What To Expect After Surgery
After the first surgery, a person will stay in the hospital for a short period to recover and learn to care for their temporary ileostomy.
Once the second or third procedure is complete, a person will generally have another brief hospital stay before the healthcare team discharges them to finish their recovery at home.
During the recovery period, a person who has had J-pouch surgery may notice the following:
- fatigue, which will lessen over time as the body heals
- an increased number of bowel movements, which should decrease as the stool thickens
- increased need to pass stools at night
- stool leakage and mild incontinence, which should decrease over time
- dehydration associated with diarrhea
- streaks of blood in the stool
Certain risks accompany any major surgery. According to the Crohns & Colitis Foundation, risks specific to J-pouch surgery include:
- pelvic abscesses and fistulas
The American College of Gastroenterology also points out that it might be more difficult for a person to get pregnant naturally following the procedure.
Of these complications, pouchitis is the most common. Doctors can treat it with a course of antibiotics.
I tell people that they will likely develop pouchitis at some point in their life following the procedure, said Dr. Wexner. However, most of the people I talk to would rather have a bout of pouchitis over a colitis flare.
Hyperthermic Intraperitoneal Chemotherapy Surgery
HIPEC is a unique surgery used to treat cancers in the abdominal cavity. It is a highly beneficial surgery as it has fewer side effects than regular chemotherapy and destroys cancer cells that can’t be reached surgically by directly applying heated chemotherapy in the abdomen.
Conducted by our multidisciplinary team of physicians, the first step is to surgically remove all the visible cancerous tumors and the second is killing the residual cancerous cells by administering high doses of heated chemotherapy inside the abdomen.
When Is Ulcerative Colitis Surgery Needed
Your doctor may suggest surgery if you can’t control inflammation and ulcers with medication or other treatments. You may also need an operation if you get emergency complications of ulcerative colitis such as severe bleeding or tears in the colon. Some people choose to have surgery if their symptoms affect their ability to work and stay active.
Don’t Miss: Is Fiber Good For Ulcerative Colitis
Scheduled And Emergency Uc Surgery
Most UC surgery can be arranged at time that’s convenient for you. Try scheduling it while your symptoms are calm to cut the chances of complications.
The risks are higher when you have emergency surgery. You may need it if you get toxic megacolon — a life-threatening condition when your colon rapidly swells and gas and bacteria build up inside. Get medical help right away if you have fever, belly pain, constipation, or swelling.
Surgery To Cure Uc Cut Colon Cancer Risk
The only way to cure ulcerative colitis is to get surgery to remove the diseased colon and rectum. You may also choose an operation if you want to cut your risk of colon cancer. Your chances of getting colon cancer go up if you have ulcerative colitis for 8 years or more or have a lot of colon damage. Your doctor may also suggest surgery if they find abnormal growth during a checkup.
Read Also: Low Fodmap Diet Ulcerative Colitis
What To Expect After J
Your body will need time to adapt to the pouch after your surgery. We can help you learn what to expect after surgery and questions you may want to ask your healthcare providers.
-
Some patients may experience an increased number of bowel movements, sometimes up to 12 times per day. This will typically decrease over time.
-
Some male patients may experience sexual dysfunction as a result of nerve damage.
-
Some female patients may develop scar tissue that surrounds their ovaries and fallopian tubes, which may lead to infertility.
-
Both men and women should discuss sexual function with their surgeon and ask when it is safe to resume sexual activity.
-
Ask your healthcare providers what supplies you may need at home, especially if you will have a temporary ileostomy.
-
Your healthcare team will advise you on how to manage your temporary ostomy and how to keep it clean.
Sudden Severe Ulcerative Colitis
This complication is the main cause of emergency surgery in patients with ulcerative colitis. With sudden, severe ulcerative colitis, medications and intravenous steroids, are unable to control the symptoms.
-
Uncontrolled bleeding can occur from deep ulcerations in the colon, though that is rare.
-
Severe, sudden ulcerative colitis can lead to toxic megacolon, a potentially life-threatening complication caused by severe inflammation.
-
Toxic megacolon leads to rapid enlargement of the colon. Symptoms include pain, distension or swelling of the abdomen, fever, rapid heart rate, constipation, and dehydration.
-
Toxic megacolon requires immediate treatment and surgery.
Don’t Miss: Can Ibuprofen Help Ulcerative Colitis
A Messy Part Of Having Ulcerative Colitis
When I had a diseased colon, bowel movements were always a very messy business. Little did I know, j-pouches are ten times worse. I can clean the toilet and by the time my next bowel movement is over, it looks as though I never cleaned it at all.
