Diseases Of The Skin And Subcutaneous Tissuetype 2 Excludes
- 2016201720182019202020212022Non-Billable/Non-Specific Code
Code First
- Pressure ulcer of left foot stage 4
- Pressure ulcer of left lower leg stage 4
- Pressure ulcer of left toes, stage 4
- Pressure ulcer of lower leg stage 4
- Pressure ulcer of right foot stage 4
- Pressure ulcer of right lower leg stage 4
- Pressure ulcer of right toes, stage 4
- Pressure ulcer of toes stage 4
- Pressure ulcer stage 4 of left lower leg
- Pressure ulcer stage 4 of lower leg
- Pressure ulcer stage 4 of right lower leg
- Pressure ulcer stage 4 of toes
- 573 Skin graft for skin ulcer or cellulitis with mcc
- 574 Skin graft for skin ulcer or cellulitis with cc
- 575 Skin graft for skin ulcer or cellulitis without cc/mcc
- 592 Skin ulcers with mcc
- 593 Skin ulcers with cc
- 594 Skin ulcers without cc/mcc
Tabular List Of Diseases And Injuries
The Tabular List of Diseases and Injuries is a list of ICD-10 codes, organized head to toe into chapters and sections with coding notes and guidance for inclusions, exclusions, descriptions and more. The following references are applicable to the code L89.153:
Inclusion Terms
- Healing pressure ulcer of sacral region, stage 3
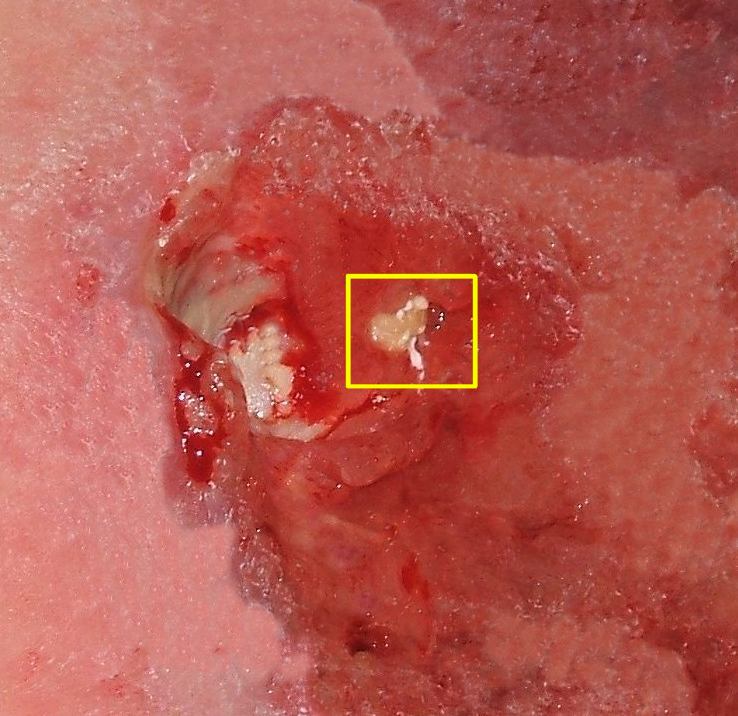
- Pressure ulcer with full thickness skin loss involving damage or necrosis of subcutaneous tissue, sacral region
Pressure Ulcer Icd 10 Diagnosis
When admitted to an acute or chronic hospital, patients must undergo a thorough skin examination to determine whether they have developed a pressure ulcer ICD 10 and whether they have symptoms of previous pressure ulcer ICD 10 . The assessment of the skin can be done with various tools, but the most common is the use of the Braden scale. This assessment includes the presence of previous ulcers and an assessment of the risk of developing pressure ulcer ICD 10.
The scale checks the following sensory parameters:
- sensation of the skin
- assessment of friction forces
- shear forces on the affected skin
The Braden scale is rated by a factor of 1 to 4, with the exception of frictional shear, which has three points on its scale. Points are added up to get a score.
