For Ulcers Caused By Varicose Veins
A UK multi-centre randomised controlled trial, EVRA, found that For patients with leg ulcers caused by varicose veins, early interventionA treatment, procedure or programme of health care that has the potential to change the course of events of a healthcare condition. Examples include a drug, surgery, exercise or counselling. to treat the veins results in faster healing of ulcers than standard compression therapy alone . It also increases ulcer-free time and is highly likely to be cost-effective.
What Is The Best Treatment For Venous Ulcers
What is the recommended procedure for treating leg ulcers?
It depends on the cause. If the ulcers are due to varicose veins, then treatment of the varicosities can help significantly in conjunction with a wound care specialist. If due to deep venous reflux, compression stockings and wound care are the best choices.
It depends on the cause. If the ulcers are due to varicose veins, then treatment of the varicosities can help significantly in conjunction with a wound care specialist. If due to deep venous reflux, compression stockings and wound care are the best choices.
Correct any superficial venous reflux.
Correct any superficial venous reflux.
Venous stasis ulcers can be due to deep, superficial, and/ or perforatorvein incompetence deep vein thrombosis can also be involved in theetiology. Before recommending the best treatment, venous duplex scanning must be performed and acomprehensive history and physical must be taken by an expert in the field of complex venous disorders. Perforator vein surgery , superficial venous ablation, vein interruptions, or a combination of these treatments may be indicated.
The best treatment for venous ulcers consists of 2 parts, both applied assoon as possible. First, the underlying cause should be identified andtreated. Second, proper compression with edema reduction and specializedwound care is needed until the ulcer heals.
Topical Antimicrobials And Antiseptics
In chronic wounds, reduction of certain microbial species, such as anaerobic bacteria in order to limit undesirable odors or perhaps mixed communities of four or more bacterial species that impede healing, use of topical antibiotics may be justified .
Various studies on dressings incorporating antibiotics and antiseptics are reviewed, but no single consensus for any particular topical agent could be made. This is partly due to the different mechanism and spectrum of action of the antimicrobials. The most frequently used topical antimicrobials in wound care practice are chlorhexidine, iodine, silver containing products, mupriocin and fucidic acid. In the past, acetic acid, honey, hydrogen peroxide, sodium hypochlorite, potassium permanganate, and proflavine have been used.
Read Also: How To Treat A Diabetic Foot Ulcer On The Sole
Where Should Care Be Carried Out
Patients with venous leg ulcers are best managed in the community for two reasons:
-
Maintenance of independence and mobility is important in this elderly population
-
The number of patients would overwhelm hospital services.,
However, direct access to appropriate specialised hospital services is essential for the investigation of underlying vascular disease and for microbiology, histopathology, and dermatology. Having said that, leg ulcer services provided in hospitals often fail to appreciate how many patients with leg ulcers simply refuse to come to hospital, let alone consent to venous investigation or surgery., Few community patients are prepared to be referred for assessment of their underlying venous disease.,,
Rates of healing have been shown to be improved and costs to be reduced when a coordinated service using research based protocols was introduced.,,, Responsibility for patient care should not be removed from community nurses they should be provided with resources and training aimed at delivering an appropriate, high quality service in specialist leg ulcer clinics. Evidence from our own research in two large health authorities in the United Kingdom showed that standards could be maintained only with close supervision when a leg ulcer service was continued without the direct involvement of a leg ulcer nurse specialist, healing rates declined and costs increased.
Description Of The Condition
Venous leg ulcers are common and recurring complex wounds that heal by secondary intention . Problems with the leg veins reduce the efficient return of blood to the heart and increase the pressure in the veins , which may result in venous leg ulcers. The precise chain of events that links high venous pressures with skin breakdown and a chronic wound is not fully understood .
Venous leg ulcers commonly occur on the gaiter region of the lower leg . A venous leg ulcer is defined as any break in the skin that has either been present for longer than six weeks or occurs in a person with a history of venous leg ulceration. Differential diagnosis of the type of leg ulcer is made by taking a clinical history, physical examination, laboratory tests and haemodynamic assessment . True venous ulcers are moist, shallow and irregularly shaped and lie wholly or partly within the gaiter area of the leg. Leg ulcers can be associated with venous disease in combination with vascular disease, which impairs arterial blood supply in these instances they are said to have a ‘mixed’ aetiology . Open skin ulceration due solely to limb ischaemia from vascular disease is less common.
