How Can I Reduce My Risk Of Foot And Toe Ulcers
There are several things you can do to help reduce your risk of getting foot and toe ulcers. Sometimes, adopting these habits can even stop them from coming back. Try to:
- Manage your diabetes. If you have diabetes you should wear appropriate footwear and never walk barefoot.
- Examine your legs as well as the tops and bottoms of your feet and the areas between your toes every day. Look for any blisters, cuts, cracks, scratches or other sores. Also check for redness, increased warmth, ingrown toenails, corns and calluses. Use a mirror to view your leg or foot if necessary. If its difficult to see, ask a family member to look at the area for you. See a healthcare provider immediately if you notice any problems.
- Talk to your healthcare provider about ways you can stop smoking.
- Manage your blood pressure.
- Control your cholesterol and triglyceride levels by changing your diet. Limit salt in your diet.
- Care for your toenails frequently. Cut your toenails after bathing, when they are soft. Cut toenails straight across and smooth with a nail file. Take care of ingrown toenails.
- Exercise.
- Wear appropriate shoes and socks. Talk to your podiatrist about what you need.
How Can I Prevent Leg Ulcers
Leg ulcers commonly open up again after healing. These steps can lower the risk of getting a leg ulcer or a wound recurrence:
- Elevate your legs above your heart when youre sitting or sleeping.
- Maintain a healthy weight and stay physically active.
- Manage health conditions that affect blood circulation, including diabetes, high blood pressure, high cholesterol and Raynauds syndrome.
- Quit smoking and using tobacco products. Talk with your healthcare provider about ways to stop smoking.
- Use gentle cleansers, and apply moisturizing lotion to prevent dry skin.
- Wear compression stockings or bandages for an hour each day to improve blood flow to the legs.
Can Venous Leg Ulcers Be Prevented
There are several ways to help prevent a venous leg ulcer in people at risk, such as:
- wearing compression stockings
- losing weight if youre overweight
- exercising regularly
- elevating your leg when possible
This is particularly important if youve previously had a leg ulcer once a leg has suffered a venous ulcer, youre at risk of further ulcers developing within months or years.
Don’t Miss: Nursing Diagnosis For Ulcerative Colitis
Where Do They Occur
Skin cancers tend to occur more in sun-exposed areas of the body such as the ears, nose, forehead, upper lips, shoulders, and the back and lower legs. However, some ulcers can develop internally due to cancer under the skinan ulcer can be a result of breast or bone cancer growing close to the surface of the skin.
Healthcare Advice For Leg Ulcers

There are some lifestyle changes you can make that will help boost healing:
- Maintain a healthy weight
- Eat a well-balanced diet that includes 5 portions of fruit and vegetables a day and protein rich foods such as eggs, fish, chicken or pulses
- Take light to moderate exercise such as cycling or walking for about thirty minutes at least three times a week
- Avoid standing or sitting for long periods of time
- Put your feet up elevate your legs above your heart.
- Every so often, move your feet around in circles, then up and down. This helps blood circulate and get back to your heart
Dont Miss: Do Stomach Ulcers Cause Nausea
Also Check: How Can You Tell If You Have An Ulcer
Who Is At Risk For A Decubitus Ulcer
Individuals with limited mobility and who remain for long periods of time sitting or lying in the same position are vulnerable to developing pressure ulcers. Older individuals with more fragile skin are also at risk. Other risk factors include:
- Poor diet with insufficient nutrients for skin health.
- Not drinking enough water to hydrate skin.
- Medical conditions such as diabetes which causes poor blood circulation to skin tissue.
Risks Of Bed Sores During The Pandemic
Not only has the COVID-19 pandemic increased the number of patients who need hospitalization, but it has also complicated care and bed sores prevention. Sedated COVID patients are usually placed on their belly instead of their neck to assist with breathing. So, in this position, nurses dont look for pressure injuries on the patients back but keep a sharp eye on their:
- face
- shoulders
- ears
Moreover, rare coronavirus symptoms may be mistaken for bed sores in elderly patients. For that purpose, the National Pressure Injury Advisory Panels position paper warns health care providers to be alert to skin discoloration in COVID-19 patients. In other words, skin manifestations like COVID toespinkish-reddish pernionlike lesions that turn blue to purple in timecan resemble deep tissue injury but are actually a symptom of the virus.
Dont Miss: Is Ulcerative Colitis A Gastrointestinal Disease
Read Also: How To Prevent Ulcers In The Stomach
How Can You Prevent Ulcers
Theres a lot you can do to reduce your risk for ulcers:
- Check yourself: If you cant feel parts of your body — such as your feet — because of nerve damage, take a look at them every day. Look for blisters, cuts, cracks, sores, redness, white spots, thick , discoloration, or other changes. If you feel warmer or colder than usual, that can be a sign that you have an open wound. But you may not feel anything. If you cant check your legs or feet yourself, ask a family member to help.
