Methotrexate
- Biologics, like vedolizumab , adalimumab , infliximab , and ustekinumab
If you have severe Crohns disease or an acute flare-up, your doctor may recommend:
- Intravenous corticosteroids, such as methylprednisolone
- Biologics
Regardless of your level of severity, your doctor may prescribe broad-spectrum antibiotics if you have any abscesses or fistulas.
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with inflammatory bowel disease and their loved ones. On MyCrohnsAndColitisTeam, more than 148,000 members come together to ask questions, give advice, and share their stories with others who understand life with Crohns disease and ulcerative colitis.
Are you living with Crohns disease or ulcerative colitis? How was your diagnostic process? Share your experience in the comments below, or start a conversation by posting on your Activities page.
You May Like: Remicade Infusion For Ulcerative Colitis
Recommended Reading: Foods To Eat With Ulcerative Colitis Flare Up
Study Selection And Data Extraction
Two researchers will independently conduct the literature retrieval, literature screening, data extraction and quality evaluation procedures. In case of disagreements, they will consult other researchers and negotiate using the original data. The 2 researchers will identify relevant literature by reading the titles, abstracts, and full-texts of the studies retrieved during the searches with reference to the eligibility criteria mentioned above. The process of study selection will be summarized in the PRISMA flowchart in Fig. Fig.1.1. The search results will be managed by NoteExpress 2.0 . The following information will then be extracted from the studies selected for inclusion using a preestablished literature extraction table: author, article title, year of publication, contact information, country, sample size, participants, diagnosis criteria, baseline characteristics, study design, randomization method, blinding, experimental intervention, control intervention, duration, treatment frequency, outcomes, adverse events, etc. The original authors of any articles which are found to have missing information will be contacted as much as possible in an attempt to obtain the data, or to perform data conversion. If the data does not prove to be available, the study in question will be discarded.
What Is Ulcerative Colitis
- Ulcerative colitis is a form of inflammatory bowel disease, or IBD that affects the large intestine.
- In a person with UC, the lining of the colon becomes inflamed and swollen.
- Symptoms:
Don’t Miss: Is Ulcerative Colitis Genetically Inherited
Safety Of Tumor Necrosis Factor Inhibitors
The safety profile of anti-TNF agents is now fairly well recognized. The potential risks include antidrug antibody formation, delayed hypersensitivity reaction, lupus-like reaction, and skin reactions, such as pustular psoriasis.26 Treatment options for skin toxicities depend on the severity of the reaction. For patients with mild disease, who have a Psoriasis Area and Severity Index score of less than 5%, a topical treatment might be appropriate.27 Severe skin involvement may require a switch to an agent with a different mechanism of action. Another option is to decrease the dose of the anti-TNF agent. It is recognized in the rheumatologic literature that high drug levels may increase the risk of skin-related adverse events.28 Anecdotal data indicate that reducing the dose while using therapeutic drug monitoring might be advantageous.
Another adverse event includes increased mortality in patients with advanced heart failure.29 Although it has been suggested that anti-TNF agents also increase the risk of congestive heart failure, this association has not been well substantiated. Before initiating treatment with a TNF inhibitor, patients should be screened for latent tuberculosis, and, when appropriate, antituberculous chemoprophylaxis should be initiated.