Eat And Drink With Caution
If youre traveling to many places outside the United States, Chachu highly recommends drinking only bottled water and ice made from bottled water. I even recommend using bottled water for brushing your teeth and washing fruits and vegetables, she says. Unclean tap water can trigger diarrhea, which can then trigger a major flare.
Also, prior to dining somewhere, inquire about how the food is prepped and cooked as well as what menu options are available. I find that most restaurants are very accommodating when it comes to food sensitivities and allergies, says Chachu.
Study Design And Participants
In the present cross-sectional study, the diet adequacy and food avoidance habits of UC patients in the UK were investigated. The study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the ethics committee of a UK Higher Education Institution. Written informed consent was obtained from all participants.
A total of ninety-seven UC patients were recruited across the UK from the National Association for Colitis and Crohns Disease registers by e-mail, posts in UC forums and social media sites. The inclusion criteria were as follows: aged 1865 years and no history of UC-related surgery.
Initially, four participants participated in a pilot study to ensure that the questionnaire and 24 h dietary recalls were readable and not distressing.
Popular Diet Plans With Patients
The Paleo Diet is another popular diet amongst patients with IBD. It recommends avoidance of processed food, refined sugars, legumes, dairy, grains and cereals, and instead it advocates for grass-fed meat, wild fish, fruit, vegetables, nuts and healthy saturated fat . While it makes sense that a diet that promotes avoidance of refined and extra sugars and processed energy dense food would have health effects, there are no clinical trials that have examined the efficacy of this diet for IBD. Randomized controlled studies are required to determine whether the Paleo diet has beneficial effects over other diet advice.
Don’t Miss: What Type Of Disease Is Ulcerative Colitis
Pita Chips And Hummus
Hummus is made with mashed chickpeas, olive oil, and other seasonings.
The Crohns and Colitis Foundation recommend 1/4 cup of hummus and 2 ounces of pita chips as a snack.
To make hummus at home, a person can blend chickpeas, tahini, and a little olive oil together. They can add seasoning to taste but should avoid adding too much salt.
Even though it is high in fiber, pita chips and hummus can be a generally well-tolerated snack or small meal. The chickpeas in hummus may help symptoms in a person experiencing gas or bloating.
How To Identify Your Trigger Foods
Theres no way around this one: Youve got to track everything you eat and what, if any, symptoms result. Even if you work with an R.D. , this will be an important part of that process. For example, maybe you realize that every time you eat dairy, diarrhea follows a few hours later. Or maybe a night of drinking really sparked a flare-up. Watch for patterns like this and make note. And dont forget to take your food diary with you to your doctors appointmentsit can be a useful tool to help you and your health care team figure out how best to manage your UC. You can go the old-fashioned route and use a paper format or try an app like GI Monitor.
When youre planning your meals, forget about sticking to three squares. Eating large portions can overwhelm your already-sensitive digestive system. Instead, aim for smaller portions spread throughout the day instead of a few big meals. Downing your food too fast can also lead to discomfort, so eat slowly and mindfully and really concentrate on chewing your food thoroughlythat gives your gut a little extra help!
Also Check: Is Cottage Cheese Good For Ulcerative Colitis
Find Your Support System
MyCrohnsAndColitisTeam is a community of more than 138,000 members who understand living with inflammatory bowel disease. Members share tips for managing flares and offer each other support and encouragement.
Do you struggle with UC flares? What has worked for you? Share your tips in the comments below, or on MyCrohnsAndColitisTeam.
How Can I Live With Chronic Ulcerative Colitis
If you are struggling with colitis or another type of irritable bowel disease, help is available at Gastroenterology Associates of Southwest Florida, PA. Our team provides compassionate, expert care to help patients suffering from these types of chronic conditions. Find out how we can help you live with chronic ulcerative colitis
You May Like: Cbd Oil For Stomach Ulcers
You May Like: What Are Infusions For Ulcerative Colitis
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Monosaccharides
Because of their poor digestion, FODMAPs can cause gastrointestinal issues in some people7. Research suggests an improvement in IBD symptoms in some patients who follow a low FODMAP diet, but there is no evidence of improved inflammation8.
