What Are The Complications Of Urinary Retention
Complications may include:
- Urinary tract infection . When urine stays in the bladder, bacteria can grow and infect the urinary tract.
- Bladder damage. If the bladder becomes stretched too far or for long periods of time, the muscle may be permanently damaged and lose its ability to contract.
- Chronic kidney disease. If urine backs up into the kidneys it can lead to permanent kidney damage, reduced kidney function and chronic kidney disease.
Changes In Bladder Voiding Parameters
As an immediate comparison with the clinical symptoms of OAB and IC/PBS, there have been a number of well-documented studies into the effects of transient colitis on bladder voiding. During the acute phase of trinitrobenzesulfonic acid -induced colitis in rodents, when colonic inflammation is pronounced, there are consistent changes in bladder voiding parameters. This includes deceased micturition intervals, decreased voided volumes, and decreased bladder capacity, as well as increased micturition frequency . By 7 days post-TNBS administration, colonic inflammation has begun to spontaneously resolve, with a corresponding increase in the integrity of the colonic wall. By 28 days post-TNBS, there are no observable histological changes in the colon compared with healthy control mice . However, changes in bladder micturition parameters remain altered at 10 and 12 days post-TNBS and may persist long term . Accordingly, these studies indicate that transient experimental colitis can have profound acute and long-term effects on bladder function following resolution of the initial inflammatory stimuli. This provides us with the closest possible analogy to the symptoms of urgency, urge incontinence, and frequency observed in humans with OAB and IC/PBS .
Table 1. Reported changes in bladder function in response to experimental colitis
What Gets Stored In A Cookie
This site stores nothing other than an automatically generated session ID in the cookie no other information is captured.
In general, only the information that you provide, or the choices you make while visiting a web site, can be stored in a cookie. For example, the site cannot determine your email name unless you choose to type it. Allowing a website to create a cookie does not give that or any other site access to the rest of your computer, and only the site that created the cookie can read it.
Read Also: Do Ulcers Cause Acid Reflux
Can Stomach Bloating Be A Sign Of Kidney Failure
My husband was diagnosed in October with stage 3 chronic kidney disease and has not yet been seen by kidney doctor I was not aware of his chronic kidney disease because his doctor never discussed it with me he went to his doctor on March the 20th and I didnt realize he had chronic kidney disease until around March the 27th when I called about his blood work and thats when they told me he was diagnosed in October we went on April the 20th 2018 for blood work at the kidney doctor he has an appointment on May 3rd for the results of his blood work but he keeps talking about hurting it in his stomach both sides underneath his rib cage he had a colonoscopy done
Read Also: Can Hemorrhoids Cause Abdominal Pain And Bloating
Crohns Vs Ulcerative Colitis
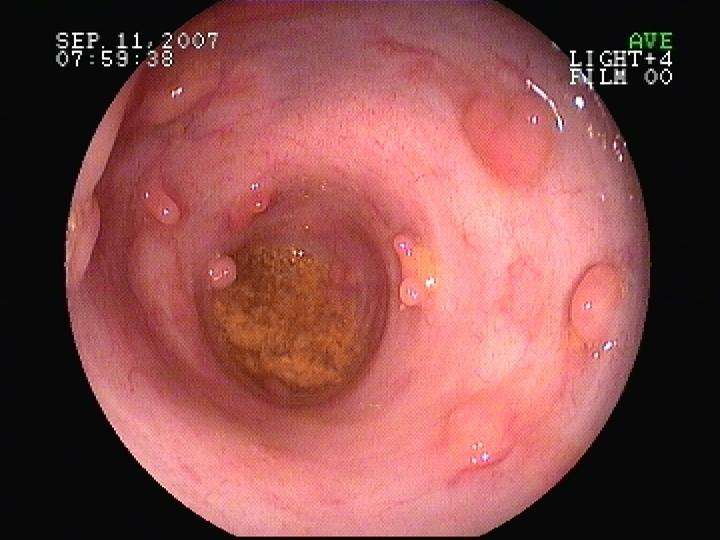
Crohnâs disease is often confused with another condition called ulcerative colitis. The symptoms are similar, and both involve periods of active flare-ups, followed by times when you donât have symptoms, which is called remission.
