Easing Symptoms During A Flare
The below suggestions can also help ease symptoms or help keep your body healthy during a flare-up.
Drink water: In UC, the large intestine can have a hard time absorbing water and salt, which can contribute to diarrhea and dehydration. Drinking plenty of water or an electrolyte replacement drink can help avoid dehydration if youre experiencing a flare.
Eat plain, easy-to-digest foods: During a UC flare, its common to lose your appetite. To keep your energy levels up and avoid malnutrition and weight loss, its important to continue to fuel your body with food. Unfortunately, fruits and vegetables, particularly when raw, are bothersome for many people with UC. Avoid fatty and greasy foods as well. Your doctor may also suggest meal replacement drinks if youre losing weight from UC flare-ups.
Get some exercise: If youre experiencing symptoms like stomach pain and diarrhea, exercise may sound like the last thing you want to do. But in addition to the well-known mood and health-boosting benefits of exercise, a workout can also have specific benefits for UC symptoms. Uncontrolled inflammation in the intestinal tract leads to UC symptoms. Exercise has an anti-inflammatory effect that can help these symptoms.
Also Check: What To Drink For Stress And Anxiety
Functioning Of The Stress Axes In Animal Models Of Ibd
There have been no studies to assess the functioning of the stress axes in animal models of IBD. However, it has been shown that reduced HPA axis function renders rodents susceptible to stress induced increases in gastrointestinal inflammation. If, as discussed above, HPA axis function is reduced in patients with IBD, this observation may be relevant to stress induced increases in disease activity. LEW/N rats have a reduced CRF content of the hypothalamus and paraventricular nucleus compared with controls. They have a markedly decreased plasma ACTH and corticosterone response to stressful stimuli, and have long been recognised as being more susceptible to inflammatory disorders such as the arthritis induced by intra-articular injections of streptococcal cell wall. LEW/N rats also show an increased susceptibility to TNBS induced colitis, an effect which was found to be dependent on coexisting stress. Thus although stress naive animals developed a similar degree of intestinal inflammation to control rats at seven days after TNBS administration, intestinal inflammation was greater in LEW/N rats than in appropriate control animals if they were restrained for six days prior to being given TNBS.
Implications For Therapy Of Ibd
If psychological stress is indeed a pathogenic factor in IBD, then stress reduction therapy may have therapeutic benefit. However, despite recent advances in our understanding of the relationship between psychological stress and IBD, most stress reduction therapy remains unformalised, and studies of its efficacy in patients with IBD are few. There are a wide variety of psychotherapeutic interventions which could be assessed making standardisation difficult. Due to the nature of the intervention, performing the trials in a blinded controlled manner is also difficult and, as already discussed, with placebo rates of up to 40% genuine therapeutic effects can be hard to detect.
In summary, further trials are required before a view can be taken as to whether any form of stress reduction therapy may have benefit for patients with IBD. However, given the considerable evidence both in humans with IBD and in animal models of IBD that stress can increase disease activity, perhaps such studies should now be attempted.
Also Check: When Was Ulcerative Colitis Discovered
Digestive Health Support Strategies
Conventional treatment options for ulcerative colitis include medications to reduce symptoms and surgery. These treatments may have serious negative side effects.
Fortunately, alternative natural strategies, including dietary changes and targeted supplementation, may improve digestive health and improve the inflammatory response. While none of these strategies are FDA approved to prevent, mitigate, treat or cure ulcerative colitis many people have benefited greatly from implementing them.
Acute Psychological Stress And Gastrointestinal Immune And Inflammatory Function

Both of the two small studies which have examined the role of acute daily stress in IBD suggest a positive association between disease relapse and exacerbation .
There have been few examinations of the effects of experimental stress on gastrointestinal inflammation in humans. One study did find that physical stress, induced by immersion of the hand in iced water, increased the luminal jejunal concentration of the mast cell mediators tryptase and histamine in healthy volunteers and even more so in those with food allergies. We have found that acute psychological stress in the form of a dichotomous listening test increases the production of reactive oxygen metabolites by rectal mucosal biopsies in patients with quiescent UC .