Recommended Reading: Does Tylenol Cause Stomach Ulcers
How Can These Ulcers Be Prevented
Once an ulcer has developed, statistics show that another one will develop within 3-5 years. You know that preventing ulcers is well worth the effort if you have experienced the pain and frustration associated with healing wounds. Many patients will continue to wear some type of compression stocking every day while they are on their feet to help the circulation. While a Venous Stasis ulcer may have healed the poor circulation which caused the ulcer has not been corrected. Use AMERIGEL Care Lotion on your lower legs, particularly around the ankles daily. This helps the skin retain its natural moisture, promoting healthier skin that is less prone to problems.
AMERX Health Care Corporation164 Douglas Rd E, Oldsmar, FL 34677 | 448-9599 | AMERXHC.com
AMERX®, AMERIGEL®, HELIX3®, EXTREMIT-EASE®, Where Compression Meets Compliance®, Turn-Key DME®, and Oakin®, are registered trademarks of AMERX Health Care Corporation.
AMERX®, AMERIGEL®, HELIX3®, EXTREMIT-EASE®, Where Compression Meets Compliance®, Turn-Key DME®, and Oakin®, are registered trademarks of AMERX Health Care Corporation.
Who Gets Stasis Ulcers
Stasis ulcers affect 1% of the population, so they are not uncommon. A variety of medical problems and lifestyle factors have been linked to their development. These include:
- Standing upright for long periods
- Multiple previous pregnancies
Stasis ulcers account for at least 4050% of chronic lower limb ulcers and contribute to a further 20% of mixed arterial and venous ulcers.
Don’t Miss: Ulcer In My Stomach Symptoms
Which Wound Dressing Is Best For Your Pressure Ulcer
Now that weve touched on some of the more common types of dressings used for pressure ulcers, you may be wondering which is the best for your particular situation. The answer will depend on multiple factors including where the pressure ulcer is located, how severe the bedsore is, and the degree of skin and tissue damage. Talk to your health care professional about any pressure wounds you notice on your body as soon as possible.
Treatment Options For Venous Stasis Ulcers
At first, venous ulcers are generally shallow and irregularly shaped. As the deterioration of the affected tissue progresses, the ulcer can extend deeper into the underlying tissues, involving the tendons, ligaments, and bone. The goal of venous ulcer treatment is to minimize edema, control infection, heal the wound, and prevent reoccurrence. Many leg ulcer patients experience alternating periods of healed and open ulcerations. Those with venous stasis ulcer commonly find the skin lesions will return unless the underlying cause is corrected.
To effectively treat venous stasis ulcers, doctors commonly evaluate the venous and arterial circulation in the affected area to identify the underlying cause. Once the cause is determined, physicians are in a better position to develop a successful plan of action. Doctors treating venous ulcers may recommend one or more of the following options:
Recommended Reading: Vulvar Ulcers Not Std Pictures
Also Check: Ulcerative Colitis And Colon Cancer Statistics
Venous Leg Ulcers: 6 Things To Know When Treating Venous Disease
Lower extremity venous disease affects millions of Americans and may ultimately lead to open, draining wounds that adversely affect quality of life. However, there are exciting developments in early diagnosis, prevention and treatment of venous leg ulcers . On the treatment side, there are more choices now than ever before in compression products, which is greatly improving the patient experience. But proper treatment also comes from a better understanding of venous leg ulcers, and better understanding comes from more education. Luckily, were here to help provide education and support for you and your team, so here are six things to know when treating VLUs.
You May Like: Can Ulcers In The Colon Be Cancerous
Diabetes And Leg Wounds
Although diabetic leg ulcers and peripheral vascular disease wounds are different, they may share some of the same causes and risk factors. According to Science Directs study, It is reported that diabetes is associated with a two to four-fold increase in the incidence of peripheral arterial disease compared to non-diabetic subjects.
Diabetes and PAD go hand-in-hand because the lining in your blood vessels becomes less flexible allowing plaque to build up even easier. When blood isnt able to move freely, blockages tend to occur. Not only does diabetes irritate and inflame the lining of your blood vessels, but it can also compromise your ability to fight infections which could cause open wounds to not heal properly.
Lastly, high blood pressure, increased cholesterol levels, family history of vascular disease, and diabetes are all linked as causal factors for peripheral vascular disease wounds. That said, if youre at an increased risk, you should be monitoring any slow-healing wounds or diabetic leg ulcers so you can notify your doctor.
You May Like: Icd 10 Stage 4 Sacral Ulcer
Recommended Reading: Can You Cure Ulcerative Colitis Naturally
How The Intervention Might Work
Animal experiments conducted over 40 years ago suggested that acute wounds heal more quickly when their surfaces are kept moist rather than left to dry and scab . A moist environment is thought to provide optimal conditions for the cells involved in the healing process with faster revascularisation , and development of granulation tissue , as well as allowing autolytic debridement , which is thought to be an important part of the healing pathway .