This is very bothersome for meespecially when Im visiting someone elses house. Not everyone keeps a toilet brush in plain sight, so what you might consider doing is investing in one of those toilet brushes with a disposable head. It may be somewhat of a hassle, but at the end of the day, I feel it is only polite for me to clean up the mess my j-pouch made.
What You Should Know About J
-
This surgical procedure can be performed in up to three stages, but is usually done in two.
-
A temporary ileostomy is typically created to give your newly formed pouch a chance to heal. A loop of your small intestine will be pulled through an opening in your abdomen, called a stoma, to allow waste to exit your body into an ostomy bag.
-
During this time, you will need to wear an ostomy bag at all times and it will need to be emptied several times a day.
-
You will have your second surgery eight to 12 weeks later, once the pouch has healed.
-
A three-stage procedure may be recommended for patients who are in poor physical health, on high doses of steroids, or if they are required to undergo emergency surgery to repair bleeding or toxic megacolon.
Also Check: Whipworm Therapy For Ulcerative Colitis
Adaptation Of Ipaa Surgery In The United States
In the United States, Australian born colorectal surgeon Dr. Victor Warren Fazio was a driving force behind the procedure’s adaptation into American colorectal surgery offerings. He established the Cleveland Clinic‘s prestigious pouch practice in 1983 when the clinic performed its first pouch surgery. In 2002 the Cleveland Clinic opened the world’s first pouch center with its “Ileal Pouch Center”.
About the same time as the Cleveland Clinic began offering the restorative proctocolectomy procedure , surgeons at the Mayo Clinic in Minnesota also started offering it to suitable patients including Dr. Roger R. Dozois who published several early studies on the pouch operation in the United States.
What Can I Expect After J
Even though J-pouch surgery is a major procedure, most men and women begin seeing results quickly. At first, you will have many bowel movements a day, but youll have control over them and can make it to the bathroom in time.
Additionally, the urgent need for a bowel movement thats usually seen with ulcerative colitis also resolves immediately.
After several months, your J-pouch begins functioning more like a rectum, and your daily bowel movements reduce to between four and six occurrences.
Possible complications of J-pouch surgery include:
- Inflammation of the J-pouch, or pouchitis
- Paralytic ileus, or irregular intestine function
You May Like: What Vitamins Are Good For Ulcerative Colitis
Exercising At Your Own Pace May Help
Working out might be the last thing on your mind after J-pouch surgery, but early mobilization is key, says Tarik Kirat, M.D., associate professor of surgery and colorectal surgeon at NYU Langones Inflammatory Bowel Disease Center in New York City. In other words: Get moving. Its sensible to avoid strenuous activities for the first four to six weeks after J-pouch surgery . Your doctor will be able to advise you on what to do and whenit will largely depend on how active you were before the operation. Gentle walking and swimming are good options in the early stages of recovery, Dr. Kirat adds.
Comparison Of Outcomes After J
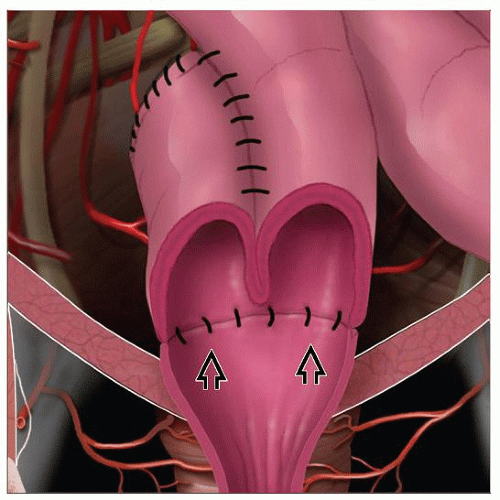
A J-pouch is the preferred ileal pouch type because it is quicker to construct. An S-pouch and a W-pouch need a hand-sewing hence, they are more time consuming. In our institution, our preference is a J-pouch. An S-pouch is used when a J-pouch will not reach into the pelvis without excessive tension in the small bowel mesentery.