The highest possible Braden score is 23. A patient with a score of 18 or less is considered at risk for pressure ulcer ICD 10. The general health and nutritional status of the patients are also assessed. Particular care is required to prevent pressure-related skin changes and risks. If the patient has a pressure ulcer ICD 10, it should be an ulcer that can be documented with photographic evidence.
Don’t Miss: Ulcerative Colitis Versus Crohn’s Disease
Pressure Ulcer Of Unspecified Part Of Back Stage 4
- 2016201720182019202020212022Billable/Specific Code
- L89.104 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.104 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.104 – other international versions of ICD-10 L89.104 may differ.
- Healing pressure ulcer of unspecified part of back, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, unspecified part of back
- Applicable To annotations, or
Q& a: Clarifying New Guidance For Pressure Ulcers Deep
Q: Our coding department was told there were changes made for fiscal year 2020 when it comes to reporting healed/healing pressure ulcers and pressure-induced deep tissue damage. Can you explain any recent updates?
A: You are right, there have been updates to guidance surrounding these diagnoses.
First, the FY 2020 ICD-10-CM Official Guidelines for Coding and Reporting have additional clarity on patients admitted with pressure ulcers documented as healed. The guidelines added the phrase at the time of admission. The guidelines now state that there is currently no code assignment for pressure ulcers that are completely healed at the time of admission.
In contrast, if the pressure ulcer is documented as healing but not yet healed, the coder is to code the pressure ulcer to the appropriate pressure ulcer stage at the time of admission. Meaning, if the pressure ulcer was to the bone but improves during the stay to only include the depth of the subcutaneous tissue , the pressure ulcer is to be reported as a stage 4 pressure ulcer, not a stage 3.
If a pressure ulcer was present on admission and is healed at the time of discharge, the site and stage of the pressure ulcer at the time of admission should be reported. Remember, healed at the time of admission is the only time a pressure ulcer would not be reported, because it no longer exists.
- L89.126, pressure-induced deep tissue damage of left upper back
- L89.156, pressure-induced deep tissue damage of sacral region
Read Also: How Long Do Ulcerative Colitis Flare Ups Last
Follow 4 Tips For Perfect Pressure Ulcer Dx
Look for site, severity, and more.
When your surgeon treats pressure ulcers, you’ll need to focus your diagnosis coding if you want to demonstrate medical necessity for the procedure.
Also called decubitus ulcers or “bed sores,” surgeons might debride the area, allowing the wound to stay open to heal, which you’d report with codes in the range 11042-+11047 . This process is called closure by secondary intention, versus primary intention, which involves some sort of definitive, active closure.
Alternatively, the surgeon might excise the ulcer and close the wound, which would direct you to codes 15920-15999 .
Either way, you need the following four expert tips to make sure you’re correctly reporting diagnosis codes on your claims:
Tip 1: Determine if Ulcer Involves Gangrene
If your surgeon’s notes indicate the patient has gangrene, you’ll need to code that first before you dig into the pressure ulcer codes. ICD-10-CM directs you to code the condition with I96 and sequence it before the specified pressure ulcer.
Tip 2: Identify Pressure Ulcer Anatomic Site
Surgeons need to carefully document the location of decubitus ulcer treated in a single operative session, because anatomic site is the starting point for accurate coding. ICD-10 breaks down pressure ulcer sites in the following way:
As we move to more outcomes-based care, correctly identifying the pressure ulcer site will become even more important for coverage and reimbursement.
Tip 3: Code for Laterality
- 5: Unspecified.
When To Use L89153 For Pressure Ulcer Of Sacral Region
Pressure ulcer of sacral region, stage 3 Billable Code. L89.153 is a valid billable ICD-10 diagnosis code for Pressure ulcer of sacral region, stage 3 . It is found in the 2021 version of the ICD-10 Clinical Modification and can be used in all HIPAA-covered transactions from Oct 01, 2020 Sep 30, 2021 .
