In What Cases Should I Check With My Doctor Before Taking Nsaids
If you have any of the following conditions or circumstances please check with your doctor before you take NSAIDs:
- Children and teenagers with viral infections should not receive aspirin or aspirin-containing products due to the risk of Reye’s syndrome .
- Those who have an upcoming surgical procedure, including dental surgery.
- People who have three or more alcoholic beverages per day.
- Asthma that gets worse when taking aspirin.
- If you are 65 years of age or older.
Disease states
- History of stroke or heart attack.
Allergic and drug interactions
- Known allergies to medications, especially aspirin, other NSAIDs and sulfa drugs.
- Please check with your pharmacist or healthcare provider before starting an NSAID to determine if your current medications, both prescription and OTC, and also your dietary/herbal supplements, are compatible with the NSAID. Do this especially if you are on warfarin , clopidogrel , corticosteroids , phenytoin , cyclosporine , probenecid and lithium .
- If you take diuretics to control your blood pressure, you may be at greater risk of kidney problems if you take an NSAID.
- Phenylketonuria . Some nonprescription NSAIDs are sweetened with aspartame, a source of phenylalanine.
Common Questions About Mesalazine
No one knows exactly how mesalazine works. It is thought to act on the inflamed lining of the gut by stopping the body producing chemicals that cause inflammation.
Mesalazine helps by reducing the redness and swelling in your intestine. This improves your symptoms.
Mesalazine has a similar effect to immunosuppressants. It can reduce the numbers of white cells in your blood, reducing your body’s ability to fight infection.
Mesalazine does not work straight away.
Depending on how bad your symptoms are, it may take from a few hours to a few weeks for them to start improving.
It may take up to a few months for your symptoms to be completely treated if they are severe.
Mesalazine can be used at a higher dose for a short time to treat flare-ups.
You can also take it long term to keep inflammation under control and prevent symptoms from flaring up again. How long you use it for will depend on how bad your condition is.
Do not stop using mesalazine unless your doctor tells you to.
Different brands and forms of mesalazine work on different parts of your gut. Your doctor will prescribe the brand that releases mesalazine in the part of your gut that needs it most.
You will usually stay on the same brand and type of mesalazine if it’s working to control your symptoms. However, if it does not help your symptoms, your doctor may try you on a different one.
If you are thinking of stopping mesalazine, discuss this with your doctor first as your symptoms may come back.
Ankylosing Spondylitis And Ulcerative Colitis
When bone fusion occurs, axial spondyloarthritis progresses into ankylosing spondylitis. AS is a specific type of axial arthritis that causes inflammatory back pain and limits range of motion. If a person has AS that causes significant fusing in their vertebral column and affects their rib movement, they may also struggle to take deep breaths.
According to the University of Washington, ankylosing spondylitis symptoms generally dont present alongside gastrointestinal symptoms in people with UC. Although doctors arent entirely sure what causes AS, some research suggests a genetic component contributes to the diseases development. Bowel or urinary tract infections are also believed to trigger the onset of AS in genetically susceptible people.
Also Check: Chinese Medicine For Ulcerative Colitis
Be Diligent And Careful With Medication
A physician will usually prescribe an anti-inflammatory and medication to help with an overactive immune system with a diagnosis of ulcerative colitis. This medication is vital to fight off flare-ups and missing a dose can be a trigger all by itself.
When taking medication for this condition, it is always wise to consult a doctor. Certain over-the-counter medications, like NSAIDs, can exacerbate ulcerative colitis as well as cause other issues.
Read Also: How Do You Treat A Peptic Ulcer
What Uc Abdominal Pain Feels Like
Youre certainly not alone if you are experiencing gut . More than half of people with UC report abdominal discomfort, according to a recent report in the Journal of Crohns and Colitis. UC pain is no joke, confirms Jonathan Cruz, a Spanish teacher and actor in Leander, TX, who lives with ulcerative colitis. Cruz describes the pain as something fresh from a horror film. For the most part, average stomachaches are manageable because most over-the-counter medications can control the symptoms, he says. Meanwhile, ulcerative colitis pain is like in the movies when a person is being tortured until the pain makes the victim surrender.
Cruz says one of the hardest aspects of UC pain is the mental anguish that often goes hand in hand. UC pain can go beyond physical pain because it can also impact your mental wellbeing, preventing you from thinking clearly, he says. Whats more, ulcerative colitis pain usually lasts longer than your average stomachache. Oftentimes a non-UC stomachache will last a couple of hours, Cruz says. But abdominal pain associated with UC can become worse throughout the day and continue into the next day and night.
Don’t Miss: Ozanimod Mechanism Of Action Ulcerative Colitis
Radiation Colitis And Enteritis
Inflammation of both the colon and the small intestine can be caused by radiation exposure, most commonly from cancer radiation therapy. However, medical procedures such as X-rays or CT scans can also irritate the colon tissues. Radiation colitis is usually temporary and is marked by diarrhea, cramping, nausea, and vomiting. Symptoms are temporary and usually fade in a few weeks. However, chronic radiation colitis can occur months to years following radiation therapy due to radiation damage. It is a progressive and serious complication of radiation therapy.
