Role Of Fiber In Crohns Disease:
The fiber in your diet is crucial for maintaining good health. It can assist you in maintaining appropriate levels of weight, blood pressure, and cholesterol. Additionally, consuming 23 grams of fiber every day can reduce your chance of a Crohns flare-up by as much as 40%. The addition of fiber in your diet can increase Crohns disease life expectancy.
Soluble fiber-containing meals are your best bet if you have Crohns disease. In your intestines, soluble fiber absorbs more liquid. Soluble fiber-rich foods can slow down digestion and relieve diarrhea.
Insoluble fiber, the other type of fiber, can increase the amount of water in your gut. Your digestion of meals is rapid. Gas, bloating, or watery diarrhea could result from that. A blockage could result from an excessive amount of insoluble fiber.
Dont Miss: Hind Gut Ulcers In Horses Symptoms
The Impact Of Biological Interventions For Ulcerative Colitis On Health
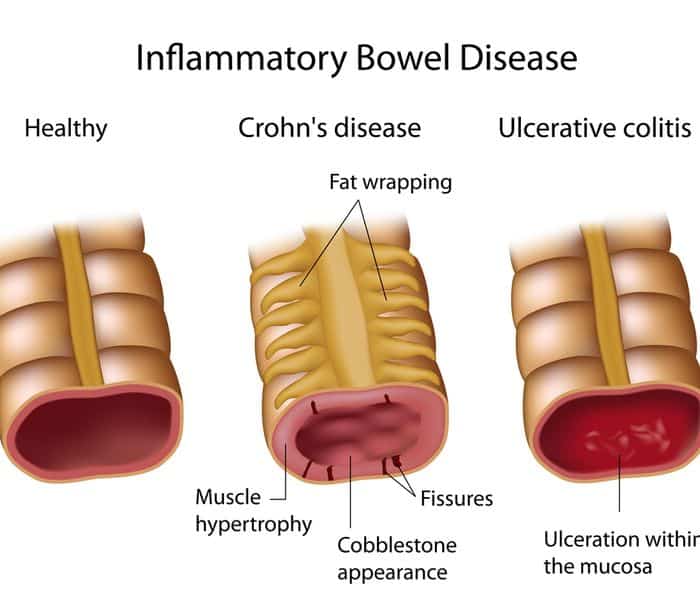
What is ulcerative colitis?
Ulcerative colitis is a chronic inflammatory bowel disease characterized by abdominal pain, urgent bowel movements and bloody diarrhea. Treatment of UC focuses on induction of remission and prevention of clinical relapse in patients in remission . UC has a major impact on patients’ health related quality of life . HRQL refers to a person’s physical functioning, social and emotional well-being, ability to work and freedom from disease symptoms. HRQL is significantly lower in patients with UC compared to the general population. Randomized controlled trials evaluating medical interventions for UC have traditionally used clinical disease activity indices which focus on subjective symptoms to define primary outcomes such as clinical remission or improvement. This focus on disease symptoms results in a failure to assess other important indicators of successful treatment such as HRQL.
What are biological interventions for ulcerative colitis?
Biologics are genetically engineered medications made from living organisms. They work by targeting specific cells in the gut that are involved in the inflammation process.
What did the researchers investigate?
The researchers assessed the impact of biologic medications on HRQL in people with ulcerative colitis. The researchers extensively searched the medical literature up to September 9, 2015.
What did the researchers find?
Symptoms To Look Out For:
Any component of your small or large intestine may be impacted by Crohns disease, and it may be persistent or comprise several segments. Some patients only have the disease in their colon, which is a passage of their big intestine.
The severity of Crohns disease symptoms can vary from minor to severe. It can also impact Crohns disease life expectancy. Though they frequently come on gradually, they can also do so quickly and without warning. Additionally, there may be times when you experience no symptoms or indicators .
Some of the symptoms include:
- Diminished appetite,
Additionally, those with severe Crohns disease might experience:
- Inflammation of the eyes, joints, and skin,
- Inflammation of the bile ducts or liver,
- A deficit in iron , and
- Delayed sexual development or growth in kids.
You May Like: Best Home Remedy For Stomach Ulcer
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
Does Stress Cause Colitis
Although stress can be responsible for triggering a flare-up of symptoms, stress is currently not thought to cause ulcerative colitis. Instead, researchers think stress exacerbates it. The exact cause of ulcerative colitis is unknown, but some people have a greater risk for developing this condition.
You May Like: Can Ulcers Cause Diarrhea After Eating
You May Like: How Do They Check For Ulcers
Proper Supplement And Medication Intake
There are plenty of supplements and medications that can improve your health-adjusted life expectancy and quality of life. Here are some of the important medications and supplements that we suggest you speak to your doctor about if you suffer from IBD:
- Anti-inflammatory drugs: This is typically the first treatment suggested by doctors for inflammatory bowel disease.