The only way to find out if you have Crohnâs or ulcerative colitis is to see your doctor for tests.
Also Check: What Can I Eat With A Stomach Ulcer
Complications Of Ulcerative Colitis
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
“It’s easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,” says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
Have A Uti It Could Be Related To Your Ibd Treatment
Many women will experience at least one urinary tract infection in their lifetime and men can experience UTIs, too. In fact, UTIs are the reason over 8.1 million people visit their doctor each year.1 But did you know that UTIs can be related to biologics for inflammatory bowel disease ?
While upper respiratory infections are a common side effect of biologics for IBD, most people dont know that UTIs are another type of infection that can be related to your IBD treatment, explains Faten N. Aberra, MD, MSCE, associate professor of medicine in the division of gastroenterology at the University of Pennsylvania in Philadelphia.
Why the increased risk? Biologics suppress your immune system increasing your risk of an infection like a UTI.
Read Also: Air Mattress For Decubitus Ulcers
Symptoms Of Ulcerative Colitis:
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. The most common symptoms are diarrhea with blood or pus, and abdominal discomfort. It often begins gradually and can become worse over time, though there may be periods of remission that can last for weeks or years.
Other symptoms include:
Also Check: Is Ginger Tea Good For Kidneys
Mixing Tolterodine With Herbal Remedies And Supplements
There might be a problem using herbal remedies and supplements while taking tolterodine.
Some herbal medicines can make you feel sleepy, cause a dry mouth, or make it difficult to pee. Their effect is similar to tolterodine. This can increase your risk of getting side effects or make your side effects worse.
You May Like: Can Ulcers In The Esophagus Cause Cancer
How Does Kidney Infection Affect Your Stomach
Stomach is one of essential organs of your digestive system. And the kidneys are part of your urinary system. But sometime they can affect each other if one of them goes awry. For instance if you have infection in the kidney, it may also cause pain in the stomach. There are a number of ways of how kidney infection can affect your stomach.
Unique Mechanisms In Ibd Patients Prompt Revised Guidelines
Although both gallstones and kidney stones may be associated with IBD, the studys authors described different mechanisms that may influence their development. Without sufficient ileal activity, for example, they noted that a patients bile may contain excess bilirubin, which may form gallstones. Furthermore, a patient with IBD may experience multiple effects in the digestive tract that potentiate a risk of gallstones.
Kidney stones typically form due to a high abundance of oxalate or similar compounds in the urine, according to the study publication. IBD may result in more concentrated urine due to factors such as dehydration from diarrhea and dysregulation of absorptionof salts in the ileum. An ileostomy may also result in urine that is more acidic.
Dr.Fagagnini and her co-authors suggested that clinical trials further explore treatment and relationships between IBD and the development of gallstones and kidney stones. Specifically, they recommended studying the use of ursodeoxycholic acid in IBD patients at risk of gallstones and a diet low in oxalate and high in fluid, with decreased ingestion of some fatty acids, for IBD patients at higher risk of kidney stones.
The authors disclosed no competing financial interests.
