Surgery In Inflammatory Bowel Disease
Generally the symptoms of Crohns disease can be managed with medicines. The medicines all aim in turning off different parts of the immune system. Medical therapy is the most important aspect of the treatment of Crohns disease. At times, surgery is required. You may develop an infection and an abscess where the intestinal fluid or food cant pass readily. You may have bloating and distention of your abdomen because of this and surgery is required to address these issues. Surgery is usually the last recourse for these patients and timing is critical. Colorectal surgeons work closely with gastroenterologists and medical teams to help you feel better. When surgery is required, it brings tremendous benefits and improvements in your quality-of-life.
Is Colitis Caused By Stress
Although stress can be responsible for triggering a flare-up of symptoms, stress is currently not thought to cause ulcerative colitis. Instead, researchers think stress exacerbates it. The exact cause of ulcerative colitis is unknown, but some people have a greater risk for developing this condition.
Ulcerative Colitis Surgery Cost
As surgery for ulcerative colitis requires at least one and possibly three hospital stays, it comes at a higher cost than procedures that can be done as outpatient surgery. Ileostomy surgery may cost approximately $39,000, while j-pouch surgery may cost $50,000.
Check with your insurance provider to find out how much will be covered and what co-pays may be required. Using a hospital and surgical team in your plan’s network is key to preventing any unexpected charges.
Also Check: Acute Exacerbation Ulcerative Colitis Symptoms
Can Colitis Cause Eye Problems
Approximately 10% of those with ulcerative colitis an inflammatory bowel disease that causes tiny open sores, or ulcers, inside the lining of the colonalso have eye pain, vision problems, light sensitivity, and, in rare cases, permanent vision loss when either their UC or the related eye condition is left
What Did I Do

Faced with these sobering statistics regarding the current treatment of ulcerative colitis, I contacted the CCFA with the results of my research and treatment for this disease because they are the premier donor-funded research foundation for ulcerative colitis and Crohns disease whose mission is to discover the cause and cure for these diseases. I have emailed the CCFA on several occasions with my data since 2005. In my emails to Dr. Heller , CCFAs Chief Scientific Officer, I describe a specific and detailed evidence-based mechanism that explains how ulcerative colitis develops and how the treatment works. My emails to Dr. Heller underscore the reality that of extensive CCFA funded research have failed to find an antecedent immune abnormality to explain the cause of ulcerative colitis. I emphasized that continued donor-funded research into this unsubstantiated assumption will only generate endless research waste and more sales of expensive drugs aimed at altering the immune response that does not cure this condition. So how does the CCFA justify this line of research in search of the cause and cure for ulcerative colitis?
Don’t Miss: How Long Does Prednisone Take To Work For Ulcerative Colitis
How Is Ulcerative Colitis Different From Crohns Disease
Ulcerative colitis is different from other inflammatory bowel diseases like Crohns disease. Crohns can affect any area of the gastrointestinal tract, including the small intestine and colon. Ulcerative colitis, on the other hand, affects only the colon. The inflammation involves the entire rectum and extends continuously up the colon. There are no normal areas of the intestine between the areas of ulceration. In Crohns, the inflamed areas are scattered and can affect the entire thickness of the bowel wall.
Can I Live A Normal Life With Ulcerative Colitis
Even during times of remission, it is important to continue taking medications and seeing your doctor regularly. Studies show that people with UC usually have the same life expectancy as people without UC. It is important to remember that most people who have ulcerative colitis lead full, happy, and productive lives.
Also Check: Can Ulcerative Colitis Cause Bladder Problems
Lifestyle Changes For Ulcerative Colitis
UC leads to several symptoms, not just gastrointestinal ones. Aside from medications, other interventions and lifestyle changes, such as the following, can help improve health and quality of life.
- Promptly treat anemia. Low levels of iron, folate, and vitamin B-12 can all cause anemia. Low iron levels can develop with bleeding. Some medications can interfere with folate absorption. Vitamin B-12 deficiency may also develop. UC flares can make it difficult to get the full nutrition you need. So the cause of anemia always needs to be identified and treated promptly.
- Manage stress. Emotional stress is very strongly associated with UC. Prevent relapses with the help of stress-relieving exercises or therapies, yoga, and meditation.
- Get some exercise and stop smoking. Adding exercise and regular physical activity can help with UC. So can quitting smoking.
- Review your drug regimen. Certain medications such as nonsteroidal anti-inflammatory drugs can be associated with UC flares. If you have UC, consult your doctor before using an NSAID.