There is also limited anecdotal evidence that artificially induced alterations in neural function can affect gastrointestinal inflammation. One reported example is of a man whose previously refractory UC went into complete remission following a Brown-Sequard paralysis at the level of C5. Kemler described a patient who suffered recurrent flares of his UC in association with spinal cord stimulation given for post-traumatic pain in his arm. Neuromodulatory drugs such as lidocaine, which decreases neuronal release of SP, clonidine, and nicotine have been claimed for many years to have benefit in UC in clinical trials and remain potential therapeutic agents in IBD.
Don’t Miss: Ulcerative Colitis And Crohn’s Disease Differences
Encountering Emotional Stressors And Facing Them
Possible Emotional Stressors
Other Peoples Perception of UCIts hard if you feel isolated because people around you dont understand how your condition affects you. The symptoms of UC can often be invisible on the outside and you could be worried that others may see you differently because of your condition.
Ways You Can Face Them
Refuse to Suffer in SilenceIf youre concerned that others dont understand what youre going through, try your best to talk about it. Open up and crush the stigma. Educate others that may not understand the facts and let go of the people who refuse to understand. Keep the people who really want to understand and support you close.
Having Symptoms at Work or SchoolWorrying about how to manage your UC symptoms when youre not in the comfort of your own home can be hard. Especially if you arent getting what you need, like a flexible schedule or support from your boss. And while you may know your rights as a patient with a medical condition, sometimes there are negative impacts, like unsupportive people, that are outside your control.
Being in Social SituationsIt can feel easy to stay isolated and keep yourself at home. But every now and then everyone needs to get out and have fun. Thinking of your UC might hinder you from doing things like going to parties, seeing friends, or attending events.
Possible Emotional Stressors
Gi Map Stool Analysis
The GI-MAP Stool Analysis Test is the most thorough stool test on the market. It is the only FDA-approved DNA test for gastrointestinal microbes and pathogens available. This test includes calprotectin which is a reliable marker for the detection of colonic mucosal inflammation in ulcerative colitis .
The GI Map measures imbalances in the gut microbiome which are common with ulcerative colitis. It also tests for candida and other fungi, and parasites, including both protozoa and worms. This comprehensive stool test can reveal if you have H. pylori, viral pathogens, potential autoimmune triggers, and viruses, including cytomegalovirus and Epstein Barr virus. These bacteria and virus may contribute to the development and worsen symptoms of ulcerative colitis.
The GI Map also reveals the integrity of your gut mucosa with digestion, gastrointestinal, and Secretory IgA levels. This is an important test for anyone with ulcerative colitis. For more information on the GI-MAP and how to order, go here.
Recommended Reading: Ulcerative Colitis Bloating And Constipation
How Stress Messes With Your Immune Response
If you are living with UC, stress talk gets elevated to a whole new level. Thats because UC is an inflammatory bowel disease that already causes inflammation in your digestive tract. So when you are experiencing stress, it can trigger even more inflammation in your body, leading to a worsening of UC symptoms. Stress affects UC as it would any chronic illness, says Loren Brook, M.D., a gastroenterologist at the University of Cincinnati College of Medicine in Ohio. Stress may increase your chances of flares and is known to weaken the immune system.
When you are stressed, the increase in cortisol can increase the pro-inflammatory cytokines and therefore cause increases in inflammation of the gut which has a negative effect on UC, says Bottoms. This also means your general immune system is not as effective and may struggle to fight against other illnesses as well.
The Relationship Between Stress & Colitis
The systemic effects of psychological stress on the immune and inflammatory systems are complex, and experts believe that both chronic and acute stress is associated with colitis, in terms of encouraging the inflammation that leads to colitis flare-ups. The duration and intensity of the colitis reaction most likely relate directly to the duration and intensity of the stressor. For example, adverse life events or difficult situations, such as being a caregiver or going through a marital separation are more likely to trigger more severe colitis symptoms than a bad day at work or an argument with your best friend.
Stress may not directly cause the condition of ulcerative colitis, but it can aggravate symptoms of the condition and increase the risk, frequency, and severity of flare-ups. And severe, chronic psychological stress may lead to increased bowel inflammation. Also, colitis patients who also live with chronic anxiety are at a higher risk for requiring surgeries, reduced medication adherence, lower quality of life, and higher perceived level of stress. In other words, left unchecked, your stress and anxiety may lead to additional and increased stress and anxiety.