Read Also: Best Way To Heal Stomach Ulcers
Activation Of Creb In Bladder Afferent Neurons Post Colitis Was Regulated By Endogenous Bdnf
Bladder afferent activity was examined by the expression level of p-CREB in specifically labeled primary afferent neurons that innervated the urinary bladder. The L1L2 and L6S1 DRGs were identified and extracted from control rats and rats that received TNBS treatment and survived for 7 days and 21 days. Western blot of CREB phosphorylation on serine 133 was conducted in DRG samples from control animals and animals at 7 days and 21 days post colitis induction. Although the degree of colonic inflammation was subsided at day 7 and significantly recovered by day 21 , the levels of p-CREB in the DRGs were sustained at both 7 days and 21 days . There were significant 2-fold increases in the level of p-CREB at both 7 days and 21 days post colitis induction . We then performed immunostaining of the DRG cryosections with a specific antibody against p-CREB on serine 133. We found that p-CREB was expressed in the nucleus of DRG neurons in all DRGs examined. The p-CREB immunoreactivity in the neurons was examined and showed increases post colitis induction , confirming the western blot results .
CREB activity was increased in the DRG post colitisPLC expression was increased in bladder afferent neurons post colitis
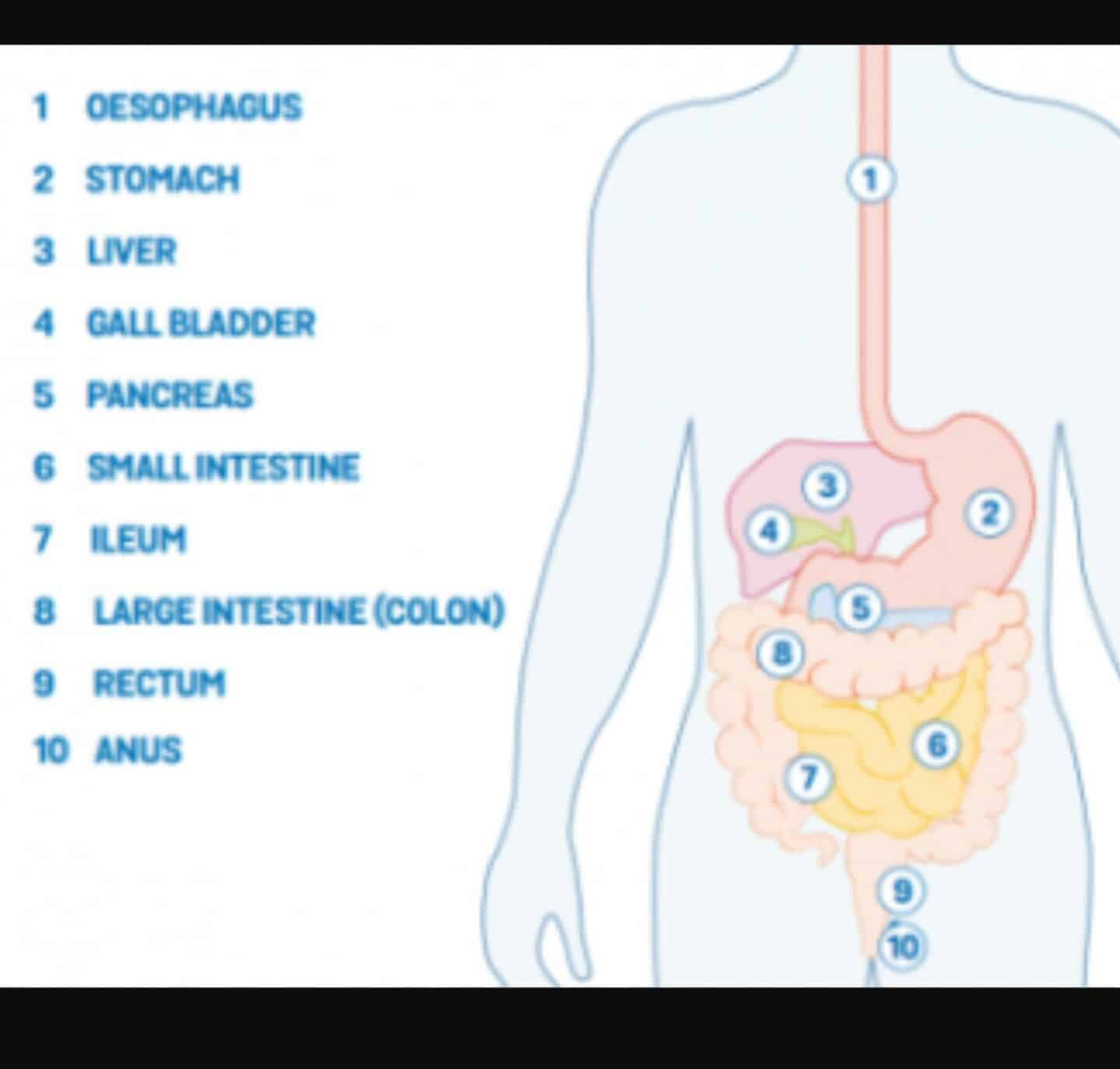
Inflammatory Bowel Disease And Colitis
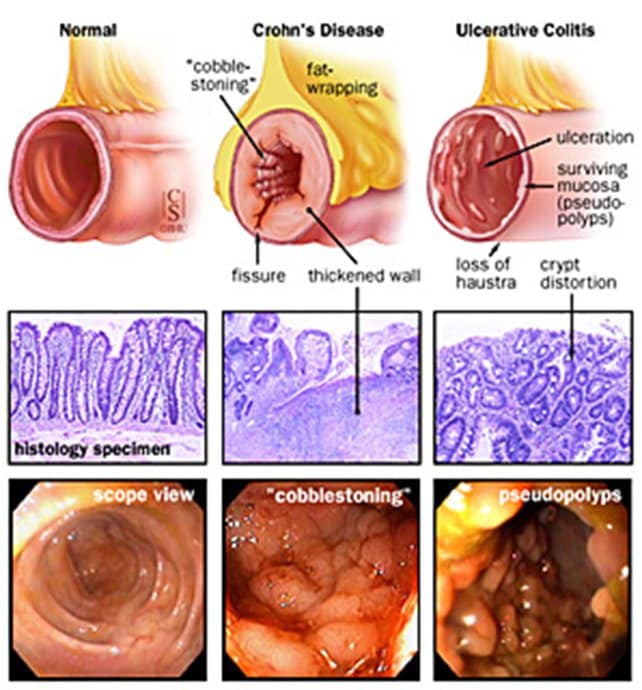
Ulcerative colitis and Crohns disease are the two types of inflammatory bowel disease that cause colitis. Crohns disease and ulcerative colitis are considered autoimmune diseases .
