Data Collection And Analysis
Two review authors independently performed study selection, risk of bias assessment and data extraction. We conducted network metaanalysis using frequentist megaregression methods for the efficacy outcome, probability of complete healing. We modelled the relative effectiveness of any two treatments as a function of each treatment relative to the reference treatment . We assumed that treatment effects were similar within dressings classes . We present estimates of effect with their 95% confidence intervals for individual treatments compared with every other, and we report ranking probabilities for each intervention . We assessed the certainty of the body of evidence using GRADE for each network comparison and for the network as whole.
Assessing Sacral Pressure Ulcers
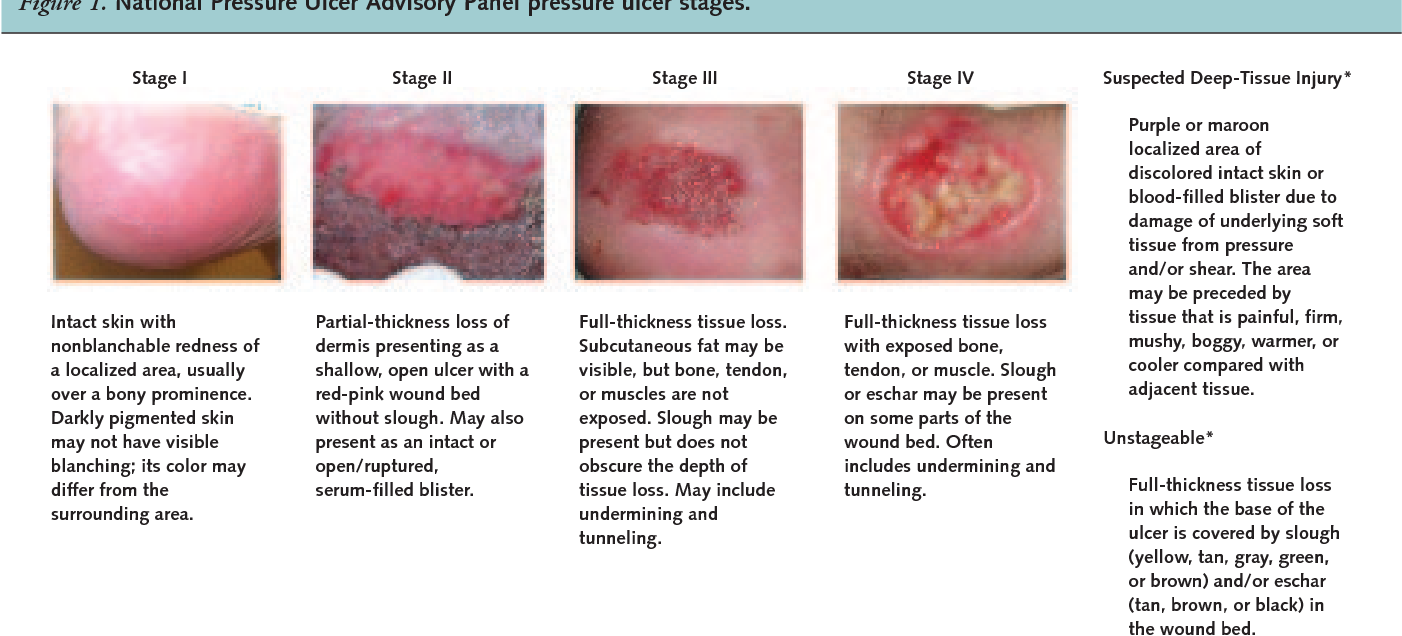
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Symptoms Of Pressure Sores
Pressure sores go through 4 stages.
- Stage 1. During this stage, the area of the sore looks red. It may feel warm to the touch. It may burn, hurt, or itch. The pressure sore may look blue or purple in people who have dark skin.
- Stage 2. During this stage, the area is more damaged. The sore may be open. It may look like a cut or blister. The skin around the sore may be discolored. The sore is painful.
- Stage 3. During this stage, the sore will have a crater-like look. This is due to increased damage below the surface. This makes the wound deeper.
- Stage 4. This is the most serious stage. Skin and tissue are severely damaged. The sore becomes a large wound. Infection is possible. Youre likely able to see muscle, bones, tendons, and joints.
Infected pressure sores take a long time to heal. Also, the infection can spread to the rest of your body. Signs of infection at the site include:
- Thick, yellow, or green pus
- A bad smell coming from the sore
- Redness or skin that is warm to the touch
- Swelling around the sore
Signs that the infection has spread include:
Also Check: What To Eat If You Have Peptic Ulcer
Also Check: Medical Card For Ulcerative Colitis
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
How Can I Tell If I Have A Pressure Sore
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
Also Check: How Do You Diagnose An Ulcer
Description Of The Condition
Pressure ulcers, also known as pressure injuries, bedsores, decubitus ulcers or pressure sores, are localised areas of injury to the skin, the underlying tissue or both. They often occur over bony prominences such as the sacrum and heel , and are caused by external forces such as pressure, or shear, or a combination of both .