Breaking the GI Stress Cycle can be as simple as focusing on taking deep, diaphragmatic breaths and muscle relaxation can begin to slow the sympathetic arousal mechanisms.
Don’t Miss: Colon Cleanse For Ulcerative Colitis
Stress: A Factor For Ulcerative Colitis Flareups And Its Management
Abstract
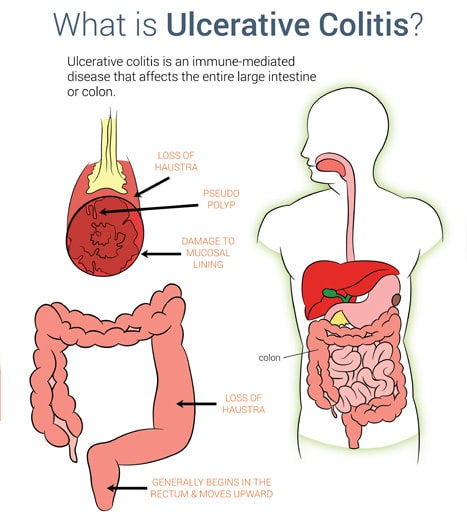
Stressful life events always create a disturbance in the normal life of any organism and thus is a threat to the homeostasis. This triggers off a physiological response which needs adaptation and response. Mild stress may subside over a period of time but if stress continues, it can cause damage and exacerbation of disease process. One such disease related to stress is ulcerative colitis. It was first described in mid-1800s. Ulcerative colitis is an idiopathic disease with chronic inflammation of the colonic mucosa. It commonly involves the rectum and can extend in a proximal and continuous fashion and other parts of the colon are affected. Though there is still a controversy over the role of psychosocial factors in the development and modulation of common gastrointestinal disorders, but researches do establish bidirectional interactions between the brain and gut, and that certain stressful life events frequently precede exacerbation of symptoms in gastrointestinal disorders.
Medication For Inflammatory Bowel Disease In Adults
Gastroenterologists at NYU Langones Inflammatory Bowel Disease Center may prescribe one or more medications to reduce inflammation in the digestive tract caused by inflammatory bowel disease, or IBD. The goals of treatment are to improve symptoms and heal any damage to the intestines.
Our gastroenterologists develop a personalized treatment plan for you based on the type of IBD, the severity of the condition, and the results of diagnostic tests. These tests may have confirmed that you have Crohns disease, which can affect any part of the gastrointestinal tract, or ulcerative colitis, which only affects only the colon, or large intestine.
Medications work differently in different people, so your gastroenterologist closely monitors how well you respond to treatment. He or she adjusts the type or dose of medication as often as needed.
Medications for IBD can often reduce inflammation and promote healing in the intestines, resulting in remissionmeaning long-term symptom relief. However, for many people with IBD, the condition is chronic and treatment is lifelong. It is very important to follow up regularly with your gastroenterologist.
Dont Miss: Can You Get Acid Reflux From Stress
You May Like: History Of Ulcerative Colitis Icd 10
The Role Of Peripheral Substance P
In addition to its central effects, peripheral release of SP from the ENS may have a role in stress induced increases in mucosal inflammation. Although there are no published data to show an increase in mucosal SP in response to stress, SP containing neurones are found in close association with mast cells, a cell type implicated as central in mediating stress induced permeability changes . SP has been shown to increase histamine release from mucosal mast cells in patients with IBD. Lastly, SP can act not only as a neurotransmitter but also an inflammatory cytokine in its own right, enhancing cytokine production and stimulating chemotaxis of inflammatory cells. It also increases expression of leucocyte adhesion molecules on microvascular endothelium, and of CD11b on neutrophils, facilitating leucocyte adhesion at sites of inflammation.
Can I Treat Ibd If I Am Pregnant Or Breastfeeding
Yes, but your doctor may change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31
Before you get pregnant, make a plan with your obstetrician and gastroenterologist about the medicines you will take during and after pregnancy. Take your medicines as your doctor tells you to. If you stop taking your medicines and your symptoms come back , it may be difficult to get them back under control.31
Talk with your doctor about your medicines and breastfeeding before you give birth. You can search for your medicine in the LactMed database to find out if your medicine passes through your breastmilk and, if so, if it has any possible side effects for your nursing baby.
