Other Key Baseline Assessments
Patients should have an early flexible sigmoidoscopy to assess endoscopic severity and predict outcomes. Intubation to 30 cm should be sufficient and proceeding further is unlikely to impact immediate medical management. To help to exclude Crohns disease, MR or CT enterography may be considered.
Those individuals with severe endoscopic lesions at baseline are more likely to go on to require colectomy. In a study evaluating 85 patients with ASUC in a single centre, 43 of 45 individuals with severe endoscopic lesions went on to have colectomy, while only 9/40 with moderate endoscopic lesions required had colectomy.
Infection with cytomegalovirus is also a consideration. The prevalence estimates of CMV infection in resected colonic specimens from UC patients range from 022%. Infection is more likely to occur in immunosuppressed patients. If a patient has steroid refractory UC, one should take biopsies for tissue immunohistochemistry for CMV. If a patient is responding to infliximab, cyclosporine, or other treatment and is CMV positive, there is no need to treat the CMV as it may just be an innocent bystander. However, if the patient is not responding and is CMV-positive, treatment of the CMV is indicated. Typical treatment is two to three days of IV ganciclovir, then two to three weeks of oral ganciclovir or valcyclovir.. Immunosuppressive therapy should be stopped in the presence of severe systemic CMV.
Role Of Cyclosporine For The Treatment Of Ibd In The Biological Era
Klaudia Farkas, Tamás Molnár
Klaudia Farkas, Tamás Molnár, First Department of Medicine, University of Szeged. 8-10 Koranyi fasor, Szeged, H6720, HungaryCorrespondence to: Tamás Molnár MD, First Department of Medicine, University of Szeged. 8-10 Koranyi fasor, Szeged, H6720, Hungary.Email: molnar.tamas@med.u-szeged.hu Published online: Febuary 21, 2014
Data Extraction Quality Assessment
The following data were extracted from each study : first author, year of publication, study type , drug regimen, the number of patients, age, gender distribution, rate of extensive colitis, concomitant, and maintenance therapy, follow-up period and the definition of ASUC. Intention-to-treat data were extracted from RCTs. If numerical data on long-term colectomy-free survival were not reported , we extracted data from the Kaplan-Meier curves by identifying the values on the axes x and y with a software according to the method proposed by Guyot et al. . Data collection was accomplished by two authors independently . Discrepancies were resolved by consensus. In the case of any disagreement, a third author was involved to resolve conflicts .
Table 1. Study characteristics.
We assessed the risk of bias of observational studies using the Newcastle-Ottawa scale . There is a reliable star system that has three broad perspectives to secure a simple tool for quality assessment: selection and comparability of the groups, and the ascertainment of the outcome. The quality of the included RCTs was assessed with the Cochrane Risk of Bias Tool along seven domains . After the assessment, low, high and unclear risks of bias were indicated with green, red and yellow symbols.
Table 2. Modified Newcastle-Ottawa Scale.
Don’t Miss: Can Lemon Water Help Ulcerative Colitis
Long Term Efficacy Of Infliximab
Long-term benefit of IFX in severe, steroid-refractory UC may be still questionable. A review of Panaccione et al revealed randomized controlled trials, which examined the efficacy of IFX for the treatment of severe steroid-refractory UC. Although the initial results of the studies were controversial, IFX proved to reduce short and long-term colectomy rates among steroid-refractory UC patients. In the paper of Gustavsson et al, the benefit of rescue therapy with IFX in steroid-refractory acute UC was shown to remain after 3 years. 50% of the patients receiving IFX vs 76% receiving placebo had colectomy after 3-year follow up in this study. In the study of Kohn et al 15% of the enrolled patients with severe UC treated with IFX underwent colectomy within 2 months. Early colectomy rates were higher in patients receiving one IFX infusion, compared with those receiving two or more infusions. After a median time of 23 months 82.9% of the patients avoided late colectomy. A retrospective study of 30 patients conducted at Oxford revealed that 53% of the patients required colectomy and only 17% achieved steroid-free remission after a median follow-up of 13 months.
It should be mentioned that IFX had a less pronounced effect in patients with more severe UC than in those with less severe UC in the Jarnerot study and a detectable trough level of IFX was the strongest predictor of remission in the study of Seow et al.
Efficacy Of Intravenous Cyclosporin In Severe Ulcerative Colitis
There have been four controlled studies of intravenous cyclosporin in patients with severe ulcerative colitis. Of 20 patients reported by Lichtiger et al, nine were randomised to receive placebo and 11 to receive cyclosporin 4 mg/kg/day as a continuous infusion for 14 days.2 Nine of 11 cyclosporin treated patients responded compared with none of the placebo treated patients. Those who responded were continued on oral cyclosporin 8 mg/kg/day. At six months, 5/11 cyclosporin treated patients maintained a clinical response.
