What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
What To Eat In An Ulcerative Colitis Flare
While certain foods can be very well tolerated during good periods of the disease, these may then become an issue during an Ulcerative colitis flare-up.
Once the gut lining becomes inflamed and irritated this can lead to anything passing along it feeling very painful. This irritation along the gut lining not only leads to abdominal pain but can also lead to more blood loss. Removing certain foods for a period of time may help to reduce the strain on the gut and lower levels of the blood being lost.
Ways to reduce the fibres that can irritate the gut include:
- Removing stems and skins from fruits and vegetables
- Cooking and pureeing fruits and vegetables
- Avoiding nuts and seeds
Dairy has also been indicated to be an issue for many people with Ulcerative colitis and can potentially contribute to a flare. If a specific food is leading to an immune reaction may then contribute to the inflammatory response which damages the gut and causes blood loss in the stool of those with Ulcerative colitis.
Removing dairy may calm the immune response and flare-up. A 2014 study concluded that the intake of dairy products may increase the severity of Ulcerative colitis.
Could I Have An Ulcer And Not Know It
Around 25 million people will have a stomach ulcer in their lifetime, according to the Centers for Disease Control and Prevention. Despite their prevalence, the symptoms of an ulcer can frequently be mistaken for other conditions, like heartburnand some people may not show any signs at all. Its also unlikely that stress or your diet is the culprit. If youre concerned that your stomach pain could be something more serious, read on to find out the causes, proper treatment and prevention methods for peptic ulcers.
You May Like: Specific Carbohydrate Diet Ulcerative Colitis
Is Ulcerative Colitis Characterized By Symptoms
The intensity of the disease determines the symptoms. Some symptoms include diarrhea, frequent stools, and blood in the stool as well as an urge to defecate along with rectal pain and incontinence from time to time.
Severe cases can include weight loss, swelling of the legs, weariness, dyspnea, and fever as well as failure to grow in height. Stools that include blood are the most common symptom, however, diarrhea is not required.
What are the Consequences of Ignoring the Problem?
Without treatment, the person will continue to lose blood and become anemic as a result of the condition.
Diarrheaand diarrhea-related problems may occur. Uncontrolled diseases can lead to obstructions of the colon and even cancer. It can affect other organs.
There is a possibility that a person will get joint discomfort, liver illness, bone disease, skin disease, ulcers in the mouth, and even an elevated risk for developing blood clots in the body.
What Is The Difference Between Peptic Ulcers Gerd And Gastritis
Peptic ulcers are holes or lesions that form due to too much acid. GERD, which stands for gastroesophageal reflux disease, occurs when a persons stomach acid repeatedly backs up into the esophagus. Gastritis is a group of conditions that cause inflammation in the stomach. While all of these conditions affect the stomach, they are not the same and require different treatments.
Recommended Reading: How To Heal Tongue Ulcers
Read Also: How To Determine If You Have A Stomach Ulcer
Treatments For Ulcerative Colitis
Ulcerative colitis is a chronic condition, which means you will have to manage it for the rest of your life. There is no cure for ulcerative colitis.
However, there are a variety of treatment options that can help you manage your symptoms and have long-term remission. Your treatment will depend on the severity of your condition, your symptoms, your overall health, and your goals. UCHealth specialists will work closely with you to formulate the right treatment plan.
UC medications
Medications are usually the first treatment for ulcerative colitis. There are many different types to help you manage different symptoms.
Anti-inflammatory medications
- 5-aminosalicylates: These medications work by blocking the chemicals that trigger inflammation. They can be taken by mouth or as a suppository.
- Corticosteroids: Corticosteroids are powerful medications that reduce inflammation and immune system activity. They are usually used in moderate or severe cases of UC that dont respond to other treatments. Long-term use of corticosteroids can have negative side effects.
Immunosuppressants
Ulcerative colitis is an autoimmune condition. So, if anti-inflammatory medications arent working, your doctor may prescribe medications to suppress your immune system to stop UC from attacking your large intestine. Certain commonly prescribed immunosuppressants for UC can affect your liver and pancreas, however, so you will need to have regular follow-ups with your doctor.
Biologics
Other UC medications
Treatment For Rectal Bleeding
The kind of treatment you require depends on your diagnosis and location of the bleeding.
