Patient Information And Support
1.1.1 Discuss the disease and associated symptoms, treatment options and monitoring:
-
with the person with ulcerative colitis and their family members or carers and
-
within the multidisciplinary team at every opportunity.Apply the principles in the NICE guideline on patient experience in adult NHS services.
1.1.2 Discuss the possible nature, frequency and severity of side effects of drug treatment for ulcerative colitis with the person, and their family members or carers . Refer to the NICE guideline on medicines adherence.
1.1.3 Give the person, and their family members or carers information about their risk of developing colorectal cancer and about colonoscopic surveillance, in line with the NICE guidelines on colorectal cancer prevention: colonoscopic surveillance in adults with ulcerative colitis, Crohn’s disease or adenomas and suspected cancer: recognition and referral.
Management Of Hospitalized Patients With Acute Severe Ulcerative Colitis
| 8. In hospitalized adult patients with acute severe ulcerative colitis, the AGA suggests using intravenous methylprednisolone dose equivalent of 40 to 60mg/d rather than higher dose intravenous corticosteroids. |
The guideline panel suggests using intravenous corticosteroids at doses equivalent to 4060mg/day of methylprednisolone rather than higher doses of intravenous corticosteroids to decrease risk of colectomy in hospitalized adults with ASUC.
Intravenous corticosteroids are the mainstay of management of hospitalized adults with ASUC. There were no head-to-head trials comparing different doses of corticosteroids in hospitalized patients with ASUC. In a systematic review evaluating the risk factors for colectomy in patients with ASUC, Turner and colleagues observed that mean methylprednisolone dose was 68mg/day in hospitalized patients with ASUC on meta-regression after controlling for baseline disease severity, there was no correlation between corticosteroid dose and risk of colectomy .32 In included trials, different intravenous corticosteroid regimens were used, and none was superior to others. Based on models estimating risk and risk factors for colectomy in patients with ASUC, corticosteroid trials of 35 days are suggested continued use of corticosteroids beyond 7 days has not been shown to be effective in non-responding patients.32, 33
Surgical Management Of Acute Severe Uc
Colectomy should be considered early in the management of ASUC in patients with intestinal perforation, exsanguinating haemorrhage or toxic megacolon. Otherwise a colectomy should be considered after three days of hospitalisation in patients with steroid refractory disease deemed inappropriate for second-line therapy, or where there has been no improvement within seven days after the introduction of rescue therapy. Planned colectomy is associated with significantly improved morbidity and mortality rates in comparison with urgent colectomy, which highlights the importance of promptly identifying patients likely to require surgical intervention. Colectomy with ileostomy is the preferred initial operation. A completion proctectomy with pouch can be planned at a later date, once the patient has improved physically and nutritionally.
You May Like: How Would I Know If I Had An Ulcer
What Are The Long
The long-term outlook for ASUC is guarded. There is a 20% chance that you’ll need colectomy surgery after your first hospitalization, but that chance rises to 40% after two hospital admissions for ASUC. Severe flares are linked to a 1% risk of death.
Older age is linked with higher death rates. The death rate from ASUC is over 10% in people over 80 compared to fewer than 2% for people between the ages of 50 and 59.
UC is a chronic disease with no cure. Developing acute, severe symptoms is a risk for up to 20% of those diagnosed with the disease. With hospitalization, medical management, and a knowledgeable health care team, you can recover from a bout of ASUC and go into remission, but new flares are possible.
Show Sources
Accelerated/intensified Infliximab Dosing For Asuc
Two studies have demonstrated that higher infliximab serum concentrations are associated with greater efficacy and better outcomes . Moreover, the are several other factors that would support the need for dose optimisation of infliximab in the acute phase. These include the high TNF burden in ASUC, the proteolytic degradation of anti-TNF associated with increased drug clearance and faecal losses from increased gut permeability associated with severe inflammation . According to BSG guidelines, patients who have not responded sufficiently 35 days after the first infliximab infusion should be treated with an accelerated induction regimen after a colorectal surgical review to exclude the need for emergency colectomy . Some clinicians also use an initial 10 mg/kg dose as salvage therapy, however, optimal timing and dose are yet to be defined and further studies are needed for dose intensification to be implemented into clinical practice.
Recommended Reading: Good Diet For Stomach Ulcers
Technical And Postoperative Considerations
For most patients with UC undergoing restorative total proctocolectomy with IPAA, a two-stage, three-stage, or modified two-stage approach is preferred.