Recommended Reading: Ulcerative Colitis And Stomach Pain
What Is A Stage 4 Sacral Wound
Stage 4 bedsores are the most severe form of bedsores, also called pressure sores, pressure ulcers, or decubitus ulcers. A stage 4 bedsore is characterized by a deep wound that reaches the muscles, ligaments, or even bone. They often cause residents to suffer extreme pain, infection, invasive surgeries, or even death.
Info For Medical Coders On How To Properly Use This Icd
- Inclusion Terms:
Inclusion Terms
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
- Healing pressure ulcer of sacral region, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, sacral region
Recommended Reading: Ulcerative Colitis Causes And Treatment
Coding Tip: Reporting Pressure Ulcers
Kim Boy, RHIT, CDIP, CCS, CCS-P
This Coding Tip was updated on 07/12/22
The coding of pressure ulcers has seen many changes over the past several years. Coders have seen that ICD-10-CM also came with changes on reporting of these ulcers.
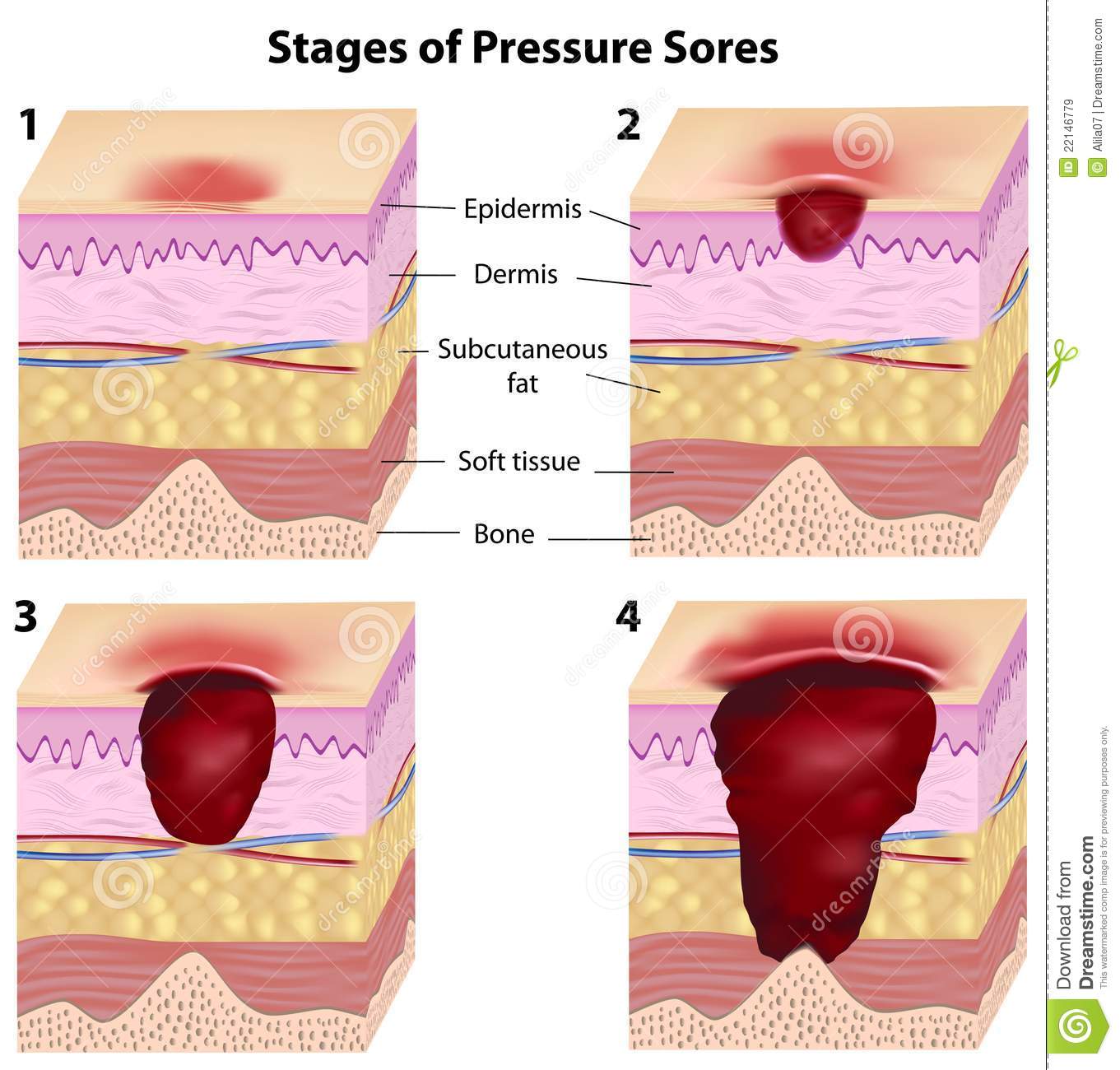
With ICD-10-CM, the code for reporting pressure ulcers now identifies the site and the stage of the ulcer. Pressure ulcer stages are based on severity of the ulcer:
- Unspecified stage and
If a patient has more than one pressure ulcer a code for each should be reported.