You should notify your doctor at first sight of the blood, as causes of rectal bleeding can be as harmless as a hemorrhoid and as severe as cancer. You will also want to monitor the accompanying symptoms to help you narrow down on the cause of your blood in stool. Once you run the necessary tests, your doctor will be able to confirm your diagnosis and put you on a treatment plan.
Rectal bleeding treatment may involve managing hemorrhoids, replenishing blood loss, supplementing vitamins and minerals, using ointments or suppositories, staying well hydrated, preventing constipation and diarrhea, increasing your fiber intake, avoiding sitting on the toilet for prolonged periods of time, and applying ice packs in case of pain.
Mohan Garikiparithi got his degree in medicine from Osmania University . He practiced clinical medicine for over a decade before he shifted his focus to the field of health communications. During his active practice he served as the head of the Dept. of Microbiology in a diagnostic centre in India. On a three-year communications program in Germany, Mohan developed a keen interest in German Medicine , and other alternative systems of medicine. He now advocates treating different medical conditions without the use of traditional drugs. An ardent squash player, Mohan believes in the importance of fitness and wellness.
Recommended Reading: Can Ulcers Make You Have Diarrhea
Uc Is A Chronic Disease
Ulcerative colitis is a chronic disease, meaning it lasts a long time and cannot be cured. There may be times when your symptoms go away for several months or even years, but your symptoms will eventually come back during a flare-up event.
However, with the treatment and support, you can greatly reduce your symptoms and bring about long-term remission.
What Are The Symptoms Of Rectal Bleeding
The symptoms of rectal bleeding can vary depending on what is causing the bleeding. Most causes of rectal bleeding are treatable and not serious. In some cases, rectal bleeding can be a symptom of a serious disease, such as colorectal cancer. Because it can be hard to know the cause of your rectal bleeding at home, its usually a good idea to reach out to your healthcare provider if you have rectal bleeding.
Some symptoms you might have with rectal bleeding can include:
- Feeling rectal pain and/or pressure.
- Seeing bright red blood in or on your stool, underwear, toilet paper or in the toilet bowl.
- Having stool thats red, maroon or black in color.
- Having stool that has a tar-like appearance.
- Experiencing mental confusion.
- Feeling lightheaded or dizzy.
In some very severe cases, rectal bleeding can lead to shock. If you experience any symptoms of shock, call 911 right away and get help. The symptoms of shock can include:
- Experiencing a sudden drop in your blood pressure.
- Having a fast heart rate.
- Not being able to urinate.
- Slipping into unconsciousness.
Recommended Reading: Ulcerative Colitis Disability Tax Credit
Recommended Reading: Foods To Eat If You Have A Stomach Ulcer
Diet And Ulcerative Colitis Flare
If you are dealing with a flare-up, you may not have an appetite or know what you can safely eat. Here are some general guidelines.
Avoid potential trigger foods:
- Alcohol and caffeine.
- High-fat foods.
- Insoluble fiber, which is contained in foods like fruits with skins, raw green vegetables , whole nuts, and whole grains.
- Lactose, a sugar that can be found in dairy products.
- Non-absorbable sugars: Sorbitol, mannitol, and other sugar alcohols that can be found in low- or no-sugar products.
Try eating easily-digested foods:
- Low-fiber fruits, like bananas, cantaloupe, honeydew melon, and cooked fruits.
- Lean protein like fish, lean cuts of pork, white meat poultry, soy, and eggs.
- Refined grains found in sourdough or white bread, potato or gluten-free bread, white pasta, white rice, and oatmeal.
- Peeled, low fiber vegetables, like potatoes, cucumbers , and squash.
If you are having a flare-up, be sure to talk to your healthcare team. They can help you come up with both a diet and a treatment plan.
