Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
What Are The Risk Factors For Pressure Ulcers:
People with fragile skin are at additional risk, as are people whose nutrition is poor. Diabetes is also a significant risk factor for pressure sores on the feet.
One of the reasons pressure sores are so common among the disabled is that many such people have impaired sensation of pressure and touch due to spinal cord injuries. Because of this, they may not be alerted by pain or discomfort to the need to change position.
People who are bedridden for extended periods may lose a great deal of weight, which reduces the cushioning around their bones, making them more susceptible to pressure sores.
Recommended Reading: Easy To Digest Foods For Ulcerative Colitis
Spotlight On Aging: Pressure Sores
|
Aging itself does not cause pressure sores. But it causes changes in tissues that make pressure sores more likely to develop. As people age, the outer layers of the skin thin. Many older people have less fat and muscle, which help absorb pressure. The number of blood vessels decreases, and blood vessels rupture more easily. All wounds, including pressure sores, heal more slowly. Certain risk factors make pressure sores more likely to develop in older people: |
Causes that contribute to the development of pressure sores include
-
Pressure
-
Friction
-
Moisture
Pressure on skin, especially when over or between bony areas, reduces or cuts off blood flow to the skin. If blood flow is cut off for more than a few hours, the skin dies, beginning with its outer layer . The dead skin breaks down and an open sore develops. Most people do not develop pressure sores because they constantly shift position without thinking, even when they are asleep. However, some people cannot move normally and are therefore at greater risk of developing pressure sores. They include people who are paralyzed, comatose, very weak, sedated, or restrained. Paralyzed and comatose people are at particular risk because they also may be unable to move or feel pain .
Friction can lead to or worsen pressure sores. Repeated friction may wear away the top layers of skin. Such skin friction may occur, for example, if people are pulled repeatedly across a bed.
-
Meticulous hygiene and care of skin
-
Maintaining movement
Icipant Responsiveness To The Care Bundle
I donât think thereâs anything in that training that could make you use them more effectively, you just live and learn. Youâve just got to get used to them I think. .
Initially, the participants were unfamiliar with how to use the bundle and found it to be time-consuming. However, they explained that the time required to complete the bundle decreased with increased familiarity and one participant reported having more time with the residents as a consequence of using the bundle. Despite the low adherence to the whole bundle, the participants reported that the bundle was straight forward to use. Therefore the issues with adherence may have been related to documentation, as highlighted above.
youâre making your colleague aware that youâve seen something because what sees, I might not have seen that day.
You can go and find this you can tick are they red? Yeah tick such a body is red and we know about it and weâve been actively doing something about it. So I think we do need that on the back. .
continence care
I think if it was simplified, people are more likely to pay a bit more attention to what theyâre ticking!
You May Like: Nursing Care Plan For Pressure Ulcer Prevention
Which Interventions Are The Most Important
Pressure ulcers usually heal very slowly, and may come back. That’s why it’s so important to make sure they don’t develop in the first place. People who are confined to a wheelchair or have to stay in bed for a long time often say that they can feel parts of their body becoming sore. It’s important to pay attention to what they say, to quickly reduce pressure on their skin, and regularly change the position they sit or lie in.
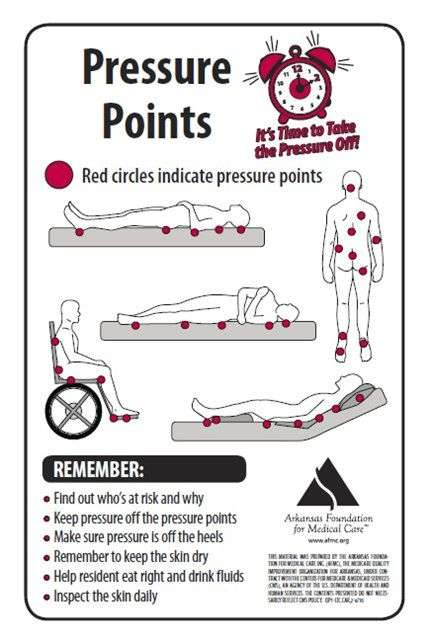
Observing which parts of the body are most susceptible to pressure, as well as the positions that put the most pressure on them, can help you get an idea of what sort of relief might be helpful. For example, lying down puts much less pressure on your backside than sitting in a chair. If you use a wheelchair, you can find out what helps to reduce the pressure and then make that your routine.