For patients with UC undergoing elective surgery, acceptable options include total proctocolectomy with IPAA, end ileostomy, or continent ileostomy.
Total abdominal colectomy with ileorectal anastomosis may be considered in selected patients who have UC with relative rectal sparing .
Counsel patients with UC undergoing proctectomy about potential effects on fertility, pregnancy, sexual function, and urinary function.
Pouchitis is common after IPAA performed in the setting of UC and is classified according to its responsiveness to antibiotics.
Optimal Dose Targeting Is Primordial
Several lines of evidence suggest that conventional weight-based dosing of infliximab salvage therapy might be insufficient in ASUC. The severe intestinal inflammation is associated with an important intestinal loss of protein resulting in hypoalbuminaemia but also a rapid clearance of infliximab in the faeces.58 Additionally, high concentrations of mucosal metalloproteinases, associated with inflammation, lead to degradation and inactivation of anti-TNF antibodies.59,60
In a pharmacokinetic study, Brandse et al showed that patients with a faster intestinal clearance of infliximab were at risk for worse clinical outcomes and had an increased chance of infusion-related reactions compared to patients with a normal drug clearance. Drug clearance seemed to be highest in the group of patients with higher CRP levels .59 In a retrospective analysis of 50 patients hospitalized for ASUC an accelerated dosing strategy of infliximab was associated with a lower colectomy rate .61 However, in another multicentre, retrospective study including 213 patients with steroid refractory ASUC no difference was found between normal and accelerated dosing strategy, although dosing regimens including a higher induction dose of infliximab were associated with a lower rate of colectomy.62
Patients not responding to rescue therapy with infliximab or cyclosporin by day 7 or that develop serious complications earlier should be referred for colectomy.25
Don’t Miss: Compression Stockings For Venous Leg Ulcers
Adaptations To The Bsg Guidelines On The Management Of Acute Severe Ulcerative Colitis In The Context Of The Covid
Our advice and guidance around COVID-19 is being regularly reviewed. Visit to see the latest published guidance.
Abstract:
Objective
Management of acute severe ulcerative colitis during the novel coronavirus 2019 pandemic presents significant dilemmas. We aimed to provide COVID-19-specific guidance using current British Society of Gastroenterology guidelines as a reference point.
Design
We convened a RAND appropriateness panel comprising 14 gastroenterologists and an IBD nurse consultant supplemented by surgical and COVID-19 experts. Panellists rated the appropriateness of interventions for ASUC in the context of severe acute respiratory syndrome coronavirus-2 infection. Median scores and disagreement index were calculated. Results were discussed at a moderated meeting prior to a second survey.