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
Although some very small studies see the benefits of this style of eating, more research is needed10.
Also Check: What Is An Ulcer Diet
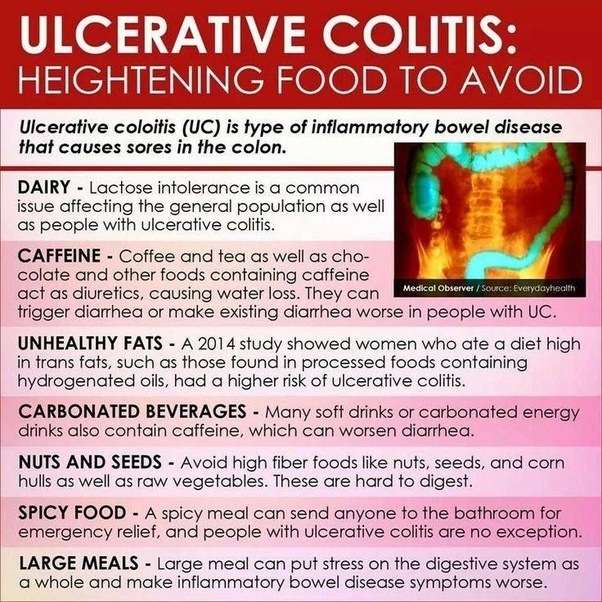
Vegetables To Avoid With Ulcerative Colitis
When it comes to veggies that can potentially trigger your symptoms or make them worse, cruciferous vegetables, such as broccoli, cauliflower, Brussels sprouts, and cabbage, are often at the top of the list. Theyre common triggers for gas and bloating, regardless of whether they are raw or cooked, Leben says. Depending on how they affect you, you may find that you need to steer clear during flares or cut them out of your diet completely.
Be careful with large amounts of tough, uncooked greens, too, such as kale salads. While leafy greens that have been cooked until soft may be tolerable for some, the rough texture of the raw greens can be irritating, Warren notes. But again, this will all depend on the patient, she says.
Salads dont have to be entirely off limits, Warren and Leben say. If you find that raw vegetables work for you when youre not experiencing symptoms, go ahead and enjoy them in quantities you can tolerate.
You May Like: Mouth Ulcer Vitamin B Complex
Give Yourself Some Tlc
Stress doesnt cause UC, but it makes symptoms and flares worse for some people. If it affects you, try meditation, breathing exercises, or a massage. You could also see a pro to try biofeedback, hypnotherapy, or a type of counseling called cognitive behavioral therapy, which helps you learn new ways to handle problems. Being active helps, too. Try yoga, tai chi, or other low-impact exercises like walking.
Also Check: How To Test For Ulcerative Colitis
How Can Diet Help With My Symptoms
Making changes to your diet may help you manage some common symptoms of Crohns and Colitis, such as loose and runny stools, dehydration, bloating, wind, constipation, weight loss, tiredness, nausea and vomiting and pain. While changing your diet can help you manage your symptoms, it doesnt replace the medical treatment suggested by your IBD team.
Loose and runny stools
A common symptom of Crohns and Colitis is loose and runny stools, called diarrhoea. For some people, their diet has no effect on their diarrhoea. Others find that avoiding certain foods helps. You could use the food diary above to help you find out which foods might be causing your symptoms. Foods which sometimes make diarrhoea worse include spicy or fatty foods, high fibre foods, foods containing gluten and dairy foods. Drinks containing caffeine, sweeteners or alcohol can also make diarrhoea worse.Your IBD team or dietitian can advise you on how to manage your diarrhoea. They will want to make sure youre eating and drinking enough to get all the nutrients you need and to stay hydrated. In some cases, they may recommend medicines to help.Our guide Diarrhoea and constipation has more information about what causes diarrhoea and possible treatments.