It’s also important to try to move if possible even if you have to lie in bed or sit in a wheelchair. If you are able to sit up, leave the bed, or even walk a few steps with a bit of help, its a good idea to do that as often as possible.
Why Do Some People Get Pressure Ulcers
Pressure ulcers or bedsores occur in areas of the skin that are under pressure for a long time. On the following circumstances, there is a possibility of bedsores:
- Lying in bed
- Wearing a cast for a prolonged time
- Friction or rubbing caused by stretching of the skin on the bedding
- Shearing, when the body slides in a chair or bed, then skin slides or pulls away from the supportive tissues below it
Pressure ulcers may be called by other names:
- Pressure injuries
- Bedsores
If an immobile person is not positioned correctly and given good nutrition and skincare, these chronic sores can develop. The risk of pressure ulcers will significantly increase in the following condition:
- Inactivity: People who are unable to move correctly due to injuries such as spinal cord injury are at risk for bedsores.
- Incontinence: In this condition, moisture from urine or stool makes skin weaker and more prone to irritation.
- Lack of sensory perception: Spinal cord injuries and neurological disorders lead to loss of sensation. Consequently, you may not feel any warning signs such as pain or the need to change position.
- Poor nutrition and inadequate hydration: Not using fluids, vitamins, minerals, and other nutrients can impair skin health and make this organ vulnerable.
- Some medical conditions: People with diabetes and vascular diseases are more at risk for bedsores.
Other widely used services of this center are:
Don’t Miss: Stage 2 Pressure Ulcer Characteristics
Prevention Of Bed Sores In Nursing Homes
Steps for Preventing Bedsores
Preventing a bedsore is much easier than treating an existing one. However, a bedsore can still develop even when providing appropriate preventative care on a consistent basis. There are well-established protocols and strategies for providing care to patients with a high propensity of developing a bedsore at home, in a hospital or medical facility.
Bedsores PreventionBedsores are caused by compression of the skin, usually over bony prominences. These areas could include on the ankles, hipbones, tailbone, knees, ankles, elbows, shoulder blades, back of the head and other areas. The compression restricts adequate blood supply to tissue, which can begin to die from lack of oxygen within just a few hours.
Repositioning the individual is a key component to preventing the development of a bedsore. However, position changes need to happen frequently, to minimize any stress on the skin. In addition to repositioning the body to minimize pressure on highly susceptible areas, other effective strategies can help. This includes providing good nutrition and hydration, routine movement when possible, and smoking cessation .
Usually, the patients most susceptible to developing a decubitus ulcer are those challenged with mobility. This could include patients confined to a bed, wheelchair-bound due to a medical condition, paralysis or in a coma.
Steps for the Wheelchair-Bound to Prevent Pressure Wounds
Wound Care Prevention Steps for the Bed Bound
Encourage Seniors To Maintain A Healthy Diet
The benefits of a well-functioning circulatory system are only as good as the nutrients it delivers. Seniors should strive to eat a well-balanced, healthy diet, explains Medscape. In fact, optimizing the nutritional status of a senior living with a pressure sore is key to ensuring successful treatment. For seniors living with metabolic disorders, such as diabetes, a healthy diet can go much further than simply preventing or encouraging the healing of pressure sores.
You May Like: Best Acid Reducer For Ulcer
What Are The Risk Factors For Bedsores
Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care. People with diabetes, circulation problems and malnutrition are at higher risk.
Implementing A Prevention Plan
Preventing pressure ulcers can be nursing intensive. The challenge is more difficult when there is nursing staff turnover and shortages. Studies have suggested that pressure ulcer development can be directly affected by the number of registered nurses and time spent at the bedside., In contrast, however, one recent study suggested that there was no correlation between increasing the nurse-to-patient ratio and the overall incidence of pressure ulcers. Donaldson and colleagues noted that this particular study was limited by the fact that the researchers could not affirm compliance with ratios per shift and per unit at all times. Given that the cost of treatment has been estimated as 2.5 times that of prevention, implementing a pressure ulcer prevention program remains essential.
A key component of research studies that have reported reduction of pressure ulcers is how to sustain the momentum over time, especially when the facility champion leaves the institution. It is clear from the evidence that maintaining a culture of pressure ulcer prevention in a care setting is an important challenge, one that requires the support of administration and the attention of clinicians.