Results
We have suggested COVID-19-specific adaptations to the BSG ASUC guideline using a RAND Panel.
Challenge : Identifying Patients At Risk Remains A Problem In Clinical Practise
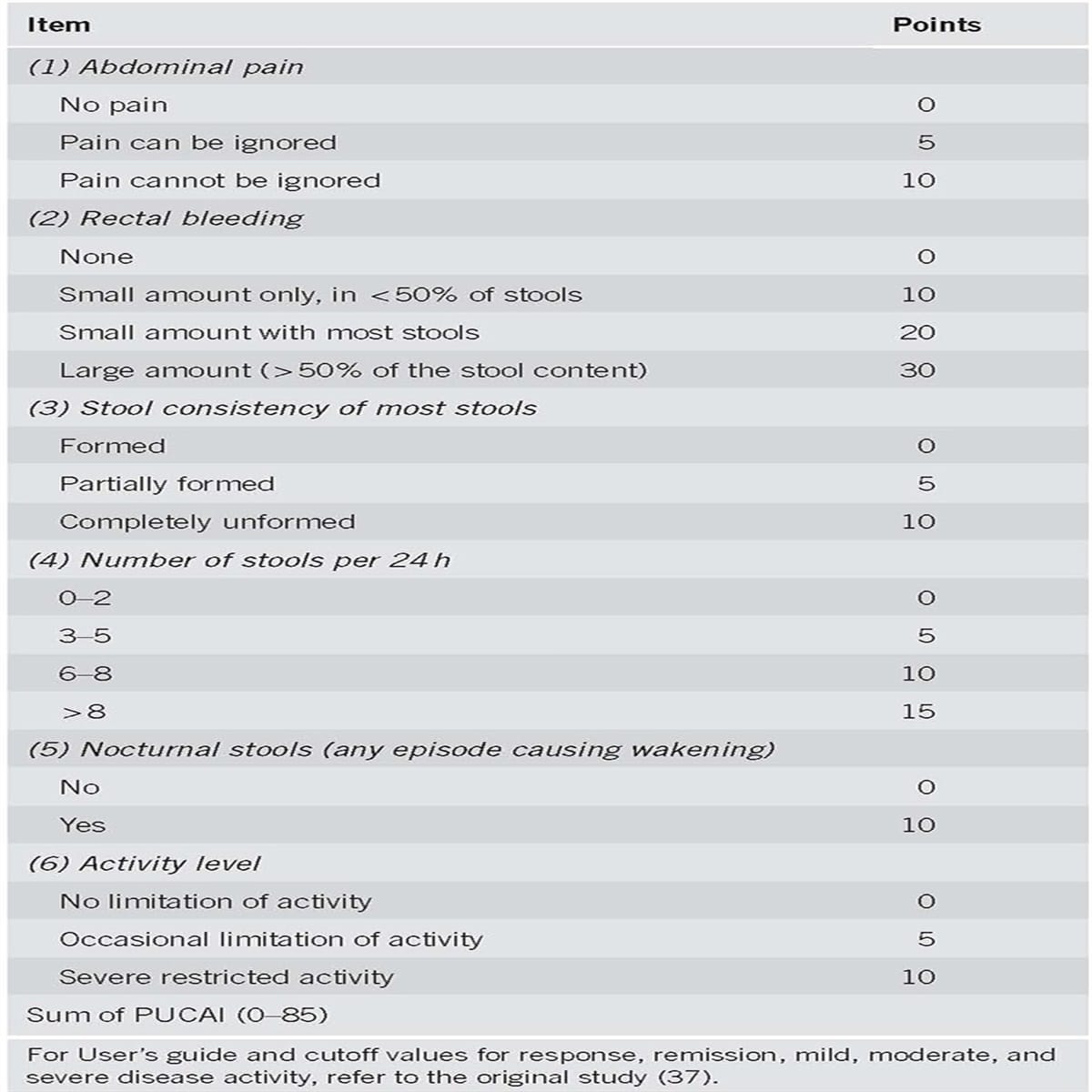
Early diagnosis of ASUC is historically based on the Truelove and Witts criteria consisting of the presence of bloody stools 6 times a day and at least one of the following signs of systemic toxicity: pulse rate > 90 bpm, temperature > 37.8, haemoglobin < 10.5 g/dl or erythrocyte sedimentation rate > 30 mm/h. Despite being 60 years old, they still remain the most sensitive criteria to define ASUC, although they must always be applied and considered in view of the circumstances and setting.7 Other indices like the clinical partial Mayo clinic score and the Montreal classification are less frequently used in clinical practise, however comparative studies for diagnosis of ASUC are not available.3,8
|
Table 1 Truelove and Witts Criteria for Acute Severe Ulcerative Colitis |
Predicting which patients are likely to fail initial treatment with corticosteroids is essential in the management of ASUC. This allows for early and multidisciplinary planning of medical and/or surgical rescue therapy.3,8 Several predictive indices have been developed but are infrequently used in clinical practise.
|
Table 2 Predictive Indices for Corticosteroid Failure in Acute Severe Ulcerative Colitis |
Lastly, plain abdominal radiography can also provide prognostic information. The presence of visible mucosal islands or a colonic diameter of > 5.5 cm predicts corticosteroid failure in 75% of patients.10 Additionally, small bowel distention conveys an increased risk for colectomy during the same admission.19
You May Like: How Can You Get Rid Of Ulcers
Toxic Megacolon And Other Complications Of Severe Uc
Toxic megacolon may be defined as colonic dilatation of more than 5.5 cm along with signs of systemic toxicity. Lifetime incidence of toxic megacolon in patients with UC varies from 1%-2.5% and approximately 5% severe UC patients who are hospitalized may develop toxic megacolon. Risk factors include dyselectrolytemia, full bowel preparation and medications . Earlier identification of this condition, prompt institution of medical therapy and low threshold of surgery in cases of non-response to medical therapy within 48 h will decrease the morbidity and mortality of this condition.
Other complications include perforation which is the most serious complication of severe UC. Risk factors include inappropriate total colonoscopy and delaying treatment of toxic megacolon. Diagnosis of perforation can often be delayed as abdominal signs can be masked when patient is on steroids. Therefore, patients with severe UC should be monitored closely for abdominal signs and on the slightest suspicion abdominal radiographs should be obtained. Other complication includes severe hemorrhage.