Risk factors for pressure ulcer development have been summarised into three main categories: a lack of mobility poor perfusion and low skin status the latter category includes the presence of stage 1 pressure ulcers or incontinence or both, which also increases the risk of ulceration by producing a detrimental environment for the skin .
Prevalence
Pressure ulcers are one of the most common types of complex wound. Prevalence estimates differ according to the type of population assessed, the data collection methods used and period of data collection and whether Stage 1 ulcers were included).
One large European study estimated a hospital pressure ulcer prevalence of 10.5% whilst a US study estimated a prevalence of 9.0% across acutecare, longterm care and rehabilitation settings ). In the UK, national pressure ulcer data are collected across community and acute settings as part of the National Health Service Safety Thermometer initiative . About 4.4% of patients across these settings were estimated to have a pressure ulcer in November 2014 .
Treatments for pressure ulcers
Impact of pressure ulcers on patients and financial costs
How Can You Tell If You Have A Pressure Sore
Sometimes, a pressure ulcer can be difficult to identify, especially in the early stages. Here is some information about the symptoms and signs that may indicate that you have a stage 1 pressure ulcer.
- Discolored, reddened, or darkened skin is one of the first signs of a pressure ulcer. For individuals with darker skin, purple, bluish, and shiny areas are one of the first signs. The area may feel warm or hard.
- If you remove pressure from the afflicted area for 30 minutes and the skin does not go back to normal, a pressure ulcer has begun to form.
- Press on the afflicted area with your finger to do the blanching test. Once the area goes white, you should remove the pressure. If the area remains white, this means blood flow has been impaired. The blanching test may not be as effective when it comes to dark skin.
Recommended Reading: Treating Hindgut Ulcers In Horses
How To Care For A Pressure Ulcer
Pressure Ulcer is a common occurrence among patients who are bed-bound or immobile. If you are a caregiver caring for a loved one who has pressure ulcers, you might want find out how you can manage the pressure ulcer wound and prevent it from deteriorating. Prevention is the key to ensure that your loved one does not develop another pressure ulcer wound. Read on to find out how to care for your loved ones wound properly and how you can get a change of wound dressing in the comfort of your home.
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Also Check: Can Ulcerative Colitis Go Into Remission
Overall Completeness And Applicability Of Evidence
The network is sparse, in terms of the total number of participants, the total number of wounds healed, the number of studies per contrast, the size of the constituent studies and the duration of followup: 21 of 27 direct contrasts were informed by only one study and the average number of events per mixed treatment contrast was around four. The median study size was 41 and several studies had zero events. The duration of followup was relatively short for most studies : only 3/39 studies in the network had a followup duration of 16 weeks or more.
In parallel we conducted a second NMA, grouping together some classes of dressings. We had hoped that the group network would provide more power in the analysis, but in practice too many data were excluded from the network, and the network was also unbalanced, being dominated by the advanced dressing versus basic dressing contrast, which involved about 55% of the participants in the group network. The group network provided equally uncertain evidence and the findings are not discussed further here, but are reported in Appendix 5 for the interested reader.