The desire to maintain a moist wound environment is a key driver for the use of wound dressings and related topical agents. Whilst a moist environment at the wound site has been shown to aid the rate of epithelialisation in superficial wounds, excess moisture at the wound site can cause maceration of the surrounding skin , and it has also been suggested that dressings that permit fluid to accumulate might predispose wounds to infection . Wound treatments vary in their level of absorbency, so that a very wet wound can be treated with an absorbent dressing to draw excess moisture away and avoid skin damage, whilst a drier wound can be treated with a more occlusive dressing or a hydrogel to maintain a moist environment.
Some dressings are now also formulated with an ‘active’ ingredient .
Polyacrylate Moist Wound And Debridement Dressings
This activated absorbent polyacrylate polymer core dressing absorbs large protein molecules while irrigating with Ringers solution, a physiological fluid, creating a rinsing effect . The interactive dressing supports both moist wound healing and autolytic debridement, gently removing dead tissue from the wound bed while creating an ideal healing environment. Polyacrylates debride at a mean rate of 38%.34 Research has shown that polyacrylate gel absorbents debride just as well as collagenase does.36 Recent research has also shown that the product may be effective in reducing wound bioburden by interfering with biofilm as well as absorbing planktonic or free-floating bacteria.35
Recommended Reading: Can Ulcers In The Esophagus Cause Cancer
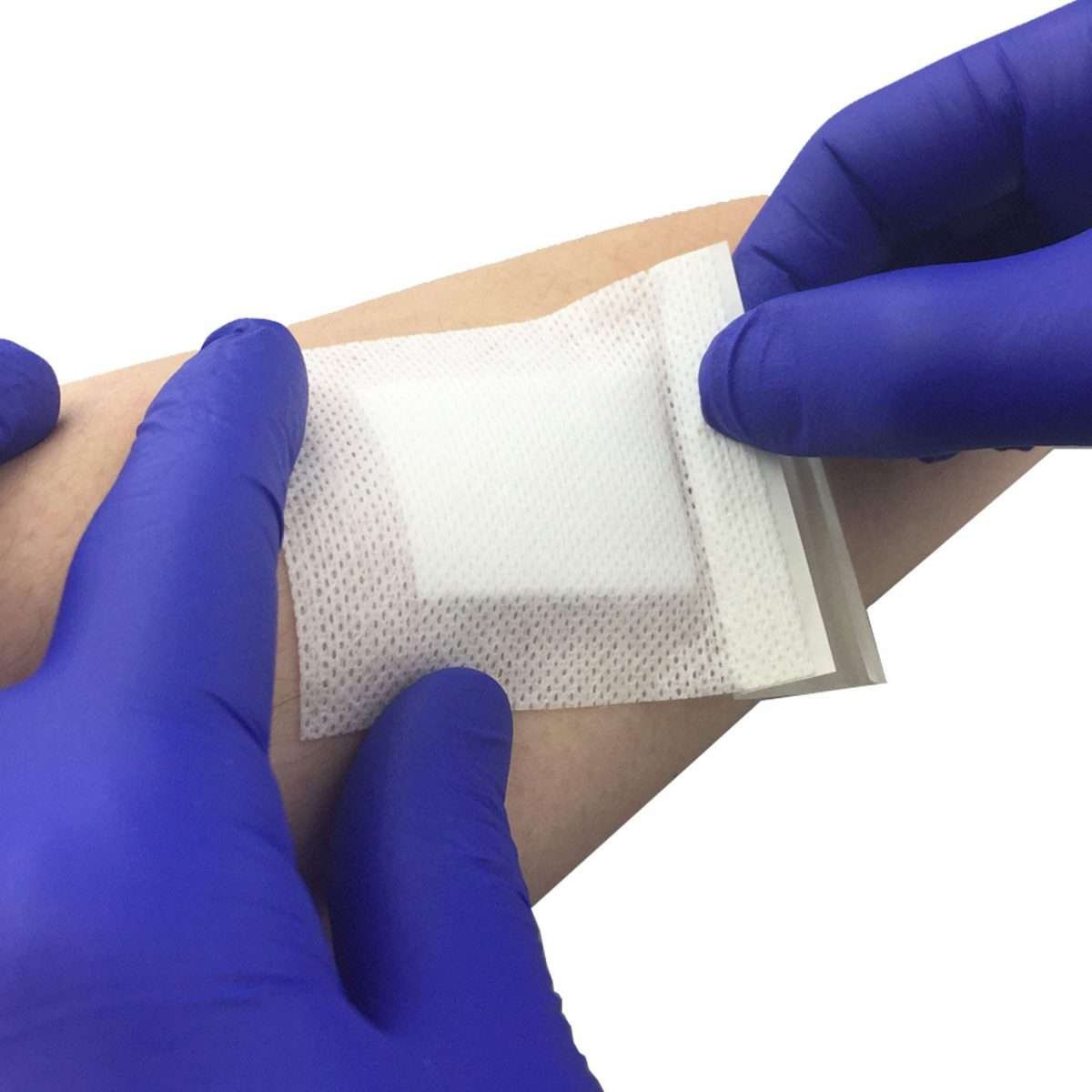
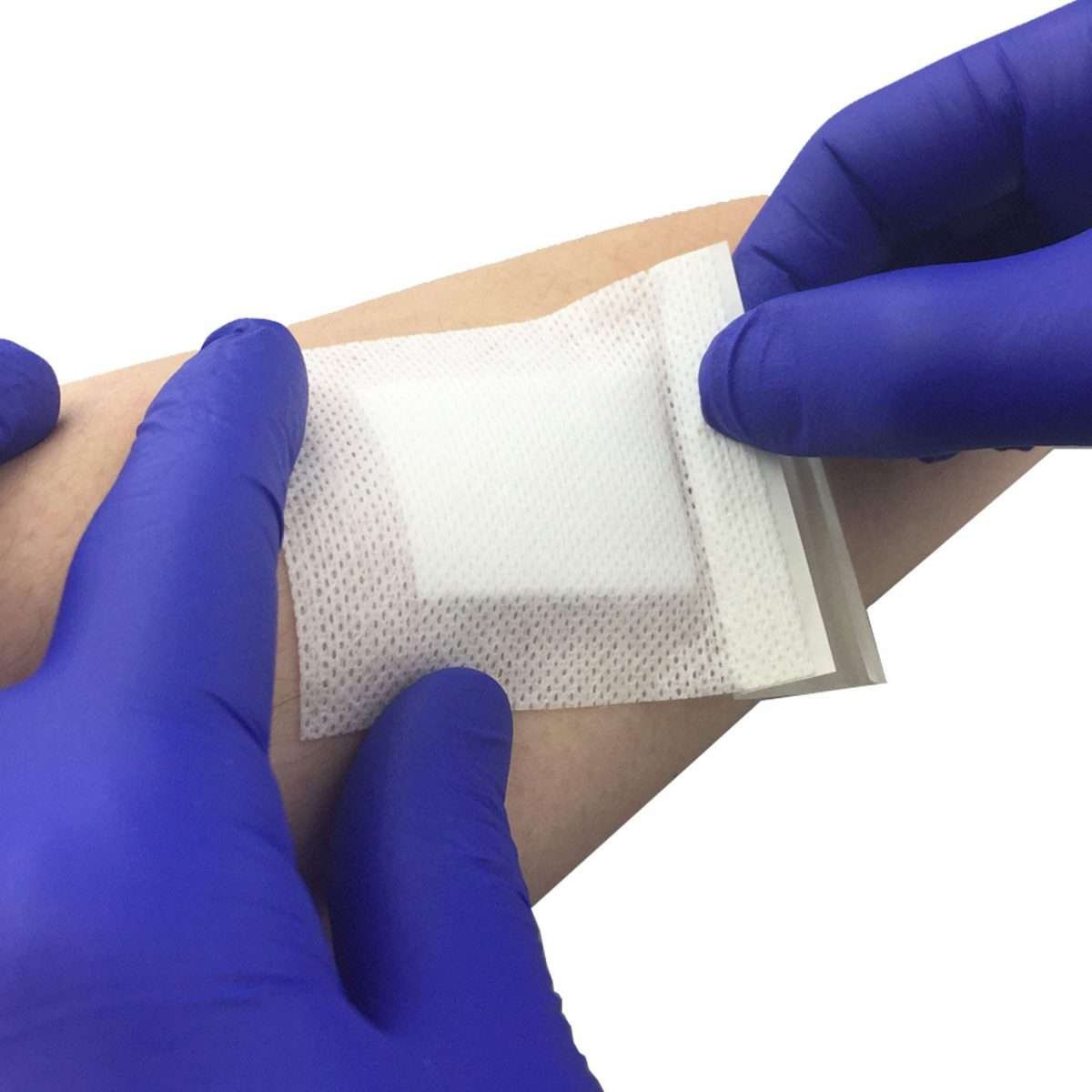
Proper Foam Dressing Application Instructions
The procedure for applying a foam dressing is as follows:
The flexibility of foam dressings allows for a wide variety of clinical applications with wounds that have from moderate to heavy exudate. Because they are easy to use and can be easily cut to fit irregular wound areas, they are a good dressing choice for many situations.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of IncontinenceSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
What Causes Sacral Pressure Ulcers
Pressure ulcers occur when there is prolonged pressure to the skin, usually over bony areas such as the elbows, spine, or sacral area .
