What Types Of Testing Can Be Done To Identify The Cause Of Chronic Diarrhea
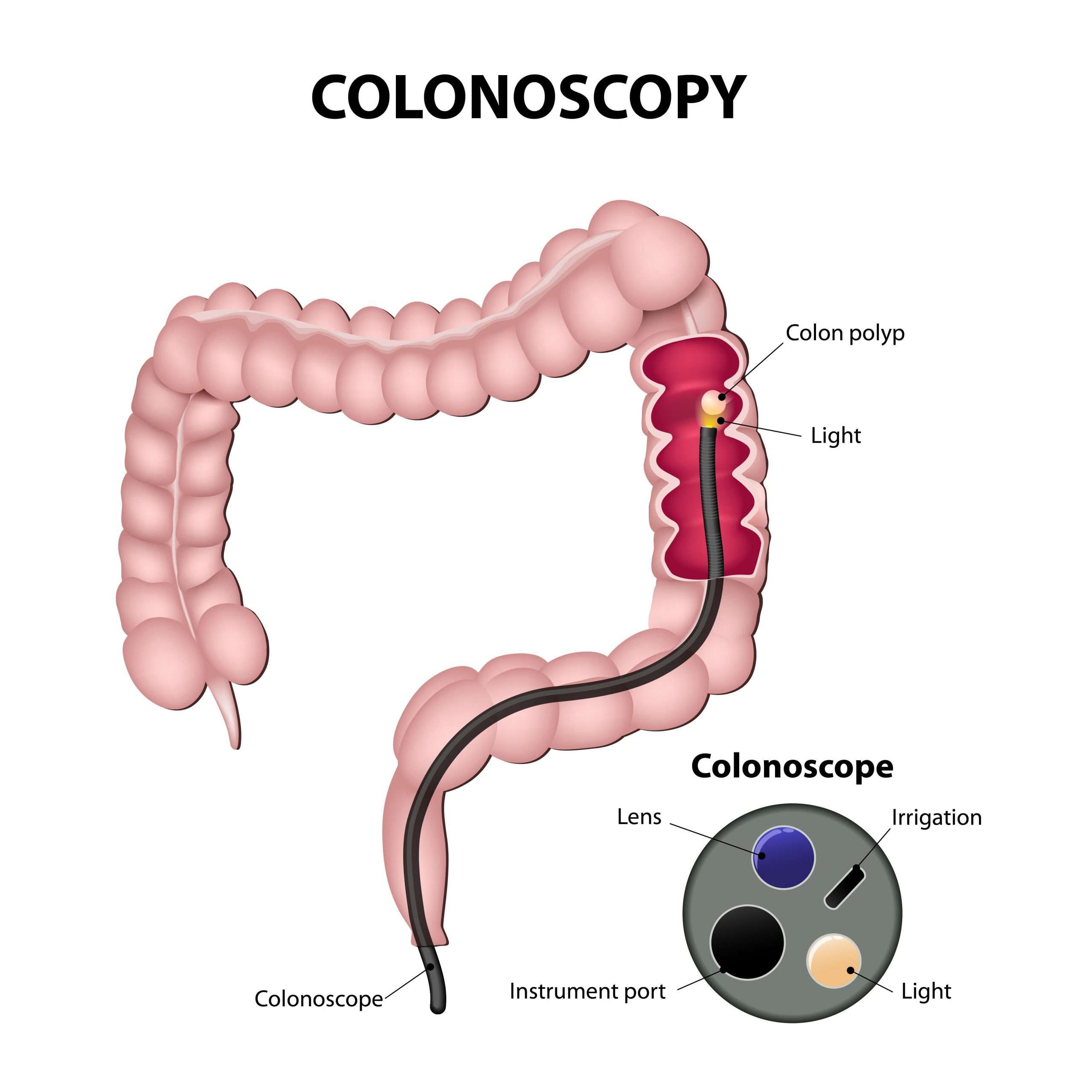
Chronic diarrhea is a sign that nutrients are not being well enough absorbed during the digestive process. Patients who have chronic diarrhea will often undergo blood tests to guide replacement of fluids, electrolytes, and minerals. A blood test can also identify whether the diarrhea is being caused by anemia or a bacterial infection.1
Patients with chronic diarrhea may also undergo fecal testing in order to accurately diagnose the cause. The presence of white blood cells indicates inflammation in the body, potentially due to IBD. If parasites or bacterial cultures are present in the stool sample, this could be the cause of diarrhea.