What Causes Bleeding From The Rectal Area
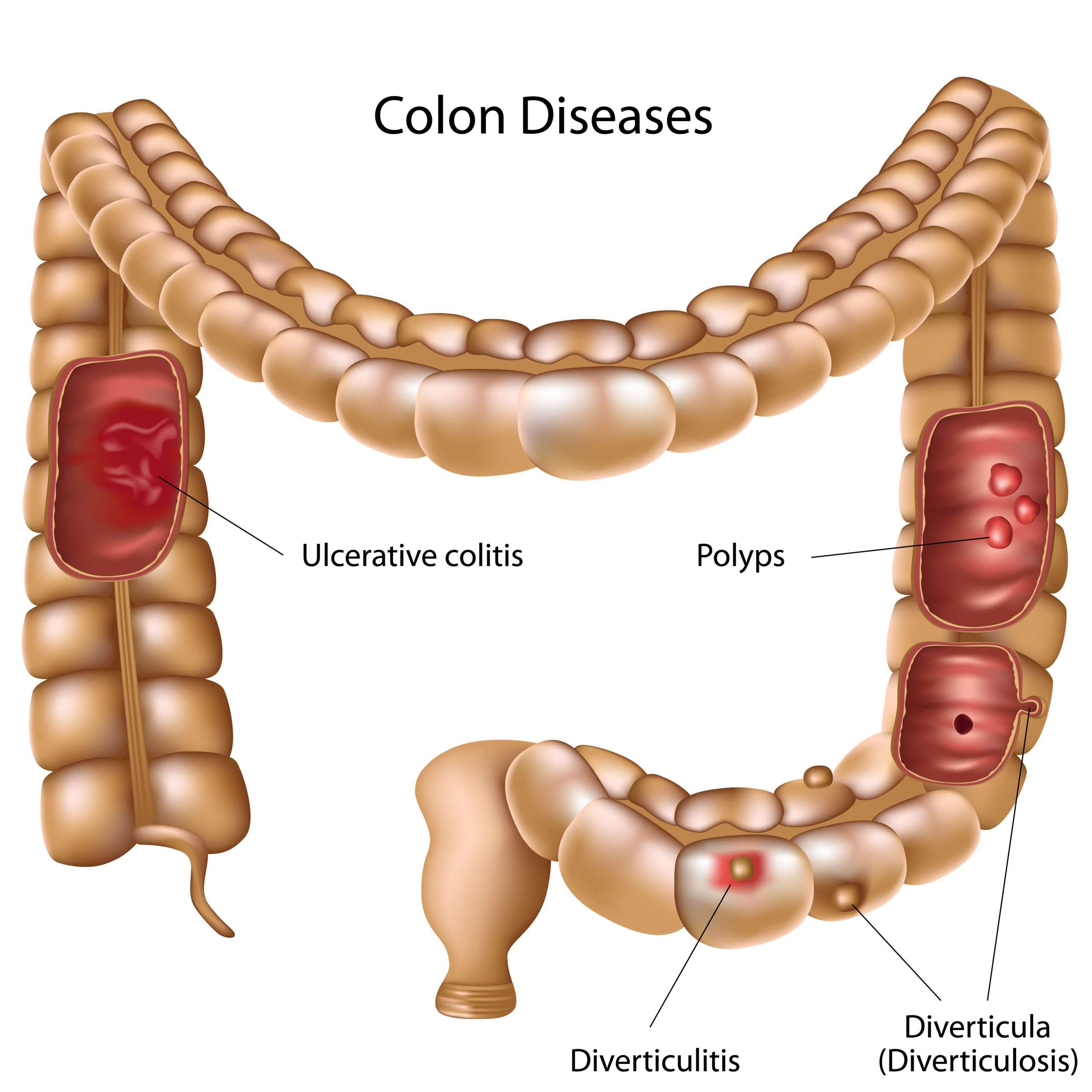
There are many causes of rectal bleeding. Common causes include hemorrhoids, , diverticulosis, infection, inflammation , blood vessel problems . Other causes of rectal bleeding include polyps, tumors, trauma, an upper gastrointestinal source like stomach ulcers, and Meckelâs diverticulum . Ischemia of the bowel occurs when blood flow to the bowel reduces or stops. For example, ischemic colitis usually occurs at the junction of the transverse and descending colon and can produce bright red or maroon blood. This article provides some of the details of the major causes of rectal bleeding.
Recommended Reading: How Do You Heal A Bleeding Ulcer
Black Or Dark Red Blood In Stool
The longer blood is in the digestive tract, the darker it appears. Black, tarry stools are a sign of bleeding in the upper part of the digestive tract, such as the esophagus, stomach, and first part of the small intestine. Dark red blood in stool is a sign that bleeding may be in the small intestine or the beginning of the colon.