Sometimes, coders will confuse unstageable with unspecified stage of the ulcers. There is a big difference between the two meanings:
- Unstageable pressure ulcers are diagnosed when the physician or clinician is not able to stage due to the ulcer being covered by eschar or possibly even a skin graft. If a patient with an unstageable pressure ulcer has a debridement and the stage of the ulcer is then revealed and documented, only code the stage revealed and not unstageable.
- Unspecified pressure ulcers are reported with there is a lack of documentation regarding the pressure ulcer stage
There are only a few areas in coding where the coder is allowed to take documentation from anyone other than the physician. The staging of the pressure ulcer is one of those exceptions. Other clinicians can document the stage of an ulcer and coders may code from this documentation. However, the diagnosis of the ulcer itself must be documented by the physician/provider.
Pressure Ulcer Icd 10 Treatment
Treatingpressure ulcer ICD 10 include:
- reducing the pressure on affected skin
- caring for the wound
- preventing infection
- keeping a good diet is needed
Members of the care team are a GP who supervises the treatment plan, a nurse who specialises in wound care, a nurse who provides care and training, and someone who administers the wound. Physicians specialized in skin diseases may also be involved. The nursing team may also include a social worker to help the patient and his family access resources and address emotional concerns related to long-term recovery, a physiotherapist to help improve mobility, an occupational therapist to ensure adequate seating and a nutritionist to monitor the patients nutritional needs and recommend good nutrition.
The following list contains numerous ways to treat and manage pressure ulcer ICD 10:
Read Also: How Do You Stop A Stomach Ulcer From Hurting
Pressure Ulcer Of Left Hip Stage 4
- 2016201720182019202020212022Billable/Specific Code
- L89.224 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.224 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.224 – other international versions of ICD-10 L89.224 may differ.
- Healing pressure ulcer of left hip, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, left hip
- Applicable To annotations, or
Q& A: Clarifying New Guidance For Pressure Ulcers Deep
Q: Our coding department was told there were changes made for fiscal year 2020 when it comes to reporting healed/healing pressure ulcers and pressure-induced deep tissue damage. Can you explain any recent updates?
A: You are right, there have been updates to guidance surrounding these diagnoses.
First, the FY 2020 ICD-10-CM Official Guidelines for Coding and Reporting have additional clarity on patients admitted with pressure ulcers documented as healed. The guidelines added the phrase at the time of admission. The guidelines now state that there is currently no code assignment for pressure ulcers that are completely healed at the time of admission.
In contrast, if the pressure ulcer is documented as healing but not yet healed, the coder is to code the pressure ulcer to the appropriate pressure ulcer stage at the time of admission. Meaning, if the pressure ulcer was to the bone but improves during the stay to only include the depth of the subcutaneous tissue , the pressure ulcer is to be reported as a stage 4 pressure ulcer, not a stage 3.