What Is Acute Severe Ulcerative Colitis
Acute severe ulcerative colitis is a serious complication of ulcerative colitis. Itâs diagnosed when the disease flares and causes frequent bowel movements and bloody diarrhea, rapid heart rate, abdominal tenderness, fever, high levels of inflammation, and anemia. Inflammation in the intestinal wall makes the colon swollen and dilated, causing the stomach to become bloated. This is linked to a risk of developing toxic megacolon, the most serious complication of colitis.
ASUC is considered a medical emergency, and you’ll probably be hospitalized to help manage the disease. Without treatment, ASUC could be life-threatening.
Also Check: What Makes Ulcerative Colitis Worse
Hydration Electrolytes And Nutritional Status
In addition to corticosteroids to reduce inflammation, most patients need intravenous fluids. These treat dehydration and correct electrolyte imbalance due to severe diarrhea, vomiting, and bleeding. Patients are at most risk for hypokalemia and iron deficiency anemia. In some cases, enteral nutrition support may also be helpful.
Maintaining Remission In People With Ulcerative Colitis
Proctitis and proctosigmoiditis
1.4.1 To maintain remission after a mild-to-moderate inflammatory exacerbation of proctitis or proctosigmoiditis, consider the following options, taking into account the person’s preferences:
-
a topical aminosalicylate alone or
-
an oral aminosalicylate plus a topical aminosalicylate or
-
an oral aminosalicylate alone, explaining that this may not be as effective as combined treatment or an intermittent topical aminosalicylate alone. In May 2019, note that this was an off-label use of some aminosalicylates for children and young people. See NICE’s information on prescribing medicines
Left-sided and extensive ulcerative colitis
1.4.2 To maintain remission in adults after a mild-to-moderate inflammatory exacerbation of left-sided or extensive ulcerative colitis:
-
offer a low maintenance dose of an oral aminosalicylate
-
when deciding which oral aminosalicylate to use, take into account the person’s preferences, side effects and cost.
1.4.3 To maintain remission in children and young people after a mild-to-moderate inflammatory exacerbation of left-sided or extensive ulcerative colitis:
-
offer an oral aminosalicylate
-
when deciding which oral aminosalicylate to use, take into account the person’s preferences , side effects and cost. In May 2019, this was an off-label use of some oral aminosalicylates for children and young people. See NICE’s information on prescribing medicines.
All extents of disease
Dosing regimen for oral aminosalicylates
Read Also: What Can I Eat With Ulcerative Colitis
Induction Of Remission In Mildly
5-aminosalicylates
We recommend 5-aminosalicylates at a dose of 2 g/day to induce remission in patients with mildly-to-moderately active UC
We performed a meta-analysis of 11 eligible RCTs with a total of 2156 patients evaluated for 412 weeks 5-aminosalicylates had a significantly higher efficacy in achieving clinical remission versus placebo . Similarly, the clinical response in 14 studies evaluated at 210 weeks was significantly better for 5-ASA with response in 59% of patients receiving 5-ASA compared with 35% of those receiving placebo. The efficacy of 5-ASA on endoscopic response as evaluated in four RCTs with 416 patients investigated after 412 weeks was better with 5-ASA 5-ASA was generally very well tolerated. The serious adverse event rate evaluated in 13 studies with 2141 patients for a maximal follow-up of 12 weeks was 6.1% versus 9% in the placebo arms .
The quality of evidence was globally evaluated as low due to significant heterogeneity and possible publication and reporting bias for certain outcomes .
We recommend topical 5-ASA at a dose of1 g/d for the induction of remission in active distal colitis
Overall, the quality of available evidence was classified as low. Despite this, our recommendation is strong considering the extensive clinical experience corroborating efficacy and very few SAEs related to topical 5-ASA administration.
Topical corticosteroids
Colonic-release corticosteroids
Immunomodulators
Potential Areas For Future Investigation
Appendectomy may reduce the need for proctocolectomy associated with medically refractory disease .
In the setting of worsening, acute, severe UC, a “rescue” diverting loop ileostomy can be considered to potentially avoid an emergent total abdominal colectomy .
Consider extended postoperative venous thromboembolism prophylaxis in patients with UC exposed to tofacitinib .
References
Murata I, Satoh K, Yoshikawa I, Masumoto A, Sasaki E, Otsuki M. Recurrent subcutaneous abscess of the sternal region in ulcerative colitis. Am J Gastroenterol. 1999 Mar. 94:844-5. .