Which Drugs Or Supplements Interact With Loperamide
Cholestyramine binds to loperamide in the intestines and prevents its absorption, thereby reducing the effect of loperamide. Therefore, there should be at least a two-hour interval between doses of loperamide and cholestyramine.
Theoretically, some drugs that are used to increase propulsion of intestinal contents could counteract loperamide. Such drugs include bethanechol , cisapride , metoclopramide , and erythromycin.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
You May Like: Food To Avoid For Ulcer Patient
Also Check: Turning Patients Every 2 Hours To Preventing Pressure Ulcers
Moderate Or Extensive Disease
Patients with inflammation proximal to the sigmoid colon or left-sided disease unresponsive to topical agents should receive an oral 5-ASA 5-Aminosalicylic Acid Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder or corticosteroid therapy as well as those who are corticosteroid-dependent. Moreover, a combination of immunomodulator and anti-TNF therapy Anti-TNF drugs Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder (see Crohn disease treatment and ulcerative colitis… read more is sometimes helpful. Finally, in some patients who fail to respond to corticosteroids, immunosuppressants, or biologics, a trial of the Janus kinase inhibitor tofacitinib, or a trial of sphingosine 1-phosphate receptor modulator ozanimod can be considered.
Are Your Ulcerative Colitis Symptoms Under Control

She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
You May Like: Is Ulcerative Colitis Caused By Stress
Can Loperamide Cause Problems
Along with their useful effects, most medicines can cause unwanted side-effects although not everyone experiences them. The table below contains some of the most common ones associated with loperamide. You will find a full list in the manufacturers information leaflet supplied with your medicine. The unwanted effects often improve as your body adjusts to the new medicine, but speak with your doctor or pharmacist if any of the following continue or become troublesome.
| Common loperamide side-effects | |
| Drink plenty of water and ask your pharmacist to recommend a suitable painkiller. | |
| Feeling sick | Try taking loperamide after eating some food if you are not already doing so |
If you experience any other symptoms which you think may be due to loperamide, speak with your doctor or pharmacist for further advice.
What Is The Most Important Information I Should Know About Loperamide
You should not use loperamide if you have ulcerative colitis, bloody or tarry stools, diarrhea with a high fever, or diarrhea caused by antibiotic medication.
Loperamide is safe when used as directed. TAKING TOO MUCH LOPERAMIDE CAN CAUSE SERIOUS HEART PROBLEMS OR DEATH.
Serious heart problems may also happen if you take loperamide with other medicines. Ask a doctor or pharmacist about safely using medications together.
Do not give loperamide to a child younger than 2 years old.
Also Check: Acute Exacerbation Ulcerative Colitis Symptoms
What Happens If I Overdose
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose of loperamide can be fatal.
Overdose symptoms may include fast or irregular heartbeats, or fainting. A person caring for you should seek emergency medical attention if you pass out and are hard to wake up.
Never exceed the recommended dose for loperamide. The maximum dosage of loperamide in adults and children over the age of 13 years is 16mg per day .
Medication Is Often Not Enough For Helping With Ulcerative Colitis Flareups Supplementing With Psyllium Husk Can Go A Long Way In Helping With Remission
Irritable bowel diseases are skyrocketing around the globe. There are about 1.6 million people in America alone who suffer from IBD. The most common form of IBD is a disease known as ulcerative colitis which is an autoimmune disease and a chronic inflammation of the larger intestine. The disease is characterized by bloating, abdominal pain, diarrhea and blood as a result of ulcers in the gut.
There is no known cure for the disease, but its symptoms are manageable with conventional anti-inflammatory medication like prednisone.
Medication is not enough to control and manage UC symptoms. Many chronic sufferers of the disease must cut back on milk, fried foods, spicy foods, certain kinds of seeds etc as they may exacerbate symptoms or take people out of remission.
Does Psyllium Husk Help with Ulcerative Colitis?
There are, however, some natural supplements that have shown much promise in treating IBDs, particularly ulcerative colitis. From our experience, the most effective natural supplement to help with UC is psyllium husk. Psyllium husk is a smooth insoluble form of fiber. It not only helps with constipation but it also helps with diarrhea. In this sense, psyllium husk acts as a colon cleans which may remove certain toxic and non-toxic elements that may be contributing to your flare-up.