References For Introduction Section Of This Article:
1. Pravda J, Gordon R, Sylvestre P. Sustained Histologic Remission 12 Years after One-Time Treatment of Refractory Ulcerative Colitis with Novel Combination Therapy: A Case Report. Journal of Inflammatory Bowel Diseases and Disorders. 5:2020 1-5.
2. Pravda J, Weickert MJ, Wruble LD. . J Inflam Bowel Dis Disor. 2019 4: 130.
3. Jewell DP, Truelove SC. Reaginic hypersensitivity in ulcerative colitis. Gut. 1972 13:903-906.
4. Triantafillidis JK, et al. Cutaneous delayed hypersensitivity in Crohn’s disease and ulcerative colitis. Diseases of the colon & rectum. 1987 30:536-539.
5. Santhanam S, et al. Impairment of mitochondrial acetoacetyl CoA thiolase activity in the colonic mucosa of patients with ulcerative colitis. GUT 2007 56:1543-1549.
6. Shi XZ, Winston JH, Sarna SK. Differential immune and genetic responses in rat models of Crohn’s colitis and ulcerative colitis. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2011 300:G41-51.
7. Pravda J. Can Ulcerative Colitis Be Cured? Discovery Medicine. 2019 27 197-200.
8. Goldowsky A, Sen R, Hoffman G, Feuerstein JD. Is there a standardized practice for the development of international ulcerative colitis and Crohns disease treatment guidelines? Gastroenterology Report. 2021 Mar 29.
9. Feuerstein JD, et al. AGA clinical practice guidelines on the management of moderate to severe ulcerative colitis. Gastroenterology. 2020 Apr 1 158:1450-61.
16. University of Oxford, Center for Evidence Based Medicine.
Recommended Reading: Is Cranberry Juice Good For Ulcers
Living With An Ileostomy
You can live a long, active, and productive life with an ileostomy. In many cases, ileostomy patients can participate in the same activities they did before the surgery, including sports, outdoor activities, swimming and other watersports, travel, and work.
Whether your ileostomy is permanent or temporary, it is common for patients to initially feel self-conscious about their ostomy and you may notice a change in how you feel about your body image. Some patients prefer to limit how visible the bag is to others. The ostomy bag typically lays fairly flat under your clothing.
Remember, it is just as important to take care of your mental and emotional health as it is your physical health. Speak with your doctor or a mental health professional if you feel you are experiencing symptoms of depression or anxiety.
-
There are several pouching systems for you to choose from. You will learn how to use your system as well as how to care for the skin surrounding the stoma.
-
Talk to your doctor about any specific dietary restrictions with an ileostomy. It is important for you to drink plenty of fluids to avoid dehydration and loss of electrolytes.
-
Eating foods high in pectin, including applesauce, bananas, and peanut butter, will help thicken your stool output and control diarrhea. Discuss this with your doctor.
The United Ostomy Associations of America has additional resources as you learn to live with your ostomy.
How To Change Your Bag
Your surgeon will advise you to take the following steps for ostomy care:
Changing out your ostomy bag also provides you with an opportunity to look for any possible skin irritation.
Also Check: What Are The 4 Stages Of Pressure Ulcers
What Is Wrong With How Ulcerative Colitis Is Currently Treated
Current treatment guidelines are focused on altering/suppressing the immune response. Since there is no evidence of any immune abnormality causing ulcerative colitis these guidelines are not evidence-based. A 2021 study regarding the quality of currently accepted treatment guidelines for ulcerative colitis and Crohns disease concluded: The majority of UC and CD guidelines are based on a low/very low quality of evidence and are further weakened due to the lack of homogeneity in specific aspects of management recommendations as well as conflicts of interest .