Set A Daily Or Weekly Goal
Goal-setting is a great way to distract yourself from the discomfort caused by UC. Youre engaging the brain, says Dr. Szigethy, and in the process also shifting any pain you might feel to the back of your mind. The doctor recommends any goal that involves physical activity: a daily walk or a 15-minute yoga flow are two great options. Youll feel good that youre doing something to improve your health, she says. Plus, exercise is a proven stress-reducer, which can help alleviate symptoms of UC, too. Make sure you regularly update your goals, she suggests, noting how the brain responds well to novelty.
Also Check: How To Treat Pressure Ulcers On Buttocks
Follow A Recommended Corticosteroid Dose
Corticosteroids are common treatments for UC flare-ups. It is important that a person follows their exact dosage over time.
Doctors may prescribe a higher dose that reduces gradually over time.
This is because if a person takes too much of a corticosteroid over a long period, it can put them at a greater risk of a number of problems, including heart problems and mood disorders.
It is important that a person gradually tapers off their use of corticosteroids. This is because instantly or rapidly stopping the course may harm their body.
Bottom Line On Uc Pain Relief
You may be battling UC pain today but that by no means predicts your future. Complete remission should be a shared goal between you and your doctor. It may take patience to find the best treatment but living your life without UC pain is an achievable goal.
Pain Prevalence:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Over the Counter Medications: Mayo Clinic. Ulcerative Colitis.
How Imodium Works: Imodium. How IMODIUM Products Work.
How Tylenol Works: Tylenol. What Is Acetaminophen?
NSAIDs: Therapeutic Advances in Gastroenterology. Pain Management in Patients With Inflammatory Bowel Disease: Insights for the Clinician.
Prescription Medications:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Read Also: Drinking Alcohol With Ulcerative Colitis
What Pain Relief Medicines Are Used In Inflammatory Bowel Disease
There are a variety of pain relief medicines available which can help to control pain in Crohns disease and ulcerative colitis.
Paracetamol
Paracetamol is a commonly used over-the-counter painkiller you can buy without a prescription. It can be used to help with mild to moderate pain, and can also help to control a high temperature. Paracetamol can be used by adults and children and is available in a variety of forms, including:
- Tablets, capsules and caplets
- Oral suspension
Paracetamol works by blocking the production of chemicals in your body called prostaglandins, making your body less aware of any pain. It also reduces your temperature by acting on the part of your brain responsible for controlling it.
Paracetamol is often combined with other medicines, including other types of painkillers. Always check any additional medicines are also safe for you to use.
It is generally considered safe to take paracetamol if you have inflammatory bowel disease, however if you need to take paracetamol for longer than three days, or have a new pain, you should speak to your IBD team.
Two paracetamol tablets every four hours, up to four times a day is considered a safe dose for adults. Side effects are uncommon with paracetamol.
You should read the patient information leaflet in your medicine packet to check if paracetamol is suitable for you. Do not take more than the maximum dose in a 24 hour period as an overdose of paracetamol can be very dangerous.
How To Manage Ulcerative Colitis Pain
Learning effective pain management strategies is a crucial aspect of living well with ulcerative colitis , a form of inflammatory bowel disease . Flare-ups can happen, even if you carefully manage your condition. Swelling of the intestine may cause bloating and painful cramping. You may experience bleeding due to skin irritation from persistent diarrhea.
During a flare-up, it’s not unusual to feel unwell all over. Fatigue, nausea, fever, and anxiety are common symptoms with UC. Progression of the disease can produce joint pain, skin rashes, mouth sores, andeven make your eyes hurt.
UC pain can significantly impact quality of life. One MyCrohnsAndColitisTeam member wrote, Pain in my gut . So tired of being in pain. Another member posted, Woke up with the worst back pain I could ever imagine. I was in tears.
Fortunately, it’s possible to manage the pain associated with UC using a combination of at-home remedies, medical interventions, lifestyle changes, and alternative treatments.
Recommended Reading: The Maker’s Diet Ulcerative Colitis
Extraintestinal Manifestations And Complications
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
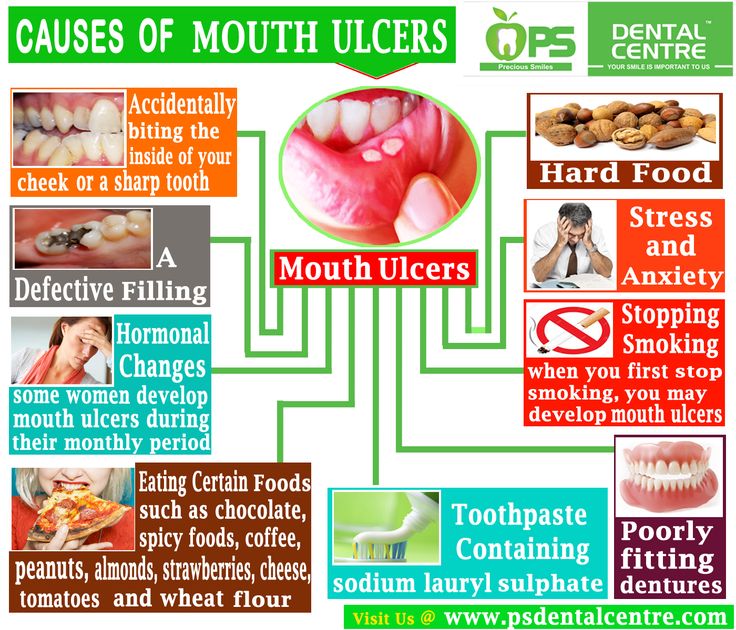
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes. Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Uveitis and iritis are more commonly associated with ulcerative colitis, whereas episcleritis is more commonly associated with Crohn’s disease.