- Ulcerative colitis always begins in the rectum and may spread to the rest of the rest of the colon, spreading from the rectum to the sigmoid, descending, transverse, and finally the ascending colon and cecum in that order. Ulcerative colitis is considered an autoimmune disease, and symptoms include abdominal pain, and bloody, diarrheal bowel movements.
- Crohns disease may occur anywhere in the gastrointestinal tract , including the esophagus, stomach, small intestine, and colon. In Crohns disease, there may be skip lesions, that is, abnormal segments of the GI tract interspersed with normal segments.
Both Crohns disease and ulcerative colitis may have other organ systems involved in addition to the gastrointestinal tract.
Either collagen or lymphocytes infiltrate into the layers of the wall of the colon, presumably as a result of inflammation. This is an uncommon illness and maybe an autoimmune disease. Diarrhea often is watery, and no blood is present in the stool.
Also Check: How To Stop Rectal Bleeding From Ulcerative Colitis
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Also Check: How To Heal Ulcers In Large Intestine
Surgery For Ulcerative Colitis
Despite drug therapies, approximately one-third of people with ulcerative colitis will need surgery to treat the inflammation, prevent or treat cancer, or to treat a complication such as rupture of the colon. Surgery in which the entire colon is removed cures the person of their ulcerative colitis. In the past they were left with ileostomies, external bags into which the small intestine emptied. Surgical techniques have been developed, however, that now allow the colon to be removed without the need for an ileostomy.