In the second study, 30 patients were randomised to monotherapy with a continuous infusion of either cyclosporin 4 mg/kg/day or methylprednisolone 40 mg/day.3 After eight days, 9/14 patients who received cyclosporin responded compared with 8/15 who received methylprednisolone. Patients who responded received the same medication orally in combination with azathioprine. At 12 months, 7/9 patients initially controlled with cyclosporin maintained remission compared with 3/8 treated with methylprednisolone.
In the third study, 30 patients were randomised to monotherapy with intravenous cyclosporin 4 mg/kg/day or intravenous cyclosporin in combination with continued prednisolone 1 mg/kg/day.4 After seven days, 10/15 patients in the cyclosporin monotherapy group compared with 14/15 in the combination therapy group had complete remission.
Also Check: History Of Ulcerative Colitis Icd 10
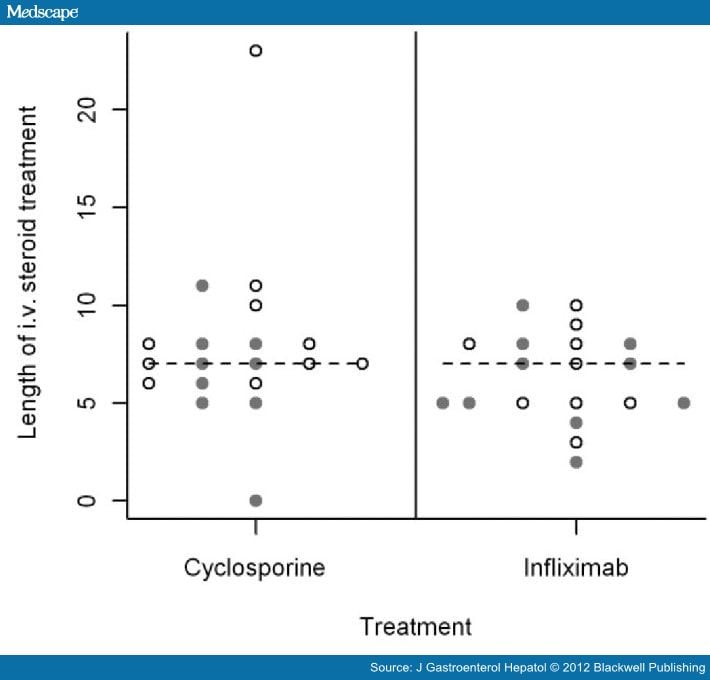
Patients Characteristics And Drug Administration
This retrospective study included two historical cohorts of UC patients with severe relapse refractory to iv steroid treatment administered according to the Oxford regimen. IV steroid resistant UC is defined as a lack of response to an adequate dosage of steroids within 57 days. Criteria for severity were those adopted by both a modified Truelove and Witts and Lichtiger score.,, Severity was also assessed by rectal endoscopy and on clinical grounds. At admittance all patients were evaluated with abdominal x-ray, full blood count, blood chemistry and arterial blood gas analysis, in order to exclude toxic megacolon. Since 1997 human cytomegalovirus detection in rectal biopsies and peripheral blood has also been researched, in order to exclude cytomegalovirus infection . At admittance we alerted the patients and the surgeons about the risk of colectomy.
In patients treated with IFX, azathioprine at the dosage of 2.5 mg/kg daily was started soon after the last infusion. In the CsA group, azathioprine was started together with CsA oral formulation. If previous intolerance or failure of immunosuppressants had been reported, maintenance treatment with azathioprine was excluded.
In the case of a new severe UC flare-up : if this occurred under CsA or IFX treatment a total colectomy was performed. On the contrary a new course of CsA or IFX was started and a colectomy was performed in the case of treatment failure.
Adverse Effects And Safety Profile
Ciclosporin has been in use for many years and in a variety of clinical situations and conditions. The risk of minor side-effects ranges from 31% to 51%,, , and includes tremor, paraesthesia, malaise, headache, abnormal liver function, gingival hyperplasia and hirsutism. Gum hypertrophy and hirsutism are common and troublesome problems with long-term use, but are rarely a significant problem with short-term therapy. Major complications are reported with a frequency from nil up to 17%,, – including anaphylaxis with the i.v. preparation, renal, infectious and neurotoxic effects. The high mortality reported in the Arts et al. study is the consequence of aggressive high-dose therapy, and is not reported in recent papers using lower-dose regimens.