Also Check: Low Sulfur Diet Ulcerative Colitis
Coffee Enemas To Clear The Colon
Compared to colonics, enemas are done at your home in private. They are inexpensive compared to a more costly visit to your colon hydrotherapist. You can buy kits at any drugs store or online. Here is a great stainless steel kit that I recommend.
Enemas also work by cleansing your colons with water. In some cases, coffee, wheatgrass, herbs, or apple cider vinegar is added for extra cleansing. While colonics target your entire intestine, enemas are targeting your descending colon only. Here is a helpful article on how to do a coffee enema.
If you choose to get a colonic or try an enema yourself, it is important that you take probiotics to support your healthy gut flora. Colonics clean your colon from waste, toxins, bacteria, fungi, and parasites. However, they also clean out good bacteria in the process.
Taking high-quality probiotics and eating a nutrient-dense, gut-supporting diet is important to achieve long-term results. Continue reading for further tips on how to reset your microbiome after a colon cleanse.
Recommended Reading: How Does Ulcerative Colitis Affect The Digestive System
Tips For Managing Anxiety When You Have Ulcerative Colitis
Learning how to cope with daily stressors will help manage UC-related anxiety.
Sam Cleasby was 23 years old when she was diagnosed with ulcerative colitis an inflammatory bowel disease that causes chronic inflammation and sores in the gut. Medication kept her flare-ups under control for nearly a decade. But in 2013, Cleasby required surgery to keep her disease under control. First, doctors removed her colon. Then they created an ileostomy, in which a piece of the small intestine is pulled through an opening in the abdomen so digested food can pass through a pouch called an ostomy bag, which she wears on the outside of her body. Later, they removed her entire large intestine.
Though I had times when life was tough and I was sad, frustrated, or angry, I didnt actually struggle with anxiety and my mental health until after surgery, says Cleasby, founder of the blog SoBadAss, who says she also suffers from post-traumatic stress disorder . It wasnt the surgeries themselves but the loss of control that was the source of my panic attacks and anxiety, explains Cleasby.
In addition to coping with their illness, people with UC have to manage doctors appointments, medication, and changes to their lifestyle and eating habits, says Mira Zein, MD, a psychiatrist with Stanford Health Care in California. Flare-ups can also put a damper on socializing.
You May Like: What Makes Stomach Ulcers Feel Better
Points To Remember: Psychological Stress In Ibd
-
Recent studies indicate that chronic stress, adverse life events, and depression can cause relapse in patients with IBD.
-
The effects of stress on inflammation in IBD are likely to be mediated through changes in hypothalamic-pituitary-adrenal function, alterations in bacterial-mucosal floral interactions, activation of mucosal mast cells, and peripheral release of corticotrophin releasing factor.
-
The symptoms of IBD may be exacerbated by the effects of stress on gut motility and fluid secretion.
-
There is a need for further controlled studies of the potential benefits of stress reduction therapy in IBD.
You May Like: Can Stress Cause Loss Of Appetite
Stress Can Trigger A Flare
Both Crohns disease and colitis are inflammatory diseases and can cause a variety of uncomfortable symptoms including:
- Blood in your stool
Inflammation in your GI tract causes these symptoms, and many people experience inflammation in cycles. This means you might have a handle on your symptoms and then suddenly something triggers a flare-up.
A flare-up is a reappearance of your symptoms. There are many things that can trigger a flare-up including missing your medication or taking the wrong dose, eating foods that irritate your GI tract, or even drinking carbonated beverages.
Many studies also show that stress can trigger a flare-up. Stress doesnt have to be a big event like moving to a new house. Everyday stressors can trigger a flare-up.
But why does an everyday stressor affect your gut health? The brain and digestive system are connected. This brain-gut connection allows your stomach to prepare for a meal by releasing stomach acids when you start thinkingabout food.
But the brain-gut connection goes both ways, which means mental stress can affect your gut health. This explains why you might feel butterflies in your stomach if youre nervous.
This, unfortunately, also explains how psychological stress can impact your digestive health and trigger a flare-up in your symptoms.
Don’t Miss: When Does Ulcerative Colitis Develop