What Is Surgery For Ulcerative Colitis
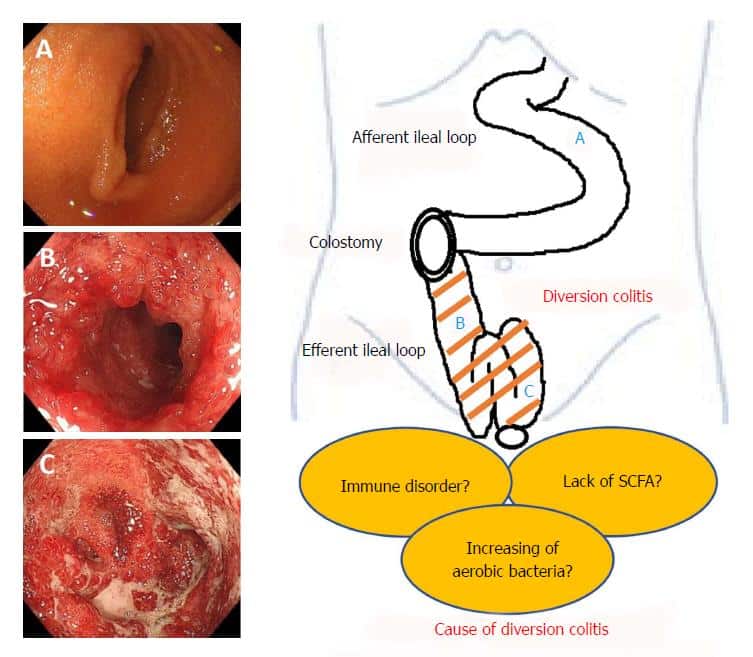
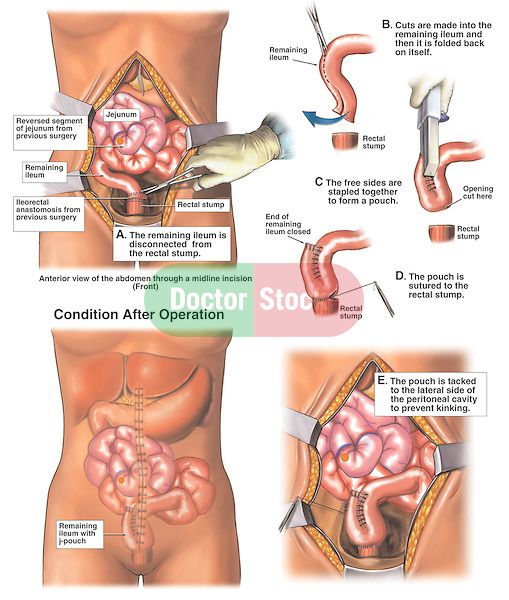
Surgery for ulcerative colitis means removing the large intestine, or colon . After the large intestine is gone, there needs to be another way for stool to leave the body. The two most common ways of achieving this are either by placing an ileostomy or creating a j-pouch.
In an ileostomy, a part of the small intestine is brought through the abdomen. This is called a stoma. Stool leaves the small intestine through the stoma and collects in an appliance . The ileostomy appliance is emptied into the toilet several times a day.
In an IPAA, or a j-pouch, the end of the small intestine is attached to the rectum. This is usually achieved through a series of two or three surgeries, although some surgeons will do it in a single operation. When done in more than one surgery, the first surgery is always a colectomy with placement of a temporary ileostomy.
These surgeries can be done through an open incision, or, as is more often the case now, laparoscopically . Ideally, the surgery is scheduled but is sometimes an emergency operation.
Read Also: Pressure Ulcer Cream Over The Counter
How Long Your Surgery Will Take
This will depend on the type of surgery youre having, whether it is keyhole or open surgery and if youve had surgery on your tummy before. If youve had surgery on your tummy before you may have scar tissue called adhesions. Adhesions can sometimes make surgery more complicated, so it can take longer. Your surgical team can tell you how long they expect your surgery to take.
After surgery youll be moved to a recovery ward. This is a small ward where nurses will monitor you as you wake up properly. The medicines that put you to sleep take a couple of hours to fully wear off. You may not remember waking up, or the first couple of hours after you wake up.
The medicines used during surgery can make you feel sick. You may also have a sore throat. This is usually because of the tube thats put into your throat to help you breathe during surgery. This tube is taken out when you wake up. If you feel unwell, let the nurses know and theyll be able to help you.
The 3 Key Goals Of Uc Treatment
There are treatments available that can help control excess inflammation in order to help you:
Controlling inflammation can help relieve UC symptoms such as frequent and urgent bowel movements, bloody stools, and abdominal pain.
Controlling inflammation can also help you achieve and maintain remission. This means you have achieved ongoing symptom relief and are able to prevent flares.
Controlling inflammation over time allows the lining of the colon to heal and can help you maintain remission.
Read Also: First Line Treatment Ulcerative Colitis
Pineapple Juice For Ulcerative Colitis Relief
One of the main protagonists of these home remedies to control ulcerative colitis is pineapple juice. The bromelain in pineapples is great to treat digestive diseases, since it has anti-inflammatory properties. In fact, by drinking two classes of pineapple juice every day , youll feel relief from your symptoms.