When To See A Doctor
Bleeding from the rectum or blood in or on the stool is never normal. It should always be brought up to a doctor. However, its not always an urgent situation.
If the cause of the bleeding is from a chronic condition , it should be discussed with your gastroenterologist.
In the case of new bleeding, see a doctor as soon as possible. Rectal bleeding that wont stop is a reason to go to the emergency department. Additionally, if you feel faint from blood loss, get to the emergency department right away or call an ambulance.
Abdominal pain can come and go with ongoing conditions, like Crohns disease or ulcerative colitis. Its important to discuss pain at doctors visits. However, if abdominal pain comes on suddenly and is severe, you should go to the emergency room or see a doctor right away.
In infants, caregivers will want to take the baby to see a pediatrician as soon as possible after seeing blood in the stool or around the rectum. Allergic colitis may be a common reason for bleeding, but its important to have a doctor check it out to make sure theres not a more serious reason.
Read Also: Aloe Vera Gel For Horses Ulcers
What Can A Uc Patient Take
If a UC patient is experiencing mild pain from symptoms, experts agree that Tylenol or generic acetaminophen is generally safe to use. Likewise, OTC medications used to treat temporary diarrhea are also considered safe to consume. However, always speak with a doctor before taking any new OTC medications to confirm that there arent any contraindications with prescription medications that could create unwanted side effects.
How Do Nsaids Work
NSAIDs block the production of certain body chemicals that cause inflammation. NSAIDs are good at treating pain caused by slow tissue damage, such as arthritis pain. NSAIDs also work well fighting back pain, menstrual cramps and headaches.
NSAIDs work like corticosteroids , without many of the side effects of steroids. Steroids are man-made drugs that are similar to cortisone, a naturally-occurring hormone. Like cortisone, NSAIDs reduce pain and inflammation that often come with joint and muscle diseases and injuries.
Read Also: Ulcers On Legs From Diabetes
The Best Exercises To Try If You Have Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that causes inflammation and ulcers in the digestive tract. According to experts at the Cleveland Clinic, ulcerative colitis mostly affects the lining of the large intestine, as well as the rectum. While anyone can get ulcerative colitis at any age, it is most likely to affect people between the ages of 15 and 30 or those who have a close relative with the disease.
However, not everyone with ulcerative colitis will experience it the same way. That’s because the disease can range in severity. As a matter of fact, half of those diagnosed with ulcerative colitis will experience mild symptoms, like nausea, fatigue, anemia, stomach pains, diarrhea, and weight loss, while the other half will experience more severe symptoms, like frequent fevers, bloody diarrhea, severe cramping, joint pain, mouth sores, and loss of fluids and nutrients. That’s why it’s important to get diagnosed and seek treatment if you experience any combination of these symptoms.
Deal With Iron Deficiencies Too
UCs painful, even gut-wrenching symptoms dont always make it fun to eat. And, people with this chronic condition may lose blood in their stool, as well as absorb dietary iron poorly due to inflammation, according to the Cleveland Clinic. Additionally, foods rich in iron, like red meat, often trigger flareups. Together, this can cause anemia, a condition characterized by a low red blood cell count. Its a common issue with the UC communityand must be controlled to battle fatigue. If you have UC and super-low energy, talk to your doctor about iron supplements.
Don’t Miss: Antibiotics For Leg Ulcer Infection
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Ulcerative Colitis Risk Factors
Anyone can develop ulcerative colitis. UC onsets are most common between ages 15-30 but can occur any time, and gender doesnt appear to be a factor in risk level . Despite UC lacking a target market, there are certain factors that make some lower intestines more at risk from UC than others.
- Smoking. Smoking = bad for you. You can add Ulcerative Colitis to the list of conditions it increases your risk of developing.
- Alcohol. Theres some evidence that prolonged/excess alcohol consumption might increase risk of IBDs. More research is needed into UC specifically, but if proved true would track with alcohols habit of being linked to health problems.
- Environmental Pollutants. Pollutants and toxins in the environment, such as air pollution or chemicals in some water supplies, increase UC risk. Research has shown this time and time again.
- Hereditary Risks. Probably the highest risk with UC is having close family members with UC. Genetics determine autoimmune response, gut bacteria, how we process alcohol and toxins basically everything else thats a UC risk/causal factor. If your family member has a UC-making DNA helix your chances of doing so too are, for obvious reasons, higher.
Dont Miss: Ulcerative Colitis Abdominal Pain Relief
Don’t Miss: Symptoms Of Crohn’s And Ulcerative Colitis