Compression of the soft tissue causes blood vessels to collapse and reduces blood flow and oxygen delivery. This localized tissue damage usually happens when a person sits or lays for long periods of time in a chair, wheelchair, or bed.
Pressure ulcers begin forming under the skin, making them difficult to catch before a wound is actually visible. So its important to take these steps to help prevent sacral pressure ulcers from happening.
Also Check: Ulcer Pain Relief At Night
Caring For Venous Ulcers
Venous ulcers need proper care and treatment to prevent infection and to heal. Its important to have any venous ulcers checked right away by your healthcare provider.
Treatment may require focusing on the circulatory or vein problems that are causing the ulcers. Or it may mean removing some tissue around the wound. You may be asked to:
-
Clean the wound regularly
-
Apply a dressing to the ulcer
-
Avoid products that cause skin sensitivity
-
Wear compression stockings to prevent blood from pooling in the legs and to speed healing
-
Apply an antibacterial ointment or another topical medicine to prevent or treat an infection
-
Take oral antibiotic medicines to prevent or treat an infection
-
Have allergy testing done
Wearing a compression wrap to keep blood flowing back up to your heart can also help ulcers heal more quickly. In some cases, surgery or a skin graft is needed to close up the opening in the skin.
Description Of The Intervention
The review includes all dressings and topical agents applied directly onto or into wounds and left in situ. This contrasts with products used to irrigate, wash or cleanse wounds and that are only in contact with wounds for a short period. Firstline treatment for venous leg ulcers is compression therapy in the form of bandages, stockings or mechanical devices . This application of external pressure around the lower leg assists venous return and reduces venous reflux . We therefore anticipated that wound dressings would commonly be used in combination with compression therapy.
Dressings are widely used in wound care with the aim of protecting the wound and promoting healing by influencing the local wound environment , typically by physical means, such as thermal insulation, absorption of exudate and physical protection. Dressings may also have pharmacological, immunological or metabolic actions. Topical agents include hydrogel gels, ointments and creams that are placed in contact with the wound and left in situ.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
Capillaryaction dressings consist of an absorbent core of hydrophilic fibres held between two lowadherent contact layers. Examples include: Advadraw and Vacutex .
Topical agents
Read Also: How Many People Have Ulcerative Colitis
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the âcontrolâ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
What Does Venous Stasis Ulcer Look Like
The venous stasis ulcer is a deep red, firm, and round ulcer that can easily form on the surface of the veins. It typically affects the legs, but can also appear on the arms and neck. The ulcer can be accompanied by intense pain and swelling, and it can be difficult to treat. If left untreated, the venous stasis ulcer can lead to serious health complications.
Recommended Reading: Ulcer And High Blood Pressure
What Does A Venous Leg Ulcer Look Like And What Causes Them
Venous leg ulcers are sores that develop between your knee and ankle, but they typically form inside the leg near or around the ankle. They are large, shallow ulcers with uneven edges that drain or weep a lot.
Youll likely see swelling in your leg, with red, itchy skin around the wound. You may also experience tightness in your calves, as well as aching, throbbing or a feeling of heaviness in your legs. Pooled and trapped blood often causes discolored splotches in the area.
The sores sometimes affect only the skin or they may sink deeper into the fat layer, muscle, tendon and bone, she says. Severe ulcers are more likely to become infected and take longer to heal.
Your veins carry blood back to your heart, and valves in the veins stop the blood from flowing backward. When your veins have trouble sending blood from your limbs to the heart, its known as venous insufficiency. In this condition, blood doesnt flow back properly to the heart, causing blood to pool in the veins in your legs.
Our veins are just like pipes, says Ehren. When theres persistently high blood pressure in the veins of the legs with a valve that doesnt work correctly, it causes damage to the skin, which eventually breaks down and forms an ulcer.
Other possible causes for venous leg ulcers include:
- Varicose veins.
- Swelling of a superficial vein .