- Immune system suppressors: These drugs are supposed to suppress the immune system from releasing inflammation-inducing chemicals.
- Biologics: This is a new type of medication used to treat IBD that is supposed to neutralize inflammation-causing proteins.
- Antibiotics: Antibiotics can sometimes be used to treat IBD, most specifically, Crohn disease.
- Anti-diarrhea medication: This medication is usually taken to reduce the symptom of diarrhea which happens during flare-ups.
- Pain relievers: This medication can be taken to reduce pain symptoms that people experience during flare-ups.
- Vitamins: IBD can cause malnutrition, which can lead to not enough vitamins and nutrients being absorbed by your body.
Differences In Surgery Outcomes
Most people can manage UC symptoms with medication and diet. But those with more severe symptoms may need surgery to remove their colon or their colon and rectum .
Black and Hispanic people with IBD seem to have worse outcomes after surgery than white people do. They need to stay in the hospital longer after surgery, have more complications, and are more likely to return to the hospital later because of post-surgery problems.
A program called Enhanced Recovery After Surgery is helping to improve surgery outcomes for people of all races. ERAS streamlines the process before, during, and after surgery to reduce complications. Research shows that this program equalizes surgical outcomes for people of all races.
Don’t Miss: Best Smoothies For Ulcerative Colitis
Driving Research To Improve Patients Quality Of Life
Inflammatory bowel disease is called an invisible illness for a reason. It can have a debilitating effect on your quality of life while others may not understand or be able to see that you are sick. It doesnt help that many patients are reluctant to speak about their disease. As Mike Weinberg, a patient featured in our recent Impact Report, tells us, Its not a disease you want to talk about, and I suffered in silence.
This is why addressing unmet patient needs is our top priority as we set our research agenda. Last year, we invested $32 million in 200+ research projects, bringing our total investment in research to $446 million over the past five decades.
We are dedicated to finding cures for IBD and were as committed to investing in research designed to address issues that impact IBD patients daily lives, such as chronic pain, diet and nutrition, and the role of stress in IBD. Here are a few examples of research we are leading to help people live better with IBD.
Etrasimod Leads To Improvements In Quality Of Life For Ulcerative Colitis Patients
Patients in the open-label extension of the OASIS study saw increases in Inflammatory Bowel Disease Questionnaire scores.
In data presented at the 2021 American College of Gastroenterology Annual Meeting, investigators found etrasimod 2 mg results in improvements in quality of life for patients with moderate-to-severe ulcerative colitis.
A team, led by Michael V. Chiorean, MD, Swedish Medical Center, examined the effect of etrasimod on quality of life metrics.
You May Like: Can Food Allergies Cause Ulcerative Colitis
Should You Stop Taking Your Ibd Medication
First of all, do not make any changes to your medication regimen without first talking to your doctor.
According to the ACG, keeping IBD well-controlled or in remission may help protect you from contracting COVID-19.
Right now the real hotspots for spread of this infection are in health care settings, says Dr. Ungaro. If your condition is well-controlled and you stop taking your usual medications, you risk having a flare. We do not want patients to have a flare in the midst of this pandemic and end up in the ER where they could be exposed .
If youre using steroids: Topical steroids, which are taken via suppositories or enemas, are unlikely to cause problems. Systemic steroids, however, are another story. If youre on oral steroids, now is a good time to start tapering off them if you can, says Dr. Ungaro, but do not stop taking steroids cold turkey. Call your gastroenterologist, discuss whether it is a good idea for you to start decreasing your dose, and find out how to do so slowly and safely.
If youre using aminosalicylates, biologics, or immunomodulators: If youre doing well on a drug in one of these classes, stick with it, says Dr. Morganstern. If you stop, youre at risk of flaring.
One exception, however, may be for patients who are stable and taking both an immunomodulator and a biologic. If someone is in remission on combination therapy, I might try removing the immunomodulator and keeping the biologic, says Dr. Morganstern.
Dr Donohue: Ulcerative Colitis Should Not Shorten Life
Dear Dr. Donohue My daughter is seriously committed to a youngman who has a good job and whom we very much like. She told us thathe has ulcerative colitis. My husband and I were flabbergasted. Helooks the picture of health.
This information has made my husband and me edgy. We wonder whatkind of future he faces, and if he will be able to support a wifeand family. Can you ease our minds?
I invited them for dinner. Now I wonder what I can serve. Do youhave any suggestions? C.C.
Answer Neither your daughter nor your son-in-law faces athreatening future. His illness doesnt preclude a long, productiveand happy life.