Causes of black or dark red blood in the stool may include:
- Inflammatory bowel disease
Of course, not all changes in stool color are due to underlying disease. Certain foods and supplements can also change the color of stool. For example, iron supplements and Pepto-Bismol are known to cause black stools. Black or dark red blood in the stool may also result from eating dark-colored foods like blueberries, black licorice, and dark chocolate.
Read Also: Nutritionist Specializing In Ulcerative Colitis
Youre Going All The Time
Theres actually a wide range of normal here. Anywhere from two bowel movements a week to two a day is the range of whats considered normal, Dr. Higgins says. Typically, people with uncontrolled UC will have more than that. When they’re doing well and in remission, two per day or less is normal, he adds.
Still, Dr. Hong maintains that its more important to focus on the quality of a bowel movement rather than how often you have to go, and whether or not you have any UC symptoms associated with it. Overall, as long as your normal stays the same, youre probably good in that department, he says.
Read Also: How Does Ulcer Pain Feel
Do You Bleed A Lot With Ulcerative Colitis
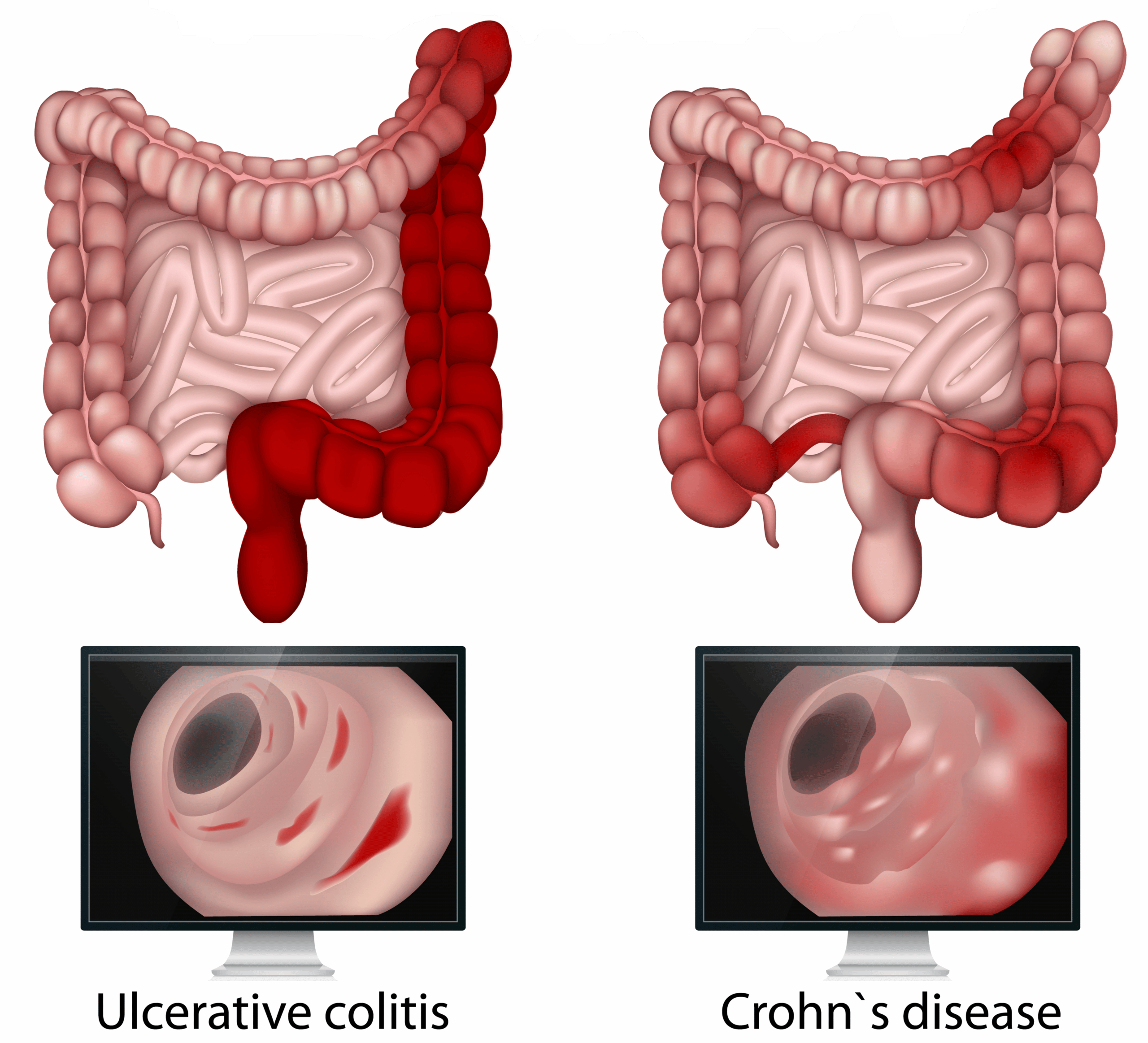
Blood in the stool is reported in the majority of those with Ulcerative colitis, while only one-third of those with Crohns disease report bleeding.