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
Also Check: Probiotics Good For Ulcerative Colitis
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
-
the Cochrane Wounds Specialised Register
-
the Cochrane Central Register of Controlled Trials
-
Ovid MEDILINE
Searching other resources
Diagnosing A Stage 4 Bedsore
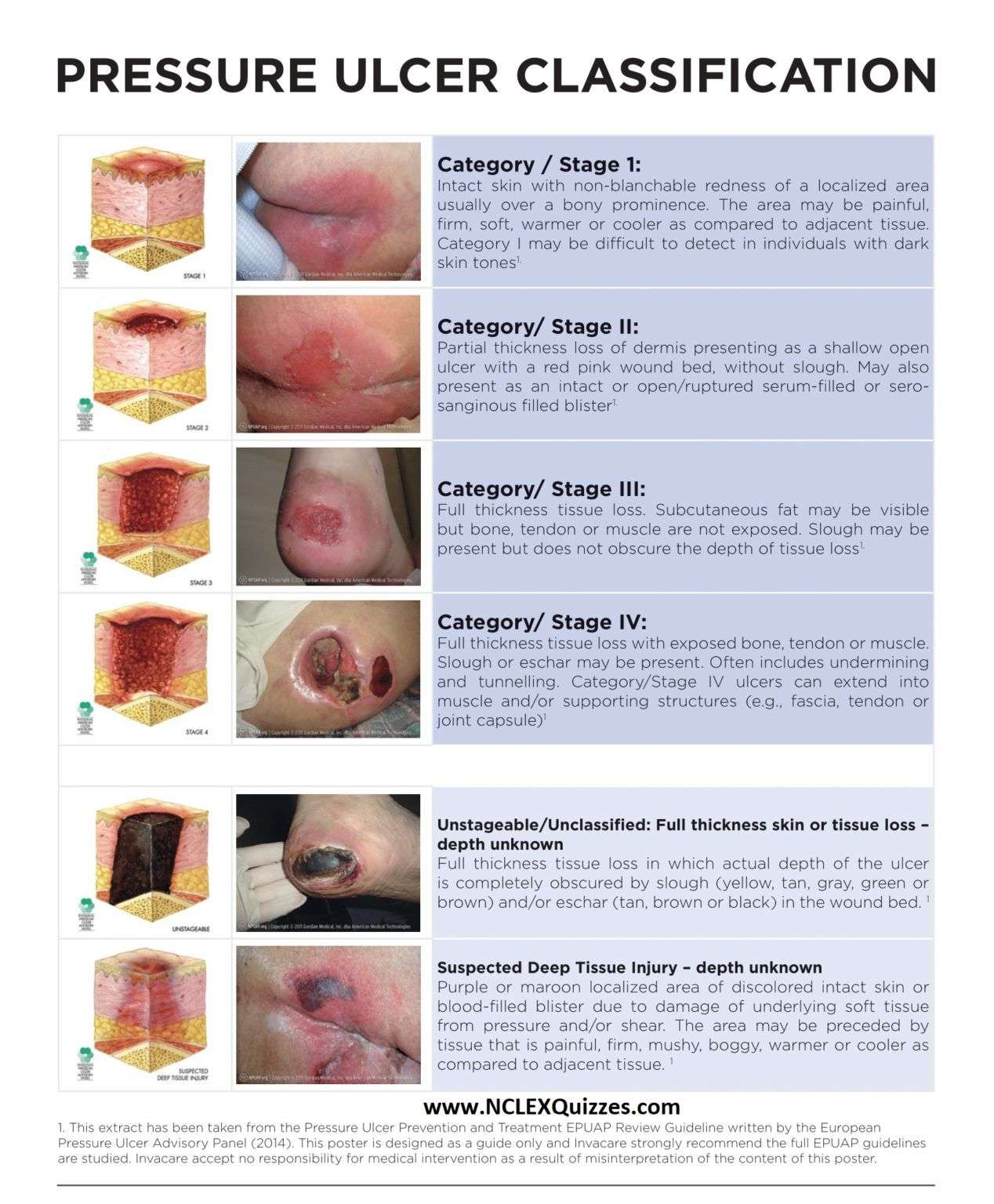
A doctor determines the by its appearance. In the case of a stage 4 bedsore, the large wound has passed the bodys fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury This diagnosis happens when the surface of a patients skin looks like a stage 1 or 2 sore, but it is actually affecting deeper tissues underneath.
Also Check: Can Ulcerative Proctitis Be Cured
Don’t Miss: Ulcerative Colitis How Much Blood Is Too Much
Posthoc Sensitivity Analysis Dressings Only
For the individual network, we also investigated, posthoc, our original assumption that topical agents could be used in place of dressings, by examining only the network of studies involving two or more dressings . There were no threearm trials remaining and the 30 studies compared 12 interventions in a total of 1627 participants experiencing 641 events, with 16 direct contrasts and 66 mixed treatment contrasts. The NMA rankings were similarly imprecise .
For the group network, 17 studies compared five interventions in a total of 798 participants experiencing 304 events, with five direct contrasts and 10 mixed treatment contrasts. This network was still sparse in terms of total participants, but, on average, there were more events per contrast. The posthoc sensitivity analysis had less overlap of rankograms than the full group network, and the mean rank was closer to a whole number one SUCRA value was 0 and another was 0.9. The mean ranks were: proteasemodulating 1.4 advanced 1.9 basic 3.1 antimicrobial 3.7: advancedantimicrobial 4.9. For the comparisons with basic dressing, effect estimates were similar to those in Table 4 but CIs were still wide.
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Recommended Reading: Bone Broth And Ulcerative Colitis
You May Like: Ozanimod Phase 2 Ulcerative Colitis
Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
Causes Of Pressure Ulcers
Pressure ulcers are caused by sustained pressure being placed on a particular part of the body.
This pressure interrupts the blood supply to the affected area of skin. Blood contains oxygen and other nutrients that are needed to help keep tissue healthy. Without a constant blood supply, tissue is damaged and will eventually die.
The lack of blood supply also means that the skin no longer receives infection-fighting white blood cells. Once an ulcer has developed, it can become infected by bacteria.
People with normal mobility do not develop pressure ulcers, as their body automatically makes hundreds of regular movements that prevent pressure building up on any part of their body.
For example, you may think that you are lying still when asleep, but you may shift position up to 20 times a night.
Pressure ulcers can be caused by:
- pressure from a hard surface such as a bed or wheelchair
- pressure that is placed on the skin through involuntary muscle movements such as muscle spasms
- moisture which can break down the outer layer of the skin
The time it takes for a pressure ulcer to form will depend on:
- the amount of pressure
- how vulnerable a person’s skin is to damage
Grade 3 or 4 pressure ulcers can develop quickly. For example, in susceptible people, a full-thickness pressure ulcer can sometimes develop in just 1 or 2 hours. However, in some cases, the damage will only become apparent a few days after the injury has occurred.
Recommended Reading: Does Ulcerative Colitis Cause Back Pain