When To See Your Doctor
If you begin to see blackened flesh around an area of numbness, see your doctor right away to seek treatment for an infected foot ulcer. If untreated, ulcers can cause abscesses and spread to other areas on your feet and legs.
At this point, ulcers can often only be treated by surgery, amputation, or replacement of lost skin by synthetic skin substitutes.
Proper Dressing Infection Control And Offloading
Its essential to use the proper types of wound dressing, infection control, and offloading to prevent your diabetic wound from regressing during or after treatment.
The best wound dressing maintains a healthy amount of moisture on the foot to create a favorable environment for the wound. It must be changed at least once or twice per day, depending on the stage and severity of the ulcer. Wound dressing helps control infection, as do antibiotics.
Offloading is also a very important but often overlooked component of diabetic foot ulcer treatment. When you offload, you remove pressure from your injured foot and give new, healthy cells the opportunity to thrive. Crushes, knee scooters, and wheelchairs all accomplish offloading.
Tea Tree Oil To Fight The Infection
Tea tree oil is rich in antibacterial properties. You can mix the tea tree oil in equal quantity with coconut oil and use it for dressing the diabetic foot ulcer. You can even keep the wound open for some time after applying the tea mixture of tea tree and coconut oil. This home treatment of diabetic foot hastens the process of healing of the wound.
Don’t Miss: Budesonide Uceris For Ulcerative Colitis
Identifying Symptoms And Diagnosis
One of the first signs of a foot ulcer is drainage from your foot that might stain your socks or leak out in your shoe. Unusual swelling, irritation, redness, and odors from one or both feet are also common early symptoms.
The most visible sign of a serious foot ulcer is black tissue surrounding the ulcer. This forms because of an absence of healthy blood flow to the area around the ulcer.
Partial or complete gangrene, which refers to tissue death due to infections, can appear around the ulcer. In this case, odorous discharge, pain, and numbness can occur.
Signs of foot ulcers are not always obvious. Sometimes, you wont even show symptoms of ulcers until the ulcer has become infected.
Talk with your doctor if you begin to see any skin discoloration, especially tissue that has turned black, or feel any pain around an area that appears callused or irritated.
Your doctor will likely identify the seriousness of your ulcer on a scale of 0 to 5 using the Wagner Ulcer Classification System:
- 0: no open lesions may have healed lesion
- 1: superficial ulcer without penetration to deeper layers
- 2: deeper ulcer, reaching tendon, bone, or joint capsule
- 3: deeper tissues involved, with abscess, osteomyelitis, or tendonitis
- 4: gangrene in a portion of forefoot or heel
- 5: extensive gangrenous involvement of the entire foot
Ulcers in people with diabetes are most commonly caused by:
- poor circulation
Infection of a foot ulcer can be prevented with:
Zinc To Speed Up The Healing

Zinc-rich foods like eggs, nuts, and legumes can prove to be very beneficial for both your diabetes and diabetic foot ulcers. Zinc promotes the production and secretion of insulin in the body and thus helps to keep blood sugar levels in check. Zinc also hastens the healing of the wound by maintaining the structural integrity of the dermal tissue.
Also Check: Cure For Stomach Ulcer Symptoms
Investigational Compound Regulates Macrophages Is Active
byJeff Minerd, Contributing Writer, MedPage Today September 3, 2021
A topical cream that helps regulate macrophage activity was effective in treating diabetic foot ulcers, a clinical trial reported.
In 236 patients with foot ulcers treated for 16 weeks, the proportion who had complete healing of the ulcer was significantly higher in the group randomized to receive the topical cream versus a comparator group treated with absorbent dressing , said Shun-Cheng Chang, MD, of the Taipei Medical University in Taiwan, and colleagues.
As shown in the team’s study online in JAMA Network Open, the results were similar when the researchers analyzed subgroups of patients with notable risk factors, including those with a glycated hemoglobin level of 9% or higher , those with ulcers bigger than 5 cm2 , and those with an ulcer duration of at least 6 months .
“Topical application of ON101 with gauze immediately after debridement demonstrated significant healing efficacy compared with an absorbent dressing in all patients, including those with DFU -related risk factors,” the researchers wrote. “To our knowledge, this study is the first international phase III randomized clinical trial of an investigational drug able to regulate M1/M2 macrophage activities in patients with DFUs.”
Chang and co-authors explained that the ON101 cream contains two active ingredients shown to regulate macrophage activity and balance:
Disclosures
Finding The Best Treatment For A Diabetic Foot Ulcer
Youre probably wondering if a person who has no history of diabetes is likely to have a foot ulcer and the answer is yes, its possible. Its important to contact a health professional no matter your current health condition as you do not want symptoms to get worse.