- Protect your feet: Dont walk barefoot, especially if you have diabetes or cant feel your feet. A foot injury can increase your risk for ulcers. Shoes that cover the whole foot, instead of sandals or flip-flops, are best.
- Quit smoking: Cigarettes damage blood vessels, decrease blood flow, and slow healing. Those things increase your risk for ulcers and amputation. If you smoke, talk to your doctor about resources that can help you kick the habit.
When Should I See My Healthcare Provider About Foot And Toe Ulcers
If you have diabetes, its important to see a podiatrist regularly. Whether you have diabetes or not, you should see a healthcare provider immediately if you find an ulcer on your foot or toe. Left untreated, it could get infected, leading to complications like amputations.
A note from Cleveland Clinic
It can be distressing to discover an open sore on your foot or toe. You might not know what caused it, it might not be healing and, if you have neuropathy from diabetes, you might not even feel it. Keep in mind that your healthcare provider can successfully treat your ulcer, especially if its found early. If left untreated, an ulcer can lead to serious complications.
If you have neuropathy caused by diabetes, remember that its important to check your feet and toes on a regular basis. Check your toes and feet every time you shower or when you go to put on your shoes. Contact your healthcare provider right away if you find an ulcer.
Don’t Miss: How Do You Heal A Bleeding Ulcer
How Do You Treat Pressure Sores On The Buttocks
Pressure sores on the buttocks are treated by proper wound care and by repositioning to remove the pressure source, states ClinicalKey. Pressure sores on the buttocks are due to long periods of uninterrupted pressure on the skin, soft tissue, muscle and bone.
There are four stages of pressure sores, according to ClinicalKey. The first stage is redness of the skin, and the second stage is partial thickness skin loss involving the epidermis and dermis. The third stage is full thickness skin loss involving the subcutaneous tissue. The fourth stage involves muscle and bone.
Prevention is the most important factor in managing pressure sores, explains ClinicalKey. For necrotic, deep and poorly healing wounds, surgical debridement may be necessary. If infection of the soft tissue or bone is present, antibiotics are needed.
Pressure sore develop in people who are chair- or bed-bound, elderly patients, hospital inpatients and people with spinal cord injuries, notes ClinicalKey. Those who are more predisposed to developing pressure sores are patients with conditions causing poor wound healing, such as diabetes and nutritional insufficiency, and those with conditions causing low tissue oxygen tension. People with fecal or urinary incontinence are also more prone to developing pressure sores, as urine and feces act as skin irritants to break down skin.
How To Heal Leg Ulcers Naturally
What You Have To Do
How Often You Should Do This
Do this 2-3 times daily.
Why This Works
Aloe vera is a therapeutic herb that is widely used to treat various ailments. It is extremely effective in healing leg ulcers as it not only inhibits the growth of bacteria but also prevents further infection . It contains compounds like anthraquinones and certain hormones that are said to render wound healing properties to it .
Also Check: What Can You Eat With A Stomach Ulcer
How Are Leg Ulcers Treated
At Cleveland Clinic, patients are treated by a team of world-class experts in the Lower Extremity Wound Clinic in the Department of Vascular Medicine. This Clinic includes doctors, nurses and other medical specialists.
These experts work together to determine the cause of the ulcer and develop an individualized treatment program.
The goals of treatment are to relieve pain, speed recovery and heal the wound. Each patients treatment plan is individualized, based on the patients health, medical condition and ability to care for the wound.