Dehydration
If your body doesnt have enough water, you can become dehydrated. This might happen if you dont drink enough fluids or if your body loses too much fluid, for example, if you have diarrhoea or vomiting.You may be more likely to get dehydrated if:
Recommended Reading: What Is Refractory Ulcerative Colitis
Eating With A Stricture
If you have a stricture , you may need to change what you eat to help prevent the intestine getting blocked.You might be advised to avoid foods that could block the intestine, such as:
If you have a severe stricture, you may only be able to eat very soft or liquid foods.Its important to speak to a dietitian to make sure youre eating a healthy, balanced diet. In some cases, they may recommend a vitamin and mineral supplement.
How Long Do Flare
UC is a condition that is unique to every individual. Some people experience flare-ups that last a few days, while others experience flare-ups that last weeks. Likewise, individuals may go from a mild flare-up to a severe one and then back again.
If a person is experiencing a severe flare-up that persists, they should speak with a doctor. The doctor will help them get their symptoms under control and improve their quality of life.
Read Also: C Diff And Ulcerative Colitis Treatment
Soothe Skin Irritation And Pain
Bouts of diarrhea often can bother your skin. Use moist towelettes for wiping. Follow up with a petroleum jelly ointment. Need more relief? Soak in a saltwater bath, which may ease soreness. Try acetaminophen for pain, but avoid NSAIDs, such as ibuprofen and naproxen. They can trigger flares and cause other problems.
What To Eat To Beat Ulcerative Colitis
If youâre dealing with ulcerative colitis, you donât need anyone to tell you how painful it is. Inflamed walls of the large intestine riddled with raw sores known as ulcers is no oneâs idea of a picnic. Its no wonder that 70% of people suffering from UC, a type of inflammatory bowel disease , have tried elimination diets in an attempt to figure out how to ease the discomfort during flares. In fact, research suggests that the removal of certain foods from your daily repertoire, combined with the addition of beneficial ones, can play a big role in helping combat symptoms.
That approach is likely your best one, since the actual cause of UC remains elusive. âIt is believed that a combination of factors may precipitate the onset, including genes, environmental factors like diet, stress, and smoking, immune system dysfunction, and imbalances in the gut microbiota,â says Ryan Warren, R.D.N. a clinical nutritionist at the Jill Roberts Center for Inflammatory Bowel Disease at Weill Cornell Medicine and New York-Presbyterian. âDiet can play an important role in managing symptoms as well as maintaining adequate nutrition.â Heres what to eat to stay one step ahead of this painful disease.
Recommended Reading: How To Determine Stomach Ulcer
To Drink: Liquid Nutrition
There are a variety of nutritional supplements on the market that can be found in grocery and drug stores. They do tend to be pricey, but they can add much-needed nutrients to the diet during a flare-up. A gastroenterologist can recommend a particular brand and offer advice on how often they should be used. Liquid nutritional supplements shouldnt be used as the sole source of calories, however, as they are only meant to augment the diet until more foods can be added.
Dont Miss: Classic Features Of Ulcerative Colitis
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Read Also: How Do I Treat Mouth Ulcers
Foods To Eat During Ulcerative Colitis Flares
A bland diet is best during periods of active ulcerative colitis, when you may experience abdominal discomfort, blood in your stool, loss of appetite, fatigue, weight loss, vomiting, nausea, abdominal pain, and diarrhea. A safer diet during flares might include dry toast, applesauce, and white rice. Although some foods are more likely to be safe for those with UC, individual experiences can vary, especially during flares.
Here are some safer foods to try during ulcerative colitis flares:
- Low-fiber refined grains, such as oatmeal, potatoes, and sourdough bread
- Well-cooked vegetables that are easier to digest
- Vegetable broth, which can be added to grains like rice for additional nutrients
- Fruits or vegetables that contain more soluble fiber than insoluble fiber, such as bananas, carrots, and apples
- Bland protein, such as nut butters, eggs, tofu, and chicken
Diarrhea specifically raises concerns for loss of nutrients, such as potassium, sodium, magnesium, and phosphorus, through bodily fluids. If you choose to drink an electrolyte beverage, choose low sugar versions such as G2, Propel, or BodyArmor Lyte. You can also cut regular Gatorade or BodyArmor with water, diluting it by half.