A recent meta-analysis12 including 18 studies reported 1519 patients with a J-, S-, or W-pouch. Among the 3 types of pouches, there were no significant differences in postoperative complications including leak, stricture, pelvic sepsis, pouchitis, small bowel obstruction, and pouch failure. In terms of functional outcomes, bowel frequency was higher in J-pouch patients than in those with either an S- or W-pouch. In addition, the use of antidiarrheal medication was greater following a J-pouch creation compared with either an S- or a W-pouch. However, those patients with an S- or W-pouch had more difficulty in pouch evacuation, which required intubation, than did patients with a J-pouch. Seepage and incontinence were similar among the 3 types of pouch design. In conclusion, the meta-analysis showed an advantage for the J and W over the S design with respect to spontaneous evacuation, despite the higher bowel frequency with the J-pouch compared with the S- and W-pouch. However, the occurrence of complications among the 3 types of pouches was comparable.
Read Also: What Type Of Disease Is Ulcerative Colitis
Colorectal Surgeon Located In Los Angeles Ca
If youre suffering from serious gastrointestinal issues like ulcerative colitis or familial adenomatous polyposis, J-pouch surgery could provide relief. Karen Zaghiyan, MD, FACS, FASCRS, is an experienced double board-certified colorectal surgeon offering the most advanced techniques available at her practice in Los Angeles, California. To see if J-pouch surgery can help your digestive disorder, call Karen Zaghiyan MD or schedule an appointment online today.
Talking To People Who Have Been Through J
The only people who can give you a true idea of what going through J-pouch surgery is really like are people who have been through it themselves. Dr. Remzi advises connecting with other patients, preferably ones who went to the same surgeon, to get a feel for what to expect from the surgery and to make sure you feel comfortable with your medical team.
In addition to offering practical advice, talking to others can be emotionally comforting, says Kimberly Hooks, 37. When Hooks had a three-stage J-pouch procedure between spring and fall of 2020, connecting with others who had the operation made her feel less alone.
I found a lot of support through community, through social media, by joining different Facebook groups and following different hashtags on Instagram. It helped me knowing there were people out there that could relate to me, she tells SELF. Hooks now uses her own account to talk about her experience and connect with other people. There have been so many people that have helped me and they don’t even know it, just by sharing their story. I’m trying to do the same and help the next person.
Recommended Reading: How Do You Treat An Ulcer Naturally
Are There Any Risks Or Complications To Be Aware Of
Despite the potential benefits, the J-pouch procedure is still considered major surgery. As with any major surgery, you may be at risk for infections, bleeding, and side effects from general anesthesia.
Sometimes its possible for the newly formed J-pouch to become infected. However, such risks are higher in one-stage procedures.
Other potential complications from this procedure include:
Overall, the outlook for J-pouch surgery is positive, with few people experiencing pouch failure.
However, one study published in 2015 reported a J-pouch failure rate of between 3.5 and 15 percent. Pouch failures have also been found to be more common in men than women.
If you do develop pouch failure, your doctor may recommend either an ostomy or another type of colorectal procedure called a K-pouch surgery.
Pouchitis is the most common problem following J-pouch surgery and other pouch surgeries. This is a treatable condition and does not necessarily mean youll develop pouch failure. However, chronic pouchitis has been linked to possible failure of the J-pouch.
Systemic Or Metabolic Disorders
- examples: malnutrition, anemia, vitamin B12 and vitamin D deficiency, low potassium
Removal of the entire large intestine and amounts of the terminal ileum at the end of the small intestine leads to fluid and nutritional absorption issues for all pouches. The colon absorbs water and salts. Dehydration can occur if a person does not get enough fluids. When the pouch is constructed small amounts of ileum are lost to the stomas and any stoma revisions. The pouch itself is also made from ileum. If a pouch is defunctioned the person also loses this extra amount of ileum when the pouch is disconnected from the digestive tract. The importance of ileum is that it absorbs key vitamins and minerals including B12 and magnesium.
Recommended Reading: What Can I Take For Mouth Ulcers
Can We Predict Who Might Have Crohn’s Disease
There is no consensus on exactly how to identify patients diagnosed with ulcerative colitis that may later be discovered to actually have Crohn’s disease. There is at least one study, however, that patients who were diagnosed with ulcerative colitis at a young age and also had extraintestinal complications were more likely to have a diagnosis change to Crohn’s disease after j-pouch surgery. Pouch “failure” and eventually having the j-pouch removed are fairly common in patients ultimately diagnosed with Crohn’s disease. However, for those who are able to keep their pouch and find that it functions well for them, there doesn’t seem to be a difference in their quality of life and the quality of life for those who had IPAA surgery and have confirmed ulcerative colitis.
One Step And Three Step Procedures
Occasionally, a surgeon and patient will decide to complete the entire procedure in one step. The surgeon will perform the colectomy, create the j-pouch and connect it all in one operation. The one step eliminates the need for a second or third surgery or a temporary ileostomy. In recent years the practice of doing this surgery all in one step has come into question because there may be a greater risk of pouch-related complications.