You May Like: What Medications Are Used For Ulcerative Colitis
Adjunctive Medical Treatments To Consider
IBD patients are at increased risk of venous thromboembolism . Prophylaxis for thromboembolism is recommended. Unfractionated or low-molecular-weight heparin is recommended in acutely ill medical patients. A meta-analysis of eight RCTs assessing heparin as adjunctive therapy in UC found no increased bleeding vs. controls.
Routine use of antibiotics is not recommended. Small studies have found no differences in outcome between UC patients that received metronidazole, ciprofloxacin, or tobramycin in addition to steroids vs. steroids alone.
Mode Of Action And Pharmacokinetics
Ciclosporin was isolated in 1970 from a fungus named Tolypocladium inflatum Gams. It is a peptide with potent immunosuppressive effects . It is a lipophilic cyclic undecapeptide that binds with high affinity to its cytoplasmic receptor protein , and the ciclosporinâcyclophilin complex specifically and competitively binds to and inhibits calcineurin, a calcium- and calmodulin-dependent phosphatase. This prevents translocation of a family of transcription factors, nuclear factor of activated T cells , and this reduces activation of genes for IL-2, -3, -4, granulocyte macrophage colony-stimulating factor, TNF-alpha and interferon-gamma. There is also inhibition of T-cell transcription factors AP-1 and NF-kB. Ciclosporin acts predominantly on CD4 cells, and in rheumatoid arthritis there is a shift from Th1 to Th2 type cytokine expression.
Figure 1
Structure of ciclosporin.
Following the oral administration of ciclosporin, the time to peak blood concentration is 1.5â2.0âh. Absorption is affected by several factors including ingestion of food or a fatty meal. The elimination of ciclosporin from the blood is generally biphasic, with a terminal half-life of 5â18âh. Because of preferential distribution of ciclosporin and its metabolites into red blood cells, blood levels are generally higher than plasma levels, and monitoring is by whole-blood monoclonal assay.
You May Like: Can Ulcerative Colitis Lead To Cancer
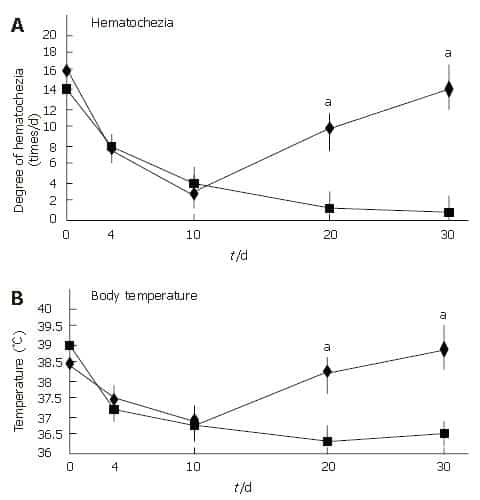
Comparison Between Cyclosporine And Infliximab
Although no specific factor has been identified to differentiate between the patients probably responding to CsA or IFX, hypalbuminaemia, superinfection with Clostridium difficile and deep colonic ulcerations are seems to be bad prognostic factors of responding to either CsA or IFX. Data of Fabros review indicated that new-onset UC, shorter disease duration and more active disease are more frequent in non-responders to IFX therefore in these cases use of CsA is more beneficial than IFX.
Burger et al revealed that short-term adverse events are higher in patients receiving IFX and that thiopurine refractory patients respond less well to CsA. However, the recently published meta-analysis of Chang et al including the data of 321 patients demonstrated that the rates of colectomy at 3 and 12 months, adverse drug reactions, and postoperative complications are equivalent when using IFX or CsA as a rescue therapy in acute, severe UC.
The currently ongoing trial CONSTRUCT with the main goals to determine the clinical and cost effectiveness of IFX and CsA in acute severe steroid resistant UC may help in the decision of the two therapeutic choice.
When To Consider Steroids A Failure
Consider second-line medical therapy or surgery in patients who fail to improve on intravenous steroids within 72 hours. Improvement should be assessed by clinical, radiological, and laboratory parameters. There are numerous scoring systems to predict failure to steroids the best validated is the Oxford criteria. Poor outcomes are predicted when there are > 8 stools/day on day 3, or when there are 38 stools/day and CRP > 45 mg/L.
The timing of decision-making at day 3 is supported by a study that evaluated outcomes in those who underwent colectomy after steroid failure, and found that post-operative morbidity and mortality is higher in those who were on steroids for a longer period of time before having surgery .