The amount of blood that appears in the stool can vary depending on the disease state. This can range from small amounts of blood that appear on the surface of the stool to higher amounts of blood that turn the toilet water red.
What Are The Symptoms Of A Peptic Ulcer
A dull or burning pain in your stomach is the most common symptom of a peptic ulcer. You may feel the pain anywhere between your belly button and breastbone. The pain most often
- happens when your stomach is emptysuch as between meals or during the night
- stops briefly if you eat or if you take antacids
- lasts for minutes to hours
- comes and goes for several days, weeks, or months
Less common symptoms may include
- feeling sick to your stomach
Even if your symptoms are mild, you may have a peptic ulcer. You should see your doctor to talk about your symptoms. Without treatment, your peptic ulcer can get worse.
Recommended Reading: Ulcerative Colitis What Vitamins Can I Take
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: Ulcerative Colitis And Lactose Intolerance
Drinking Cabbage Juice For Peptic Ulcers
If you have ulcers or inflammation of the stomach lining that is causing internal bleeding and bloody stools, you should drink cabbage juice.
According to a study in the Western Journal of Medicine, cabbage juice reduced the length of time that peptic ulcers took to heal. Researchers concluded that drinking fresh cabbage juice can help to treat peptic ulcers in humans.
In my article on the amazing health benefits of cabbage juice, you can see how to use cabbage juice to boost your digestive health.
Recommended Reading: Pepto Bismol And Ulcerative Colitis
Don’t Miss: How To Cure Ulcerative Colitis In 90 Days
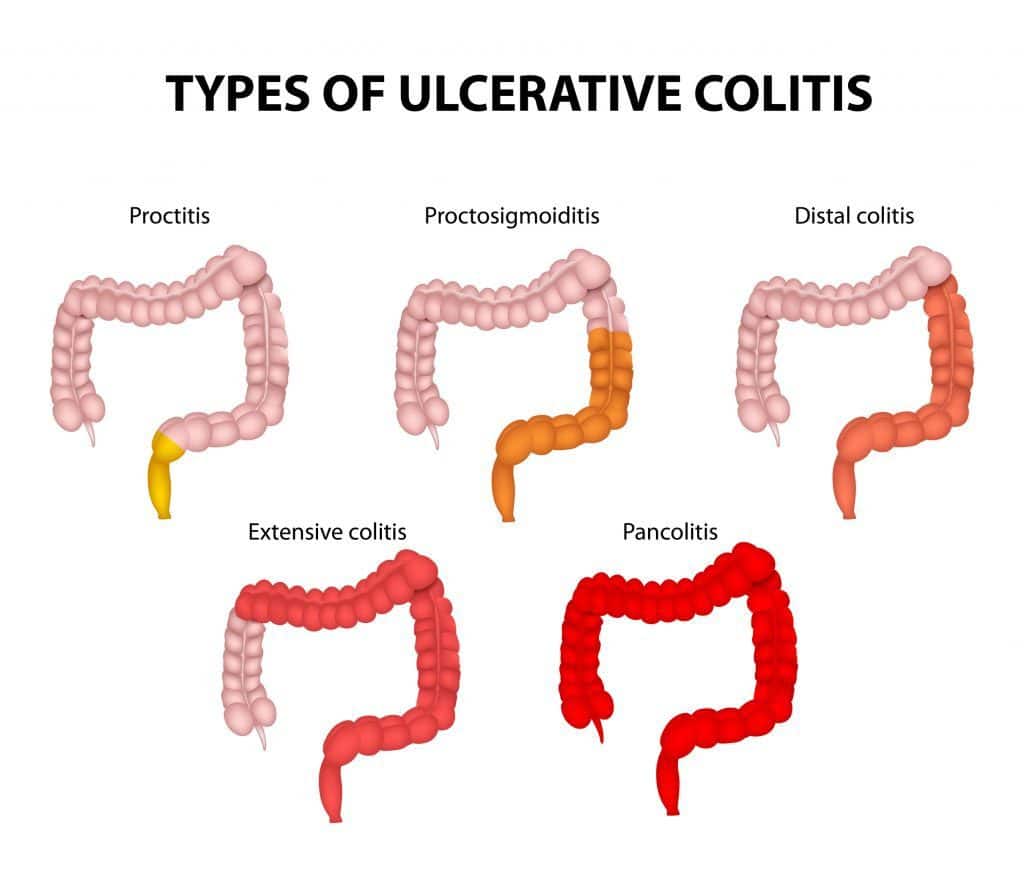
Treatment By Disease Severity And Location
Mild-moderate distal colitis
- Oral aminosalicylates, topical mesalamine, or topical steroids
- Combination of oral and topical aminosalicylates is better than either alone
For refractory cases, oral steroids or IV infliximab can be used
Mild-moderate extensive colitis
- Oral sulfasalazine 4-6 g/day or alternative aminosalicylate 4.8 g/day
- Oral steroids for patients refractory to above therapy + topical therapy
- 6-MP or azathioprine for patients refractory to oral steroids, but not so severe as to require IV therapy
- Infliximab in patients who are steroid refractory/dependant on adequate doses of 6-MP/thiopurine or who are intolerant to these medications