Ulcerative colitis is an illness where the colon lining isstudded with shallow sores, ulcers. Abdominal pain, diarrhea , weight loss and sometimes fever are symptoms of thiscondition when it is active. It isnt always active. It fluctuatesbetween periods of remission and periods of activity. It alsovaries in severity. Your daughters fiance sounds like he has amild case. People with severe and unremitting symptoms are quitethin.
Read Also: How Serious Is A Stomach Ulcer
What Is The Treatment Of Ulcerative Colitis
Ulcerative colitis is a lifelong disease with constant periods of flare-ups and remission . Presently, there is no permanent medical cure for it, but there are various medications that can provide symptomatic relief, reduce inflammation, and manage flare-ups.
Treatment involves medical and surgical management depending on the disease severity. Patients would also require dietary and lifestyle changes.
- Medical treatment includes the following:
- Medication to suppress and/or modulate the immune system
You May Like: How Do You Know If You Have A Stomach Ulcer
What Causes Racial Disparities In Uc
There are a few possible reasons for the disparities in UC outcomes between white people and people of color.
Lack of access to care. UC is a chronic disease that requires long-term treatment to manage symptoms and prevent complications. Having access to a gastroenterologist â a specialist who treats UC â and going for regular follow-up visits is key to having a good outcome.
Studies show Black people are much less likely to see a gastroenterologist or other IBD specialist than white people. Instead, they often get treated in the emergency room after they’ve already developed complications.
Delayed diagnosis. A lack of access to specialists and assumptions in the medical community that UC is a white person’s disease could slow the process of getting a diagnosis for people of color. That may be why they often have disease thatâs progressed or have already developed complications by the time they see a doctor.
No insurance coverage. IBD treatments are effective but expensive. Managing UC can cost around $23,000 a year. Insurance coverage can make the difference between affording treatment and going without. That’s especially true for people of low income, and Black Americans with IBD typically earn less money than the national average.
Outcomes also differ by type of insurance. People with Medicaid are three times more likely to die after UC surgery than those with private insurance. This may be because of longer wait times for surgery.
Show Sources
Read Also: Best Way To Treat Mouth Ulcers
Figuring Out Which Foods Trigger Flare
As the NIDDK explains, although ulcerative colitis isnt caused by diet or nutrition, certain foods can trigger the symptoms or make them worse in some people. The tricky part is figuring out which ones.
Common ulcerative colitis triggers include dairy, high-fiber foods like fruit, vegetables, and whole grains, spicy foods, alcohol, and caffeine, according to the Mayo Clinic. That said, its really individual. Sam has always loved food and says that when it comes to what she can eat now, I have not figured that aspect out. And its not for lack of trying. I feel like Ive done everything! she tells SELF, explaining that she tries to avoid various food groups like dairy that can trigger symptoms. It doesnt mean I dont ever eat them, but I try to avoid them, she says. Im definitely still experimenting.
Stacey Bader Curry, 48, was diagnosed with ulcerative colitis in March 2020 and is concerned about giving up foods she loves, as well as alcohol and coffee. Im trying to focus on what I can eat and not what I cant eat, she says.
To figure out whether certain foods might be triggering your symptoms, the NIDDK recommends keeping a food diary where you record everything you eat and any flare-ups to help you work out what your dietary triggers could be.
Recommended Reading: How To Heal Stomach Ulcers Naturally
How Uc Looks In People Of Different Races
The specific location of your UC inflammation affects the kind of symptoms you have and the treatment you need. Black people are more likely to have inflammation in their rectum or on the left side of their large intestine . People who are of Asian heritage have fewer inflamed areas in their intestines than people of other races do.
IBD doesn’t affect just the GI tract. It also can cause inflammation and complications in other parts of the body. Those complications differ by race, too. For example, Black people are more likely than people of other races to have inflammation in their joints and eyes. Hispanic people have more problems with their skin.
Also Check: Does Stelara Work For Ulcerative Colitis
About Our Health Information
At Bupa we produce a wealth of free health information for you and your family. This is because we believe that trustworthy information is essential in helping you make better decisions about your health and wellbeing.
Our information has been awarded the PIF TICK for trustworthy health information. It also follows the principles of the The Information Standard.