The Wound Institute of America is ready to accept new patients who want to have professional wound care from the number one wound care center in California. To make an appointment with Wound Institute of America or to learn more about your foot ulcer, call 919-4179. You can also learn more about foot ulcers and other wound care treatments on our website here.
Don’t Miss: Ulcerative Colitis Shortness Of Breath
How Can A Foot Ulcer Be Prevented
The best way to treat a diabetic foot ulcer is to prevent its development in the first place. Recommended guidelines include seeing a podiatrist on a regular basis. He or she can determine if you are at high risk for developing a foot ulcer and implement strategies for prevention.
You are at high risk if you:
- Have neuropathy
- Wear inappropriate shoes
- Have uncontrolled blood sugar
Reducing additional risk factors, such as smoking, drinking alcohol, high cholesterol, and elevated blood glucose are important in the prevention and treatment of a diabetic foot ulcer. Wearing the appropriate shoes and socks will go a long way in reducing risks. Your podiatric physician can provide guidance in selecting the proper shoes.
Learning how to check your feet is crucial in noticing a potential problem as early as possible. Inspect your feet every dayespecially between the toes and the solefor cuts, bruises, cracks, blisters, redness, ulcers, and any sign of abnormality. Each time you visit a health care provider, remove your shoes and socks so your feet can be examined. Any problems that are discovered should be reported to your podiatrist or a medical professional as soon as possible, no matter how simple it may seem to you.
The key to successful wound healing is regular podiatric medical care to ensure the following gold standard of care:
- Lowering blood sugar
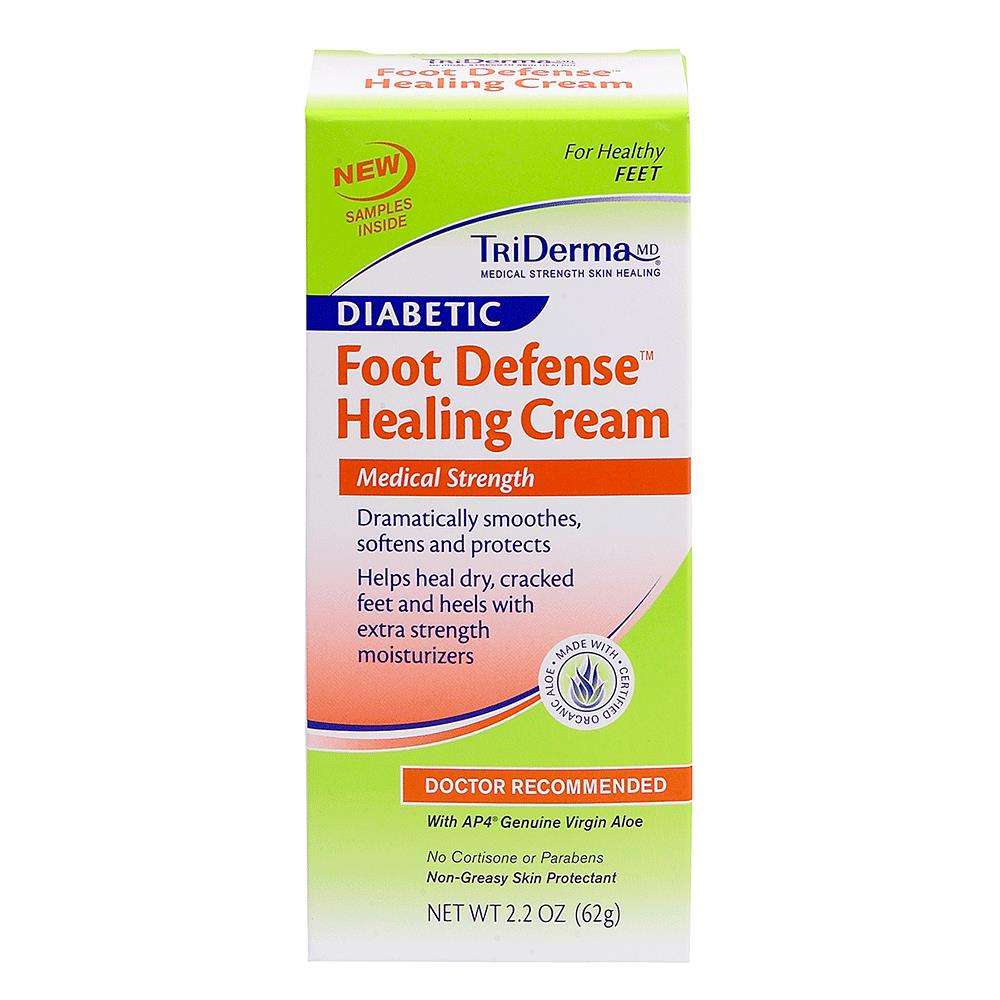
Should Diabetics Use Lotion On Their Feet
The best diabetic foot creams are meant to soothe the achy, itchy, and inflamed feet. Always pay attention to the below points before using any cream or lotion on your feet. If you are not sure you can always ask your doctor.