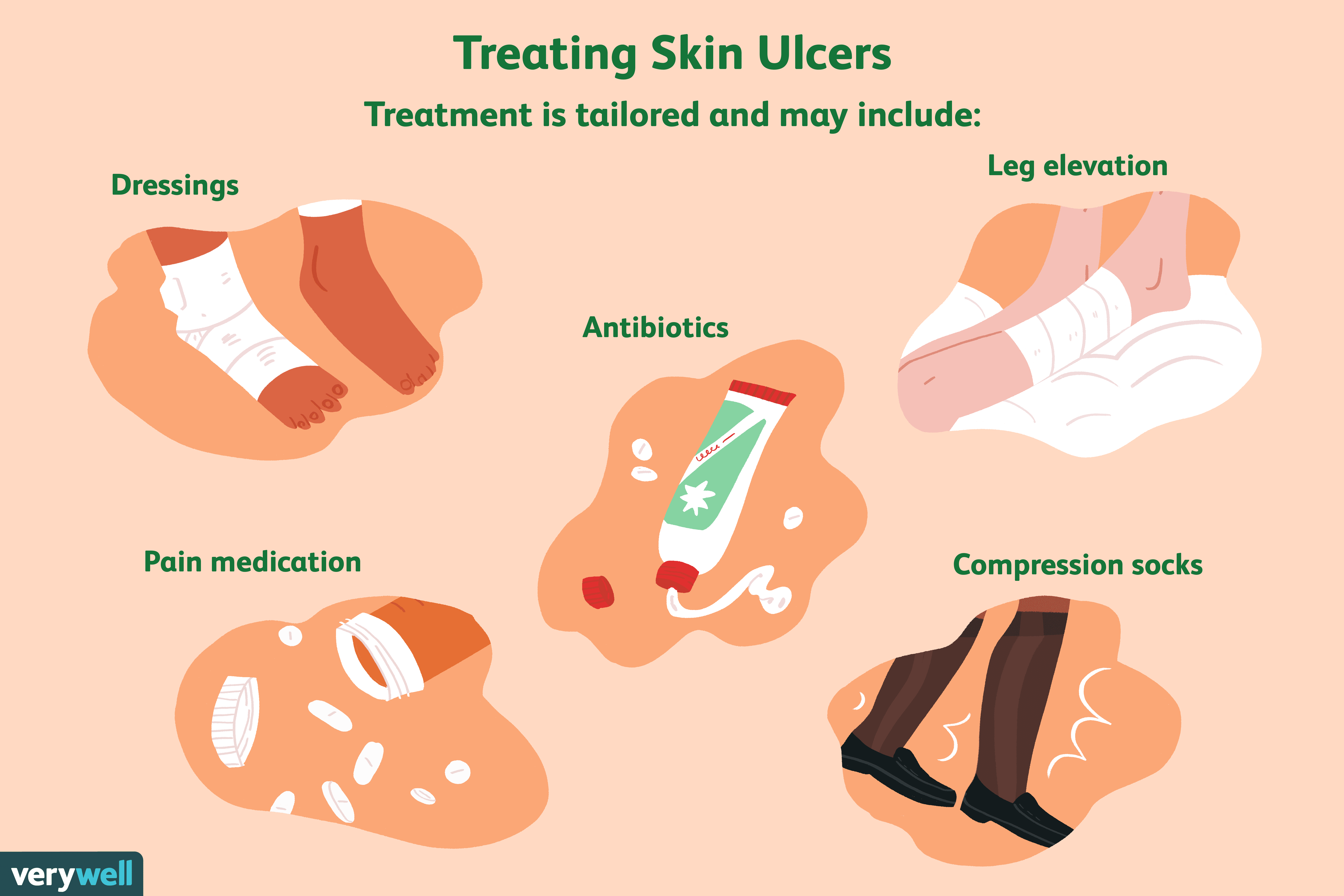
Treatment options for all ulcers may include:
- Antibiotics, if an infection is present
- Anti-platelet or anti-clotting medications to prevent a blood clot
- Topical wound care therapies
- Prosthetics or orthotics, available to restore or enhance normal lifestyle function
Venous Ulcer Treatment
Venous ulcers are treated with compression of the leg to minimize edema or swelling. Compression treatments include wearing compression stockings, multi-layer compression wraps, or wrapping an ACE bandage or dressing from the toes or foot to the area below the knee. The type of compression treatment prescribed is determined by the physician, based on the characteristics of the ulcer base and amount of drainage from the ulcer.
The type of dressing prescribed for ulcers is determined by the type of ulcer and the appearance at the base of the ulcer. Types of dressings include:
- Moist to moist dressings
Arterial Ulcer Treatment
Wound Cleaning And Dressing
To heal, pressure sores need to be cleaned, dead skin needs to be removed , and dressings need to be applied.
The wound is cleaned when the dressing is changed. Health care practitioners often flood the wound, particularly its deep crevices, with saline to help loosen and clean away hidden debris.
A doctor may need to remove dead tissue with a scalpel, a chemical solution, a whirlpool bath , a special dressing, or biosurgery . Removal of dead tissue is usually painless, because pain is not felt in dead tissue. Some pain may be felt because healthy tissue is nearby.
Dressings Dressings Topical drugs are a mainstay of treating skin disorders. Systemic drugs are taken by mouth or given by injection and are distributed throughout the body read more are used to protect the wound and promote healing. Dressings are used for some stage 1 pressure sores and all others. When the skin is broken, a doctor or nurse considers the location and condition of the pressure sore when recommending a dressing. The amount of drainage oozing from the sores helps determine which type of dressing is best.
Also Check: Stage 3 Pressure Ulcer Treatment
Also Check: Are Beets Good For Ulcerative Colitis
Who Gets Foot And Toe Ulcers
Foot and toe ulcers can happen to many people but might be more common in Black, Native American and Hispanic people. If you have an eye, kidney or heart disease related to diabetes, youre also at a higher risk. About 15% of people with diabetes will get an ulcer, typically on the bottom of their foot. Some of those people will be hospitalized because of complications.