Also Check: List Of Foods To Eat With Ulcerative Colitis
Below Is My Email To Dr Caren Heller Chief Scientific Officer Of The Crohns Colitis Foundation Of America Sent On 27/july/2021 In This Email I Detail The Evidence Which Identifies Colonic Epithelial Hydrogen Peroxide As The Cause Of Ulcerative Colitis Her Response Follows Complete References Can Be Found At End Of This Article
Caren Heller MD, MBA, Chief Scientific Officer, Crohns Colitis Foundation of America
Andrés Hurtado-Lorenzo PhD, Vice president of translational research Crohns Colitis Foundation of America
Dear Drs. Heller and Hurtado-Lorenzo:
I am writing to follow up on my past correspondence with the Crohns Colitis Foundation of America about three exciting developments, which support the conclusion that colonic epithelial hydrogen peroxide has a causal role in the pathogenesis of ulcerative colitis and suggest that a cure for ulcerative colitis is within reach. I am sharing these encouraging results with other inflammatory bowel disease experts, research institutions, media outlets, and others who may want to evaluate the results we have obtained to perform further research and/or clinical investigation.
As you know, I initially contacted CCFA in 2005 to inform the organization of my published paper providing evidence that colonic epithelial hydrogen peroxide is the etiological agent responsible for the development of ulcerative colitis . Since that time, the following three important developments have occurred:
Video: Neutrophils attracted by cellular secretion of hydrogen peroxide :
A second study published in the American Journal of Physiology-Gastrointestinal and Liver Physiology concluded:
A 2021 study regarding the quality of treatment guidelines for ulcerative colitis and Crohns disease concluded:
Sincerely,
Jay Pravda MD MPH MBE
Recommended Reading: Genetic Testing For Ulcerative Colitis
Why Did I Get Ulcerative Colitis
Ulcerative Colitis Causes and Risk Factors Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders.
What is the main cause of ulcerative colitis?
The exact cause of ulcerative colitis remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but dont cause ulcerative colitis. One possible cause is an immune system malfunction.
Does Sunny Anderson have UC?
The Food Network star revealed that for the past 20 years, shes suffered from ulcerative colitis a chronic disease that affects the large intestine and doesnt allow her body to absorb nutrients as it should. Unfortunately, greens, along with vegetable and fruit skins, can trigger flare-ups.
What Is Ulcerative Colitis
Ulcerative colitis is a chronic disease of the colon or large intestine. It is marked by inflammation and ulceration in the colons innermost lining. Tiny, open sores form on the surface of this lining they bleed and produce pus and mucus. Because the inflammation makes the colon empty frequently, symptoms include diarrhea and, often, abdominal cramping.
The inflammation usually begins in the rectum and lower colon, but it may involve the entire colon. When it affects only the lowest part of the colon the rectum it is called ulcerative proctitis. If it affects only the left side of the colon, it is known as limited or distal colitis. Ulcerative colitis involving the entire colon is called pancolitis.
Recommended Reading: Stage 4 Pressure Ulcer Mortality
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
When Is Ulcerative Colitis Surgery Needed
Your doctor may suggest surgery if you can’t control inflammation and ulcers with medication or other treatments. You may also need an operation if you get emergency complications of ulcerative colitis such as severe bleeding or tears in the colon. Some people choose to have surgery if their symptoms affect their ability to work and stay active.
You May Like: Do Ulcers Make You Lose Weight
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Diagnosis Of Crohns Disease
The mainstay of diagnosis for Crohns disease is a combination of medical history, physical examination, laboratory tests, and imaging studies. The most common test used to diagnose Crohns disease is the colonoscopy which allows your doctor to see inside your large intestine and small intestine. Endoscopic procedures can also be undertaken if deemed necessary for diagnosis.
Dont Miss: What Can I Eat When I Have Ulcerative Colitis
You May Like: How To Heal Leg Ulcers Quickly
Can Colon Surgery Treat My Ulcerative Colitis
Nearly a million Americans have ulcerative colitis, a disease that causes sore and inflammation in your large intestine and rectum. Ulcerative colitis is an inflammatory bowel disease with symptoms that develop slowly over time.
Ulcerative colitis can cause serious, life-threatening complications unless its actively and appropriately managed with medical care customized for your symptoms and the progression of the disease. At Desert West Surgery, our team is skilled in tailoring ulcerative colitis treatment, including conservative treatments and colon surgery, to help every patient achieve the best outcomes.