Not only does it help prolong remission, but it also has a healing effect on the colon by repairing the protective lining system in the colon which also reduces flare-ups.
Read Also: How To Know If You Have Ulcerative Colitis
What Is Loperamide How Does It Work
Loperamide is a medication that is used for the relief of acute diarrhea and the management of chronic diarrhea in patients with inflammatory bowel disease . The effectiveness of loperamide is comparable to another anti-diarrheal, diphenoxylate . Loperamide reduces diarrhea by slowing the forward propulsion of intestinal contents by the intestinal muscles. Although loperamide is related chemically to narcotics such as morphine, it does not have any of narcoticspain relieving effects even at high doses.
Loperamide was approved by the FDA in 1976.
Can Imodium Make You Feel High
No, taking Imodium at the recommended dosage to treat diarrhea wont make you feel high. At this dosage, Imodium doesnt affect your brain. Instead, it only works inside your intestine.
However, Imodiums chemical structure is similar to that of opioids, such as morphine and heroin. If its misused and taken in extremely large doses, Imodium can affect your brain. And if it enters your brain, it may make you feel high.
Some people misuse Imodium in this way to make themselves feel high. But you shouldnt misuse Imodium, because doing so can have serious effects on your heart. .
If you have questions about how Imodium may affect you, talk with your doctor or pharmacist.
Dont Miss: How To Ease Mouth Ulcer Pain
Recommended Reading: How Do You Get Ulcers On Your Legs
Dietary Modifications For Ulcerative Colitis Pain
There is no single diet that will work for everyone with UC. Thats why its important to have a very clear conversation with your doctor about what foods you seem to tolerate, especially during a flare of your symptoms. There are some foods that may make your symptoms worse, according to the Crohns and Colitis Foundation. These include foods that are hard to digest such as seeds, nuts, broccoli, and cauliflower. You may also want to experiment by reducing your intake of high lactose foods such as milk and cheese to see if these are making your pain worse. Eliminating foods high in sugar and fat may also provide some relief.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Dont Miss: Can Ulcerative Colitis Go Into Remission
You May Like: Is Alcohol Bad For Ulcerative Colitis
Dealing With Side Effects
Symptoms And Signs Of Ulcerative Colitis
Patients typically have
-
Attacks of bloody diarrhea of varied intensity and duration interspersed with asymptomatic intervals
Usually an attack begins insidiously, with increased urgency to defecate, mild lower abdominal cramps, and blood and mucus in the stools. Some cases develop after an infection .
When ulceration is confined to the rectosigmoid, the stool may be normal or hard and dry, but rectal discharges of mucus loaded with red and white blood cells accompany or occur between bowel movements. Systemic symptoms are absent or mild.
If ulceration extends proximally, stools become looser and the patient may have > 10 bowel movements per day, often with severe cramps and distressing rectal tenesmus, without respite at night. The stools may be watery or contain mucus and frequently consist almost entirely of blood and pus.
Toxic or fulminant colitis manifests initially with sudden violent diarrhea, fever to 40° C , abdominal pain, signs of peritonitis , and profound toxemia.
Also Check: What Makes Stomach Ulcers Feel Better
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
What Are The Possible Side Effects Of Loperamide
Get emergency medical help if you have signs of an allergic reaction or a severe skin reaction .
Stop taking loperamide and call your doctor at once if you have:
- diarrhea that is watery or bloody
- stomach pain or bloating
- ongoing or worsening diarrhea or
- fast or pounding heartbeats, fluttering in your chest, shortness of breath, and sudden dizziness .
Common side effects may include:
- stomach cramps.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Recommended Reading: Meal Replacement Shakes For Ulcerative Colitis
How Do You Stop Diarrhea With Ulcerative Colitis
4.4/5diarrhea
You may need additional medications to manage specific symptoms of ulcerative colitis. For severe diarrhea, loperamide may be effective. However, use anti-diarrheal medications with great caution and only after talking with your doctor.
Also Know, how long does diarrhea last with colitis? The diarrhea can vary from loose stools to dysentery with grossly bloody and purulent feces. Symptoms arise 8 to 48 hours after ingestion of contaminated food. The illness lasts for 3 to 5 days in patients manifesting with gastroenteritis and 2 to 3 weeks in patients who develop enterocolitis.