- Don’t add product on your feet if you have blisters or any injury on your feet
- Inflamed feet will be relieved from pain after a good gentle massage
- Numbness and bad blood circulation are improved after applying the cream for some days
- If you have dry and itchy feet, choose a cream that could cure these symptoms
- Cream for neuropathy will have a different composition and heal that specifically
A great tip is to wear diabetic socks and diabetic shoes after a good massage. Your problems will be solved within no time. It’s all about skincare and proper use.
You May Like: Can Ibuprofen Help Ulcerative Colitis
Find And Treat Cuts Scrapes And Other Wounds Immediately
If you treat new wounds right away, you can start caring for them before things get bad. So as soon as you find a cut or sore:
Of course, if you dont know you have a wound, you cant treat it quickly. So if you suffer from neuropathy, keep an eye out for new wounds. Check your hands and feet daily, and dont forget to check between your toes.
Wearing white socks can help, too. If you see a red spot or a place where your sock is sticking to your skin, check your foot to see if you have a wound thats new or not healing.
Who Gets Foot And Toe Ulcers
Youre at higher risk for foot and toe ulcers if you are:
- Native American.
If you have an eye, kidney or heart disease related to diabetes, youre also at a higher risk. About 15% of people with diabetes will get an ulcer, typically on the bottom of their foot. Around 6% of that 15% will have to be hospitalized because of complications.
Youre also at a higher risk of getting foot and toe ulcers if you have any of the following:
- Problems with circulation.
Recommended Reading: Best Cure For Mouth Ulcers
How Do I Take Care Of My Foot And Toe Ulcers
Your healthcare provider might teach you how to care for your ulcers at home. You might be instructed to:
- Wash the affected area with mild soap.
- Keep the wound clean and dry.
- Change the bandages as directed.
- Take prescribed medications as directed.
- Drink plenty of fluids. Ask your healthcare provider how much water you should drink every day.
- Follow a healthy diet, as recommended by your healthcare provider.
- Exercise regularly, under your healthcare providers care.
- Wear appropriate shoes.
- Wear compression wraps as directed.
Contact Our Dfw Wound Care Doctor For A Consultation Today
Diabetic foot ulcers can be easily treated if caught early. If you are diabetic and are experiencing signs of a foot ulcer and need treatment, contact our DFW wound care doctor at Alliance Foot & Ankle Specialists for help. To request an appointment in our Grapevine or Keller office, fill out our convenient online contact form, or call our office today.
|
Related links: |
Read Also: Is Beer Bad For Ulcerative Colitis
What Causes Diabetic Foot Ulcers
- Blood glucose levels
- And the length of time you have had diabetes
If youve been struggling with diabetes for many years, you are more likely to develop neuropathy, which is reduced feeling in the feet due to nerve damage. This nerve damage can occur slowly over time due to high blood glucose levels, and because it is often painless, you might not even be aware of the problem.
Unfortunately, you might also not be aware of foot ulcers.
If you cant feel DFUs, then you probably arent doing anything to help them heal. And, diabetic wound healing can be very complicated and slow if you dont help it along.
Which Ointment Is Best For Diabetic Wound
Hydrogen peroxide is used for very small wounds, but itâs more important to prevent infection when treating diabetic wounds. For a closed incision or wound, you would want to cover the entire surface of the skin with dry non-stick dressing and secure it with adhesive tape.
For an open wound or ulcer, itâs important to cleanse using soap and water as well as to irrigate your wound twice per day in order to maintain a sanitary environment. Wet dressings may be recommended after cleaning which may include sterile gauze/adhesive tapes applied so that the material can absorb any fluids from the surrounding area.
Newer products such as hydrocolloid dressings which are able to create a moist healing environment on surfaces by absorbing wound fluid while protecting the area from infection, dirt, and other external contaminants are available over-the-counter at pharmacies or grocery stores.
If you have a non-healing ulcer after six months of treatment, consult your doctor for further help in promoting wound healing. They may prescribe antibiotics to prevent infections.
Here is a list of supplies required when treating sores on diabetics:
- Hydrogen peroxide
Read Also: What Is A Gastric Ulcer And What Is Its Cause
Also Check: Alternatives To Humira For Ulcerative Colitis
History Of Previous Ulceration And Amputation
A diabetic patient with a history of previous ulceration or amputation is at increased risk for further ulceration, infection and subsequent amputation. Alterations in foot dynamics due to ulceration, joint deformity or amputation can cause the abnormal distribution of plantar pressures and result in the formation of new ulcers28.