Recommended Reading: Best Pain Relief For Leg Ulcers
Also Check: Prevention Of Diabetic Foot Ulcer
Living With Ulcerative Colitis And Kidney Disease
If you are living with UC and kidney disease, it is important to maintain a healthy lifestyle. Many MyCrohnsAndColitisTeam members have shared their tips on how they live with UC and kidney disease. I have regular appointments with my urologist/kidney specialist to check my blood and urine, one member noted. Another said, I exercise and stay at a good weight, while a third member wrote, I try to get enough potassium and vitamin D in my diet.
Recommended Reading: Vsl 3 And Ulcerative Colitis
Who Can And Cannot Take Tolterodine
Tolterodine can be taken by most adults. It can also be taken by children aged 2 years and over, on the advice of their specialist.
Tolterodine is not suitable for some people. To make sure it’s safe for you, tell your doctor or pharmacist before starting tolterodine if you:
- have ever had an allergic reaction to tolterodine or any other medicine
- have kidney or liver problems
- have myasthenia gravis, a condition that causes muscle weakness
- have digestive problems such as heartburn and acid reflux
- are pregnant, trying to get pregnant or breastfeeding
Recommended Reading: Gastric Ulcer Treatment At Home
Colitis And Crohns What Is The Difference
Ulcerative Colitis and Crohns Disease are long term illnesses but they do have differences. Ulcerative Colitis affects only the inner lining of the large bowel and Crohns Disease can affect all layers of the lining of any part of the intestines and other parts of the digestive system.
It is important to get a clear diagnosis of Ulcerative Colitis or Crohns as both conditions can be treated by drugs and/or surgery.
When To Contact A Doctor
People need to discuss any blood in the stools with their doctor, even if they have experienced it before.
A person may also wish to monitor their UC symptoms, so they know what is usual for them to experience. People can then discuss any abnormal symptoms with a healthcare professional.
If individuals have ongoing diarrhea that lasts for a couple of weeks, they can contact their doctor to discuss concerns and treatment.
The Crohnâs and Colitis Foundation advises people to seek emergency medical attention if they experience any of the following:
- inability to keep down liquids due to nausea, vomiting, or pain
- rectal bleeding with blood clots in stools
- continuous pain
Managing UC with treatment may help reduce bleeding. There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding.
Anti-inflammatory medications for UC can include:
- 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
- Corticosteroids: A short-term treatment to help reduce inflammation.
- Immunosuppressants: These medications can help suppress the immune response that can cause inflammation. However, they may take up to 6 months to be effective.
- Biologics: For treatment of moderate to severe UC, biologics help block molecules that trigger inflammation.
Read Also: Can You Take Imodium If You Have Ulcerative Colitis
Effects Of Crohns Disease And Ulcerative Colitis
Every person responds differently to IBD. The severity of symptoms will vary from time to time and from person to person. IBD is not a progressive disease . Rather, flare-ups can range from mild to severe and back to mild again. Some people will experience periods of relief from symptoms in between flare-ups.We cannot predict how long a person will stay free from symptoms, or when their next flare-up will occur. Some flare-ups settle down quite quickly with treatment. Other times, it may take months for a persons symptoms to respond to treatment.IBD interferes with a persons normal body functions. Signs and symptoms can include:
- pain in the abdomen
In addition to the above prevention methods, women can also:
- Avoid contraceptive methods that contain spermicide
- Avoid using a diaphragm as a birth control method
- Avoid the use of feminine products on genital regions, such as deodorant sprays and douches, which have the potential to irritate the urethra
- Receive vaccination against certain E. coli strains
Why Is Inflammatory Bowel Disease Linked With Gallstones
There are several reasons that people with Crohnâs disease are at risk for gallstones:
Donât Miss: C Diff And Ulcerative Colitis Treatment
You May Like: Easy To Digest Foods For Ulcerative Colitis
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.