Also asked, why do I have diarrhea with ulcerative colitis?
Ulcerative colitis is a chronic inflammatory disease that affects the lining of the large intestine and rectum. People with this condition have tiny ulcers and small abscesses in their colon and rectum that flare up periodically and cause bloody stools and diarrhea.
Can you take Imodium with colitis?
You should not use loperamide if you have ulcerative colitis, bloody or tarry stools, diarrhea with a high fever, or diarrhea caused by antibiotic medication. Loperamide is safe when used as directed. TAKING TOO MUCH LOPERAMIDE CAN CAUSE SERIOUS HEART PROBLEMS OR DEATH.
Also Check: Venous Leg Ulcer Dressing Treatment
When To Contact A Doctor
Let a doctor know about new or worsened UC symptoms. Also, never take leftover prednisone without first talking with a doctor.
A doctor can provide detailed instructions about when and how to take prednisone. They can also monitor how it affects UC symptoms and check for side effects.
Prednisone is only suitable for short-term use, and taking it for too long increases the risk of complications, including severe
Recommended Reading: What To Do If You Have A Stomach Ulcer
From Stabbing Sensations To Major Cramps Uc Pain Can Be Debilitating Heres What To Expectand How To Get Relief
by Health Writer
If youve recently been diagnosed with , you know: It can be hard to separate out symptoms of this gastrointestinal disease from the other aches and pains in your body. Is that stomachache due to a meal that didnt agree with you, or is caused by inflammation in your colon? Are those cramps related to your inflammatory bowel disease or your monthly cycle? Lets take a closer look at symptoms that make UC abdominal pain different from a run-of-the-mill stomachache, plus how to relieve the pain so you can get back to the things you love.
Treatment Of Ulcerative Colitis
If fulminant or toxic colitis is suspected, the patient should
-
Stop all antidiarrheal drugs
-
Take nothing by mouth and have inserted a long intestinal tube attached to intermittent suction
-
Receive aggressive IV fluid and electrolyte therapy with 0.9% sodium chloride, and potassium chloride and blood as needed
-
Receive high-dose IV corticosteroids or cyclosporine
-
Receive antibiotics
-
Perhaps receive infliximab
Having the patient roll over in bed from the supine to prone position every 2 to 3 hours may help redistribute colonic gas and prevent progressive distention. Insertion of a soft rectal tube may also be helpful but must be done with extreme caution to avoid bowel perforation. Even if decompression of a dilated colon is achieved, the patient is not out of danger unless the underlying inflammatory process is controlled otherwise, colectomy will still be necessary.
If intensive medical measures do not produce definite improvement within 24 to 48 hours, immediate surgery is required or the patient may die of sepsis caused by bacterial translocation or even perforation.
You May Like: Acute Ulcerative Colitis Icd 10
Prognosis For Ulcerative Colitis
Usually, ulcerative colitis is chronic with repeated exacerbations and remissions. In about 10% of patients, an initial attack becomes fulminant with massive hemorrhage, perforation, or sepsis and toxemia. Complete recovery after a single attack occurs in another 10%.
Patients with localized ulcerative proctitis have the best prognosis. Severe systemic manifestations, toxic complications, and malignant degeneration are unlikely, and late extension of the disease occurs in only about 20 to 30%. Surgery is rarely required, and life expectancy is normal. The symptoms, however, may prove stubborn and refractory. Moreover, because extensive ulcerative colitis may begin in the rectum and spread proximally, proctitis should not be considered localized until it has been observed for ⥠6 months. Localized disease that later extends is often more severe and more refractory to therapy.
Pregnancy And Breast Feeding
Loperamide is not recommended in the United Kingdom for use during pregnancy or by nursing mothers. In the U.S., loperamide is classified by the U.S. Food and Drug Administration as pregnancy category C. Studies in rat models have shown no teratogenicity, but sufficient studies in humans have not been conducted. One controlled, prospective study of 89 women exposed to loperamide during their first trimester of pregnancy showed no increased risk of malformations. This, however, was only one study with a small sample size. Loperamide can be present in breast milk, and is not recommended for breast-feeding mothers.
Don’t Miss: Off Loading Shoe For Heel Ulcer