Dont Miss: Can Diet Help Ulcerative Colitis
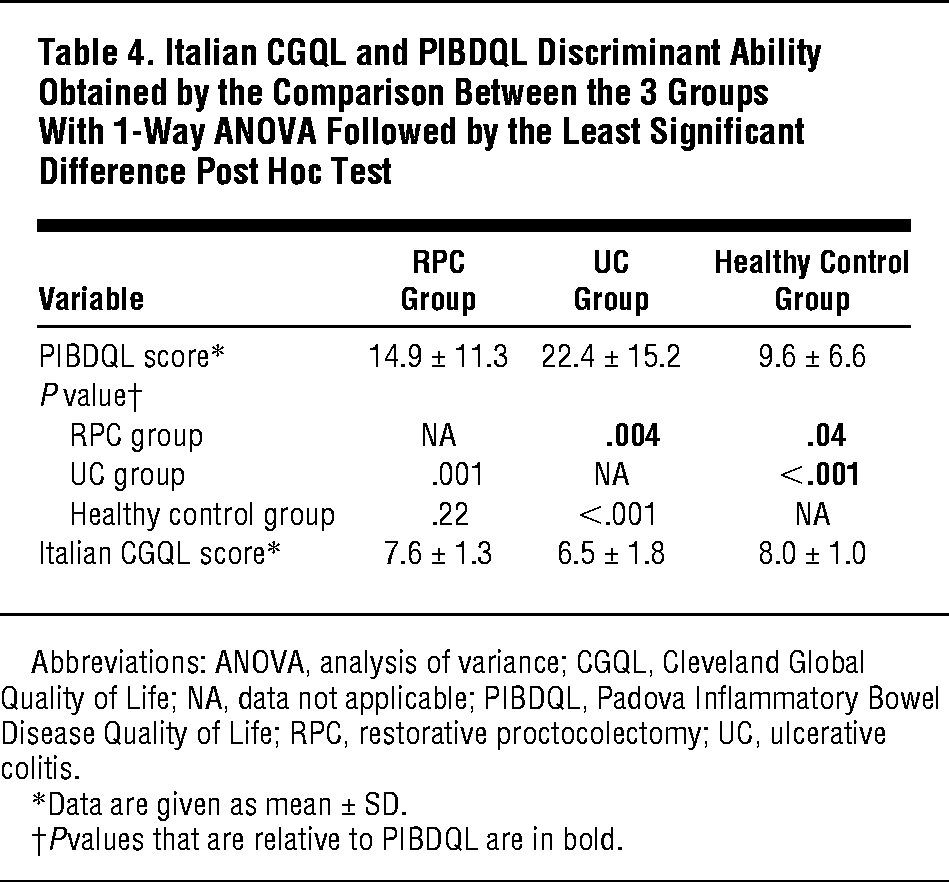
Patient Cohort And Study Design
Patients with new onset of UC were prospectively recruited from two outpatient specialized IBD clinics between 2004 and 2007. The inclusion criteria were adults with newly diagnosed UC. The exclusion criteria were malignancy during the previous 5 years, alcohol or drug abuse and other significant disease, such as severe heart, kidney, neurological or psychiatric disease, that could affect the possibility to comply with the study protocol as judged by the investigators. All included patients were offered prescheduled follow-up visits at the time of diagnosis and 3 months, 1, 2, 3 and 10 years after the inclusion. Only data collected at the 10-year follow-up were used for the purpose of the present study. All patients received verbal and written information, and signed an informed consent form, before any study-related procedures were initiated. Approval of the study protocol was obtained by the Regional Ethical Review Board in Gothenburg prior to the start of patient inclusion . The reporting of this study conforms to the STROBE statement13
Self-assessment questionnaires to measure GI symptom severity, psychological distress , fatigue, and HRQoL were completed by the patients. GI symptom severity was assessed with the Gastrointestinal Symptom Rating Scale ,15 psychological distress with the Hospital Anxiety and Depression scale ,16 fatigue with the Multidimensional Fatigue Inventory ,17 and HRQoL with the Short Form Health Survey .18
You May Like: Is Ulcerative Colitis And Colitis The Same Thing
Study Design And Data Sources
We conducted a matched cohort study comparing trends in life expectancy and health-adjusted life expectancy in people with and without IBD. We included all those with prevalent cases of IBD who were alive on July 1, 1996, 2000, 2008 and 2011. We matched all people with a diagnosis of IBD who were alive on July 1, 1996, 2000, 2008 and 2011, to 5 people without a diagnosis of IBD, based on age, sex, rural or urban residence and mean neighbourhood income quintile at the time of survey or index date for those not participating in a survey. All patients had been diagnosed with IBD at least 6 months before responding to a Statistics Canada survey. We matched people with IBD who responded to a Statistics Canada survey to people without IBD who responded to the same survey and followed them for 5 years from the index date, or until death or migration from Ontario.
We identified prevalent cases of IBD from the Ontario Crohns and Colitis Cohort, derived from health administrative data using validated age-specific algorithms based on encounters in health services and using International Classification of Diseases, 9th Revision codes 555 and 556 , and International Statistical Classification of Diseases and Related Health Problems, 10th Revision codes K50 and K51 .16,17
We classified survey respondents as having IBD if they were contained within the Ontario Crohns and Colitis Cohort.
Colon Cancer And Ulcerative Colitis
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you don’t get treatment for UC. That’s because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if you’ve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesn’t go away.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member who’s had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think it’s because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
Recommended Reading: How To Clean A Diabetic Foot Ulcer