If a patient is very ill, the surgeon may elect to use three steps to complete the procedure. In the first step, the colectomy is done, and the temporary ileostomy is created. In the second step, the j-pouch is constructed, and the third step is the takedown. The wait between each of these surgeries is two to three months, depending on the health of the patient. The intervals may be longer for patients who were quite ill at the time of the colectomy. While three surgeries is a major investment, there is some evidence emerging that three surgeries may be associated with a lower risk of complications in the long run.
Also Check: How To Stop Ulcer Pain Instantly
Ordering Ostomy Bags Before Your Operation Is Useful
There are many types of ostomy bags, and your ostomy care nurse can also help you determine the best one for you based on your body type, daily activities, and personal preferences, according to UChicago Medicine. Once youve decided on the type of ostomy bag you want, it can help to order them prior to your operation, says Jess Mazelis, 29, who had her surgery three years ago. Get as many samples as you can before your surgery, and have them ready to go, Mazelis tells SELF. The last thing you want to deal with when youre recovering is talking to medical suppliers. You want to make everything as easy as possible on you, because you’re not going to want to think about anything except recovering once you get home, Mazelis says.
How Does The J
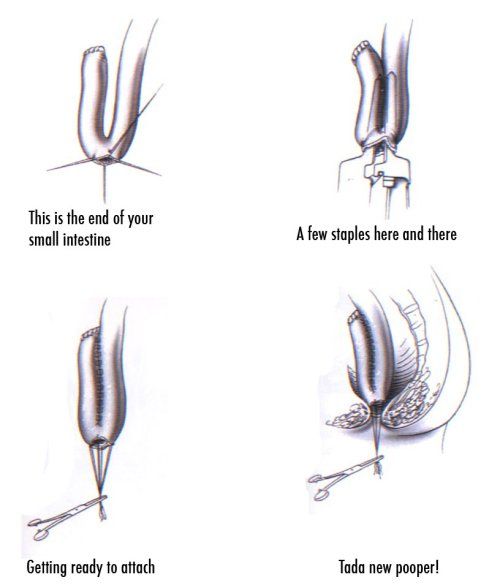
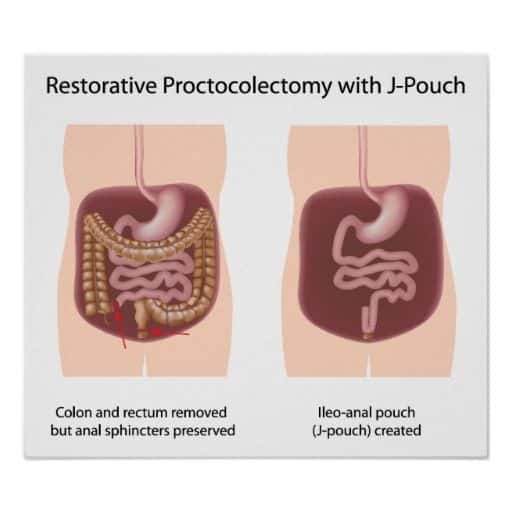
The small intestine has three parts: the duodenum, the jejunum, and the ileum. To create a J-pouch, the end section of the ileum is looped into a J-shape to create a pouch.
UC is a type of inflammatory bowel disease . It affects the large intestine and rectum. Any surgery that removes these parts is considered a cure for UC.
After the colon and rectum are removed, J-pouch surgery creates a new rectum.
You May Like: How To Lose Weight With Ulcerative Colitis
It Can Help To Meet Your Ostomy Care Nurse Before Your Operations
You may want to ask your doctor whether you can meet your enterstomal therapist, who can help you get comfortable using these bags, says Cristal Steuer, 39, who had her surgery in 2011. Enterstomal therapists are nurses who specialize in ostomy care, and some hospitals like the UNC School of Medicine allow you to meet with your nurse before your operation. Scheduling time with your nurse before your surgery can help you get more comfortable using the ostomy bags . And after the surgery, your doctor might not be as responsive as youd like, Steuer explains. When she was having issues with her ostomy, she would call the nurse and get a reply faster than if she tried to reach a doctor. I used to get terrible rashes around where you would stick the bag on. The ostomy care nurse would give me tips to fix that, or if something wasnt working or if I had symptoms, I could find out if it was worth coming into the hospital, she tells SELF. The ostomy nurses were readily available and were very supportive. They deserve a lot of praise.