Locilex: Clinical Study Results
Pexiganan acetate has been found to have a broad spectrum of antimicrobial activity against many gram-positive and gram-negative aerobic and anaerobic bacteria and certain species of fungi.
In vitro, 91% of aerobic strains of bacteria were susceptible to pexiganan, similar to the 91% for ofloxacin and 92% for ciprofloxacin. Only enterococci required the highest concentrations of pexiganan for eradication. Of the anerobes tested, 97% were susceptible to pexiganan. Thirty percent of candida isolates were inhibited by the drug.
In vivo studies have shown a 5-log reduction in the numbers of Pseudomonas aeruginosa in swine skin wounds and a 4-log reduction in perineal skin flora on human skin following topical application. Several large-scale clinical studies have been completed evaluating the drug in the treatment of infected diabetic foot ulcers. These were designed to compare the efficacy of pexiganan to that of the fluoroquinolone ofloxacin, which is recognized as being a standard of antibiotic therapy for infected diabetic ulcers.
Also Check: Children’s Mouth Ulcers Treatment
Impaired Angiogenesis In Diabetes Due To Epc Dysfunction
It is known that EPCs are decreased in number and dysfunctional in people suffering from diabetes mellitus. The decrease in number of circulating EPCs in people with diabetes is still under investigation but defects in the SDF-1/CXCR-4 pathway are becoming evident. There are defects in EPC recruitment to wound sites. This is due to decreased mobilisation from the bone marrow and decreased homing to cutaneous wounds. With diabetes there is decreased EPC participation in neoangiogenesis and neovsacularisation. Studies show that there are defects in cell migration, adhesion and tube formation. There is also an increase in reactive oxygen species in EPCs isolated from diabetes patients leading to cellular dysfunction. There is a body of evidence indicating that diabetes mellitus related EPC cell dysfunction represents a mechanism for impaired angiogenesis and impaired wound healing seen in diabetic patients. The obstacle with autologus EPC therapy for diabetic complications is that there is a decreased number of cells available for transplantation. In addition, these autologous cells are dysfunctional.
How Are Foot And Toe Ulcers Diagnosed
Your healthcare provider can tell what type of ulcer you have based on four observations:
- The appearance of the ulcer.
- Location of the ulcer.
- The appearance of the borders.
- The appearance of the surrounding skin.
Your primary healthcare provider can diagnose an ulcer, but they might send you to a specialist for treatment. You might see a podiatrist, a provider who works with feet, or a wound specialist. For more complicated cases that require surgery, you might also see a plastic surgeon, anesthesiologist, orthopedic surgeon and/or vascular surgeon.
Also Check: Foods To Avoid With Ulcerative Proctitis
The Initial Causes Ointment For Diabetic Foot Ulcers
Type 2 diabetes is a common condition in many people. This type is caused by a lack of insulin and is a result of an unhealthy lifestyle. The bodys inability to process glucose from the blood can damage many parts of the body, including the eyes, kidneys, and nerves. Fortunately, there are some things you can do to avoid diabetes. Here are five tips to help you lower your risk: Eat more vegetables and fruits, get regular exercise, and avoid smoking.
High levels of triglycerides in the blood are another factor that can cause diabetes. These triglycerides are caused by a buildup of cholesterol in the blood. A high triglyceride level causes the body to misrepresent insulin as a molecule, which causes glucose to build up in the blood. A simple blood glucose test can confirm your diagnosis of type 2 diabetes. By following these tips, you can begin living a healthy life and avoid the complications of diabetes.
A person with type 2 diabetes must consume less sugar. Glucose causes thirst and dehydration because the body releases energy stores into the bloodstream instead of using insulin. If untreated, diabetes can lead to weight loss and diabetic ketoacidosis, a dangerous condition whereby the cells are deprived of energy. To prevent the condition, you must make sure that your diet is low in glycemic load and that you exercise regularly.
How The Intervention Might Work

For millennia healers have applied various compounds to infected wounds, some of which are still in use today. Use of a topical application has many potential advantages compared with giving systemic antibiotic therapy, including: a high and sustained concentration of the antimicrobial agent at the site of infection the need to use only a limited amount of the antimicrobial at the selected site avoidance of potential toxicity associated with systemic treatment ability to use novel agents not available for systemic use easy application in the outpatient setting and potentially better patient adherence to treatment. Topical treatments may also prove helpful in addressing the globally increasing problem of multidrugresistant organisms that are now untreatable with most systemic agents. For example, a study of 47 organisms from burn wounds that were multidrugresistant to systemic antibiotics were susceptible to 11 commonly used topical antibiotics and antiseptics, although the rates of resistance were higher than in nonmultidrugresistant organisms .
Read Also: How To Treat Sacral Pressure Ulcer
You May Like: How To Treat An Eye Ulcer