If a pressure ulcer was present on admission and is healed at the time of discharge, the site and stage of the pressure ulcer at the time of admission should be reported. Remember, healed at the time of admission is the only time a pressure ulcer would not be reported, because it no longer exists.
- L89.126, pressure-induced deep tissue damage of left upper back
- L89.156, pressure-induced deep tissue damage of sacral region
You May Like: Venous Stasis Ulcer Signs And Symptoms
Pressure Ulcer Of Sacral Region Unspecified Stage
- 2016201720182019202020212022Billable/Specific Code
- L89.159 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.159 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.159 other international versions of ICD-10 L89.159 may differ.
- Healing pressure ulcer of sacral region NOS
- Healing pressure ulcer of sacral region, unspecified stage
- Applicable To annotations, or
L895 Pressure Ulcer Of Ankle
Pressure ulcer of unspecified ankle
Pressure ulcer of right ankle
Recommended Reading: Medication For Ulcers Over The Counter
The Dilemma Of Coding And Reporting Deep
Confusion and apprehension surround new guidelines for deep-tissue pressure injury.
The release of the 2020 Official Guidelines for Coding and Reporting has resulted in confusion and apprehension surrounding the intent of the new guideline related to the new ICD-10-CM codes for pressure-induced deep-tissue damage, or deep-tissue pressure injury .
The ambiguity stems from what appears to be conflicting advice found within the coding guidelines regarding pressure ulcer stage codes.
To provide history on the introduction of the new ICD-10-CM codes, we can reference the September 2018 Coordination and Maintenance Committee meeting. During this meeting, the following three points were discussed, based upon the request by the Centers for Medicare & Medicaid Services for Healthcare Research and Quality for new codes in order to identify and track deep-tissue injuries for surveillance and quality improvement purposes. The National Pressure Ulcer Advisory Panel serves as the authoritative voice for improved patient outcomes in pressure ulcer prevention and treatment through public policy, education, and research. In 2016, the NPUAP adopted several changes to pressure ulcer staging, based on recent clinical literature and expert consensus, which introduced minor inconsistencies with ICD-10-CM.
The guidelines referenced in this article are as follows:
Patient admitted with pressure ulcer evolving into another stage during the admission:
What Is The Cause Of Sacroiliitis
What causes sacroiliitis? Inflammation of the sacroiliac joint causes most of the symptoms of sacroiliitis. Many medical conditions cause inflammation in the sacroiliac joint, including: Osteoarthritis -This type of wear-and-tear arthritis can occur in the sacroiliac joints and results from the breakdown of ligaments.
Recommended Reading: What Does An Eye Ulcer Look Like
Audit Considerations & Strategies
- The original coder did not code the pressure ulcer excision. Adding either the right or left hip excision would drive the case from a medical DRG to a surgical DRG
- The procedure code may have been overlooked because the surgeon documented that the tissue was excised rather than documenting that an excisional debridement was performed
- Documentation of excision or excised is sufficient to code PCS root operation: Excision
- Always carefully review the entire medical record including the Progress Notes for bedside procedures, especially for patients with pressure ulcers
- Per Coding Clinic1, the body part value for an excisional debridement performed on a muscle in the sacral region is the Hip muscle. If the documentation specifies that the right side or left side of the sacral ulcer was debrided, then a single code can be assigned. If the documentation does not specify laterality, assign codes for both the right and left hip muscles.
- Since only excision of sacral pressure sore was noted, both the 0KBN0ZZ and 0KBP0ZZ codes were assigned
- Coding Clinic likely allows coders to assume both the right and left hip muscles when laterality is not specified because sacral pressure ulcers often develop on the lower back which would include portions of the left and right hips
- Cases with a principal diagnosis of stage 3 or 4 pressure ulcer automatically result in DRG 592: Skin ulcers with MCC
- ICD-10 only requires one code to be assigned for the pressure ulcer and stage
Reference
L898 Pressure Ulcer Of Other Site
Pressure ulcer of head
Pressure ulcer of other site
Also Check: Signs And Symptoms Of Bleeding Ulcer