Recommended Reading: How Do They Treat Ulcerative Colitis
What Is The Best Method To Prevent Pressure Ulcers
What is the best method to prevent pressure ulcers?T o fully implement evidence- based practice , nurses need to have both
a spirit of inquiry and a culture that supports it. Inour first article in this series ,we defined a spirit of inquiry as an ongoing curiosity about the best evidence toguide clinical decisionmaking. A spirit of inquiry is the founda- tionof EBP, andonce nurses pos- sess it, its easier to take the next steptoask the clinical question.1
Formulating a clinical question in a systematicwaymakes it pos- sible to find an answermore quickly and efficiently, leading to improved processes and patient outcomes. In the last installment,wegave
an overviewof themultistepEBP process . Thismonthwell discuss step one, asking the clinical question. As a context for this discussionwell use the same
scenariowe used in the previous articles . In this scenario, a staff nurse,
lets call herRebeccaR., noted that patients on hermedical surgical unit had a high acuity level thatmay have led to an in- crease in cardiac arrests and in the
number of patients transferred to the ICU.Of thepatientswho had a cardiac arrest, four died. Rebecca sharedwith her nurse manager a recently published study onhow the use of a rapid response teamresulted in reduced in-hospital cardiac arrests andun- planned admissions to the critical
Asking the Clinical Question: A Key Step in Evidence-Based Practice
A successful search strategy starts with a well-formulated question.
furosemide peak?
How Are Pressure Sores Diagnosed
Your doctor will do a physical exam to look at the sores. They will examine the size and depth of the sore and look to see if blood or fluid is oozing from the sore. Your doctor will check to see if your sore has a bad smell. They also will check for additional sores.
Testing may help to diagnose pressure sores or their complications. These tests might include a blood test. Another test would be to take a sample of the tissue from the sore. This is done by scraping or cutting it from the sore. That sample is sent to the lab for examination.
You May Like: List Of Foods Good For Ulcers
Signs And Symptoms Of Pressure Ulcers
A pressure ulcer is a lesion that forms when tissue under the skin is squashed by excessive localized pressure, leading to abnormal blood flow. The condition can be painful and can cause other problems, including loss of fluids. The best ways to prevent them are to follow your doctors advice about chronic conditions and watch for the following signs and symptoms: Painful skin that is red, hot and swollen with areas of open bleeding. Pus or blood coming from the wound. A pressure ulcer is a skin infection that can become severe and even life threatening if it goes untreated. Most pressure ulcers are caused by prolonged periods of sitting or lying in one position, but they can also develop from chronic conditions such as diabetes, cancer, or rheumatoid arthritis. Signs and symptoms include redness, swelling, pain, and open sores that dont heal as quickly as they should.
What Causes Bed Sores In The Elderly
Three main factors contribute to the formation of bed sores:
- Pressure: Persistent pressure that compromises the blood flow to a localized body area is the leading cause of bed sores. As noted, without oxygen and nutrients, our cells will die. Damage starts from the skin and moves deeper toward the bones.
- Friction:Can lying on a towel cause bed sores in elderly patients? Yes, friction against rough towels, clothing, and bedding can make fragile skin vulnerable to injury. Furthermore, moisture makes things even worse.
- Shear: This occurs when two surfaces move in the opposite direction. For instance, when you elevate the bed, you may slide down, but your skin may stay in place. Shearing in areas where very little tissue separates skin and bones can damage it.
Recommended Reading: What Is Refractory Ulcerative Colitis
First Cycle Of Unfreezing: Planning
In this stage, there were some activities to come up with a preliminary diagnosis of the problem, gather data, and giving feedback on the results and the plan for action. The first author and the trained research assistant met several key people including the in-charge and experienced HWs or nurses selected by the in-charge of each NH to learn the issues relevant to pressure ulcers in their homes. They reported on the existing PUs but did not have record of the incidence of PUs. The prevalence of PUs in these four homes ranged from 8 to 10%. Overall, the residence-staff ratio was around four to six. The turnover rate of care staff was acceptable, although this sometimes affected the care that was delivered. They agreed that the occurrence of PUs was an important issue in their homes, and efforts e.g., having a prevention protocol and training to care staff should be made to decrease them.
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Recommended Reading: Can You Take Tylenol With Ulcerative Colitis