Severe colitis
- Infliximab if urgent hospitalization is not needed
- If patient is toxic, should be admitted to the hospital for IV steroids
- Failure to improve in 3-5 days is indication for colectomy or IV cyclosporine
Indications for Surgery
- Absolute: Hemorrhage, perforation, documented or strongly suspected cancer
Also, surgery is recommended for severe colitis refractory to medical therapy
Why Is My Poop Black/red
Essentially, the brighter red blood is fresher and is associated with the lower gastrointestinal tract. The dark red or black blood is old blood that has already travelled through the GI system for some time. It is associated with the upper GI tract, originating from as far back as the stomach, potentially .
Recommended Reading: What Causes Crohn’s Disease And Ulcerative Colitis
Are There Any Tests For Rectal Bleeding
There are several ways your healthcare provider can evaluate rectal bleeding to help figure out the cause. Your provider might start by asking you about the situation around your rectal bleeding. Some questions may include:
- When did the rectal bleeding start?
- What did you eat the day before seeing the rectal bleeding?
- How frequently do you have a bowel movement?
- Have you been constipated?
- Do you have any inflammatory bowel conditions?
- Do you have a family history of colorectal cancer?
These questions can help your healthcare provider narrow down a possible cause of your bleeding. There are also tests that your provider can do to help determine the cause.
Tests to help diagnose the cause of rectal bleeding can include:
- A sigmoidoscopy.
- A fecal occult blood test .
Your healthcare provider may suggest only one of these tests, or do several of them together to try and discover the cause of your rectal bleeding.
Dont Miss: Is Ulcerative Colitis Considered An Autoimmune Disease
What Is Bloody Stool
Rectal bleeding or bloody stool is when blood is passed out in the faeces when you go to the toilet. Also called gastrointestinal tract bleeding or GI bleeding, this can range from mild to severe bleeding or haemorrhage. In case bleeding is mild and irregular, tests need to be conducted. But heavy bleeding is a medical emergency which must be tended to.
You May Like: Ulcerative Colitis Left Side Pain
Also Check: What Pain Reliever Is Safe For Stomach Ulcer
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Read Also: What Helps With Ulcerative Colitis Pain