How To Find A Meal Kit That Wont Trigger A Flare
Kennedy tells people with ulcerative colitis to keep a daily food journal to track which foods trigger a flare-up. By narrowing down the foods you can and cant eat, youll have an easier time finding meals that will fit your diet.
Kennedy also recommends checking the nutrition labels for fat content, because too much fat can trigger a flare. You never want one meal to account for 75 percent of your daily fat, for example, she says.
Plus, not all fats are created equal, she says. Meals that contain a lot of fat from cheese or red meat can be difficult to digest for people with UC, she says. For example, fat that comes from salmon, as opposed to steak or butter, is less likely to cause GI issues for people with colitis, she says.
Also Check: Is Peanut Butter Bad For Ulcerative Colitis
Reintroducing Your Usual Diet
Your IBD team and dietitian will give you information about returning to your usual diet after youve finished enteral nutrition. They may suggest reintroducing foods slowly so you can see if any foods affect your symptoms and to help you feel more confident about eating again. There are three ways of doing this:
- the elimination diet – after excluding all foods, they are reintroduced one by one every few days, to see if they cause problems
- the Royal Free method – this is similar to the elimination diet but foods are reintroduced more quickly, over a period of days rather than weeks
- the LOFFLEX diet – this excludes foods high in fat and fibre.
There isnt much evidence to show how well these diets work, or whether one works better than another. Your dietitian will explain the benefits and risks of all your options.
Ive found that you have to be very careful on the internet as there are many websites claiming to cure IBD through untested diets and supplements – which are not properly regulated and could be harmful and also expensive.
Zaineb
This is an extreme form of low carbohydrate diet that limits:
Is Ulcerative Colitis And Autoimmune Condition
We are frequently asked whether Ulcerative Colitis it is an autoimmune condition. The short answer is yes, but its most important to understand what that means for your treatment plan.
With Ulcerative Colitis, the body recognizes harmless gut bacteria as an enemy and attacks the tissues in the colon. In a typical immune response, the body will send white blood cells to the area of illness or infection to help protect the body. After the body has combated the illness or infection, the inflammation will resolve.
However, in a colon affected by UC, the body continues to send white blood cells to the inner layer of the large intestine, which accumulate and continue to attack. This process causes a buildup of inflammation and can lead to sores, or ulcers, in the affected area. Because UC is recognized as an autoimmune condition, the treatment methods generally target the immune response within your body.
Medical Treatments for Ulcerative Colitis include:
Don’t Miss: Alginate Dressings For Treating Pressure Ulcers
Ulcerative Colitis Diet: Foods To Eat And Foods To Avoid
- Keeping a food journal can help you identify foods that trigger ulcerative colitis symptoms.
- Avoiding common trigger foods may help manage symptoms during UC flares.
- Knowing which foods are most nutritious for those with UC and how to safely prepare them can help you eat healthier.
- Working with a registered dietitian can help you get the most nutrients out of the foods you can safely eat.
Ulcerative colitis is an autoimmune condition caused when the immune system attacks the tissues of the digestive tract, specifically the large intestine and rectum. Along with Crohns disease, ulcerative colitis is a type of inflammatory bowel disease. IBD inflammation leads to gastrointestinal symptoms, such as diarrhea, bloating, and cramping, as well as problems with digestion and absorption of nutrients.
No specific foods cause ulcerative colitis, and there is no specific diet that has been proven to cure it. However, each person with UC finds that certain foods can trigger or worsen symptoms, while other foods can be digested safely and comfortably. The foods on each list vary by individual. As one MyCrohnsAndColitisTeam member put it, This disease is not one-size-fits-all, so you will have to experiment to see what works for you and what does not.
The list of foods to avoid and foods to eat with ulcerative colitis may also change depending on whether youre currently experiencing a disease flare or remission .