Kimura K, Hunter SF, Thollander MS, et al. Concurrence of inflammatory bowel disease and multiple sclerosis. Mayo Clin Proc. 2000 Aug. 75:802-6. .
Egan CA, Meadows KP, Zone JJ. Ulcerative colitis and immunobullous disease cured by colectomy. Arch Dermatol. 1999 Feb. 135:214-5. .
Bernstein CN, Eliakim A, Fedail S, et al. World Gastroenterology Organisation global guidelines: inflammatory bowel disease: update August 2015. J Clin Gastroenterol. 2016 Nov/Dec. 50:803-8. . .
Esteve M, Gisbert JP. Severe ulcerative colitis: at what point should we define resistance to steroids?. World J Gastroenterol. 2008 Sep 28. 14:5504-7. . .
Shen B. Crohn’s disease of the ileal pouch: reality, diagnosis, and management. Inflamm Bowel Dis. 2009 Feb. 15:284-94. .
Van Assche G, Vermeire S, Rutgeerts P. Treatment of severe steroid refractory ulcerative colitis. World J Gastroenterol. 2008 Sep 28. 14:5508-11. . .
Don’t Miss: Can I Join The Military With Ulcerative Colitis
Medical Management Of Moderately
5.1. Induction of remission in moderately-to-severely active ulcerative colitis
Systemic corticosteroids
We recommend oral prednisolone for induction of remission in non-hospitalised patients with moderately-to-severely active UC
Despite a limited evidence base, the use of systemic corticosteroids for the induction of remission in moderately-to-severely active UC is well established in clinical practice. The limited evidence is due in part to the large effect size and limited alternative options at the time of the original RCTs., A previous meta-analysis included five placebo-controlled RCTs, although only two of them, used standard systemic corticosteroids. Therefore, we performed a meta-analysis of just these two studies and calculated an RR of 2.83 for the induction of clinical remission. The quality of evidence was rated as very low, due to a serious risk of bias, indirectness, and imprecision .
No information regarding AEs with steroid treatment was available in these two studies. Other studies established the side-effect profile of corticosteroids in both short courses and also longer-term exposure in both UC and Crohns disease., Due to the potential for side effects, some of which are irreversible, corticosteroid-free remission represents a desired outcome for patients.,
Anti-tumour necrosis factor agents
Vedolizumab
Tofacitinib
Ustekinumab
5.2. Maintenance of remission of moderately-to-severely active ulcerative colitis
Anti-TNF agents
Vedolizumab
Tofacitinib
Solutions Towards A Better Asuc Management In The Future
Despite the fact that numerous challenges remain to be solved in ASUC management, current evidence does already provide several solutions to improve our current care of patients with ASUC. How we can integrate these in clinical practise is represented in Figure 1 and Box 1.25
|
Figure 1 Treatment algorithm for acute severe ulcerative colitis. Adapted with permission from Hindryckx P, Jairath V, DHaens G. Acute severe ulcerative colitis:from pathophysiology to clinical management. Nat Rev GastroenterolHepatol. 2016 13:654664. Copyright © 2016, Nature Publishing Group, a division of Macmillan Publishers Limited. All Rights Reserved.3 |
|
Box 1 Tips to Improve Your Care of ASUC Patients |
Don’t Miss: How To Treat Ulcerative Colitis Pain
Information About Treatment Options For People Who Are Considering Surgery
These recommendations apply to anyone with ulcerative colitis considering elective surgery. The principles can also be applied to people requiring emergency surgery.
Information when considering surgery
1.3.1 For people with ulcerative colitis who are considering surgery, ensure that a specialist gives the person and their family members or carers information about all available treatment options, and discusses this with them. Information should include the benefits and risks of the different treatments and the potential consequences of no treatment.
1.3.2 Ensure that the person and their family members or carers have sufficient time and opportunities to think about the options and the implications of the different treatments.
1.3.3 Ensure that a colorectal surgeon gives any person who is considering surgery and their family members or carers specific information about what they can expect in the short and long term after surgery, and discusses this with them.
1.3.4 Ensure that a specialist gives any person who is considering surgery and their family members or carers information about:
-
psychological wellbeing
-
the type of surgery, the possibility of needing a stoma and stoma care.
1.3.5 Ensure that a specialist who is knowledgeable about stomas gives any person who is having surgery and their family members or carers specific information about the siting, care and management of stomas.
Information after surgery