Youre also at a higher risk of getting foot and toe ulcers if you have any of the following conditions:
- Blood circulation issues.
- Grey.
- Black.
If your ulcer is black, that means cells in the tissues have died. This is called necrosis .
Ulcers Caused By Injury Or Pressure
- Injury. Most ulcers start off with an injury to the skin. Some are trivial a little scratch or bite for example, which doesn’t properly heal for some reason, such as a circulation problem as above. Others may be larger skin injuries, or injuries which extend more deeply to tissue under the skin.
- Neuropathic ulcers. Some injuries to the skin occur because there is a problem with the feeling in the skin. If you can’t feel your feet, for example, you may not be able to tell that a shoe is too tight, or the bath is too hot. So you end up with a blister or a burn, which can go on to become a skin ulcer, particularly if your circulation is not very good. Ulcers caused in this way are called neuropathic ulcers. Diabetes is the common cause. See the separate leaflet called Diabetes, Foot Care and Foot Ulcers.
- Pressure sores are a common type of skin ulcer. Areas of skin become damaged due to a continuous pressure on them, usually due to a person not being able to move well. See the separate leaflet called Pressure Sores.
Read Also: Ulcerative Colitis And Back Pain
Basic Approach To Patients With Inflammatory Ulcers
The diagnosis of inflammatory ulcers begins with a detailed history. Several important questions need to be to be asked , and the following is a reasonable list. What was the primary lesion? How did the lesion progress? How fast was the progression to ulceration? Was the lesion painful? What management and treatment interventions took place and have they improved or worsened the condition? Has there been a similar problem in the past? Were any new medications started over the last couple of months? Was a surgical procedure performed in the last several months? Have there been any changes in the patient’s general health? A thorough review of systems provides clues to diagnosis. A past medical history of connective tissue diseases, diabetes, heart disease, kidney disease, inflammatory bowel disease, hepatitis, hypertension, coagulopathies, prior pregnancy, and malignancies help support or suggest a particular etiology and diagnosis.
Wound Bed score and its individual features
The total WBS adds each individual score for each characteristic to give a total score. Percent of eschar present Severity of peri-ulcer dermatitis Depth of the wound Severity of callus/fibrosis Percent of pink granulation tissue present Severity of edema Percent of healing edges Frequency of dressing changes
Examples of some inflammatory ulcers
Risk Factors For Leg Ulcers
- Age peripheral circulation becomes less efficient with old age.
- Varicose veins the one-way valves that stop blood from travelling backwards in the vein stop working. The pooling of blood stretches and distorts the vein.
- Cigarette smoking tobacco is known to constrict the vessels of the circulatory system.
- Arterial disease vein problems are more likely if the person already has other diseases of the arteries.
- Certain disorders these include diabetes and arthritis.
- Pressure sores bed-bound people are at risk of pressure sores, which are areas of damage to the skin caused by constant pressure or friction.
- Medication some cardiovascular medications can contribute to leg oedema and altered circulation.
Don’t Miss: What Are The First Signs Of A Stomach Ulcer
Ulcers Caused By Problems With Blood Circulation
The blood supply coming to the skin is needed for the skin to heal after it has become broken or split for any reason. If there is a problem with circulation, the break in the skin does not heal, and may persist, leaving an ulcer. This may be a problem with the veins, the arteries, or the smaller blood vessels. The kinds of ulcers caused by circulation problems are:
- Venous ulcers. These ulcers and their treatment are described in the separate leaflet called Venous Leg Ulcers. They occur when the circulation in your legs is not working very well. Fluid tends to pool in the legs because the veins don’t work well enough to pump the blood efficiently back to the heart . This type of ulcer is more common in people with varicose veins that have lead to associated skin problems such as varicose eczema. They are also more common if you are overweight or obese, or not very mobile for any reason. They can also occur when the circulation is damaged by a deep vein thrombosis .
- Arterial ulcers. These are caused by conditions affecting arteries – see the separate leaflet called Peripheral Arterial disease.
- Vasculitic ulcers. These are caused by a number of conditions which cause blood vessels to become inflamed. This is called vasculitis.
Swelling In The Legs And Ankles
Venous leg ulcers are often accompanied by swelling of your feet and ankles , which is caused by fluid. This can be controlled by compression bandages.
Keeping your leg elevated whenever possible, ideally with your toes above your hips, will also help ease swelling.
You should put a suitcase, sofa cushion or foam wedge under the bottom of your mattress to help keep your legs raised while you sleep.
You should also keep as active as possible and aim to continue with your normal activities.
Regular exercise, such as a daily walk, will help reduce leg swelling.
But you should avoid sitting or standing still with your feet down. You should elevate your feet at least every hour.
You May Like: What To Do For Mouth Ulcers