Read Also: Best Remedy For Stomach Ulcer
A Novel Player: Cyclosporine Therapy In The Management Of Inflammatory Bowel Disease
Simcha Weissman1, Abimbola Chris-Olaiya2, Tej I. Mehta3, Muhammad Aziz4, Ali Alshati5, Rani Berry6, Rawish Fatima7, Sindhura Kolli8, Ammar Hassan9, Michael A. Sciarra9
1Department of Medicine, Hackensack University-Palisades Medical Center, North Bergen, NJ, USA Grand Strand Regional Medical Center , University of South Dakota Sanford school of Medicine , University of Kansas Medical Center , 5Department of Medicine, Maricopa Integrated Health System, Creighton University Ronald Reagan UCLA Medical Center , University of Toledo Medical Center , 9Division of Gastroenterology and Hepatology, Hackensack University-Palisades Medical Center, North Bergen, NJ, USA .
Correspondence to:
Keywords: Inflammatory bowel disease Crohns disease ulcerative colitis cyclosporine
Received: 08 May 2019 Accepted: 15 August 2019 Published: 10 September 2019.
doi: 10.21037/tgh.2019.08.08
Medical Management Of Acute Severe Ulcerative Colitis
May 28, 2019 – Classic Edition | IBD Dialogue | Volume 15 2019
Issue 04
Mentoring in IBD is an innovative and successful educational program for Canadian gastroenterologists that includes an annual national meeting, regional satellites in both official languages, www.mentoringinibd.com, an educational newsletter series, and regular electronic communications answering key clinical questions with new research. This issue is based on the presentation made by the contributing editor, Dr. Neeraj Narula, at the annual national meeting, Mentoring in IBD XIX: The Master Class, held November 2, 2018 in Toronto, Ontario.
You May Like: Special Mattress For Pressure Ulcers
Steroid Use And Predictors Of Steroid Failure
Most patients with ASUC should be treated initially with intravenous corticosteroids. However, indications for early surgery include: massive hemorrhage toxic megacolon with impending or frank perforation co-existent colorectal cancer or dysplasia longstanding colitis with intractability and medical noncompliance .
Failure Of Rescue Therapy
Longer periods of uncontrolled inflammation are more likely to lead to adverse outcomes, including toxic megacolon, perforation, severe hemorrhage, thromboembolism, infection and mortality. If a patient is not improving or is deteriorating on rescue therapy with cyclosporine or infliximab, he or she should be referred for colectomy.
Read Also: What Should I Eat If I Have An Ulcer
Toxicity Associated With Intravenous Cyclosporin
Of 111 patients with inflammatory bowel disease treated with intravenous cyclosporin 4 mg/kg/day, the most common toxic effects were paresthesias , hypertension , and hypomagnesaemia .8 Major toxicities reported were renal insufficiency , infections , seizures , death , and anaphylaxis . Low dose intravenous cyclosporin may be associated with lower rates of toxicity.5 Both hypocholesterolaemia and hypomagnesaemia significantly increase the risk of seizures in patients treated with intravenous cyclosporin.9
Cyclosporine A For Induction Of Remission In Severe Ulcerative Colitis
Ulcerative colitis is a chronic inflammation of the large bowel. Symptoms include bloody diarrhea and abdominal pain. The disease can also have manifestations outside the bowel with involvement of the joints, skin, eyes and liver. While the ‘first line’ treatment for a severe attack of UC is usually steroids the options for patients not responding to steroids are limited and include surgical removal of the large bowel. Cyclosporine A , a drug effective in preventing transplant organ rejection by suppressing the immune system, was tried in severe UC with encouraging results in the early 1990’s. The aim of this review was to assess the effectiveness of CsA for severe UC. The literature search identified 36 studies. Only 2 studies were of high methodological quality and both support the use of CsA in UC patients with a severe attack. However, both studies were small and limited in the length of follow-up . There is limited evidence that cyclosporine is more effective than standard treatment for severe ulcerative colitis. The conclusion of the review is that while the data concerning the use of CsA in severe UC are encouraging, more studies are needed.
Also Check: Symptoms Of Crohn’s Disease And Ulcerative Colitis
Characteristics Of The Studies Included
The main characteristics of the included studies are listed in Table 1. The studies were published between 2004 and 2018 and the follow-up period ranged at least from 1 year to maximum of 10 years. In the quantitative analysis, we used data from three RCTs and 12 cohort studies . A total number of 1,607 patients with steroid-refractory ASUC were included, 879 of which were treated with CYS and the other 728 with IFX. The most common definitions of ASUC used in the studies were the Truelove and Witts criteria, the Mayo and the Lichtiger scores . Three of the 15 articles were published only in conference abstract form .
In most of the studies, the standard 2 mg/kg/day IV CYS regimen was applied, oral CYS was used for induction of remission only in two studies . After the oral CYS bridging, AZA maintenance therapy was continued in all studies. Standard 5 mg/kg dose of IFX was administered in multiple IV infusions following the induction protocol. Only two studies reported a single infusion of IFX . In the IFX treatment groups, AZA was the most commonly administered maintenance drug, albeit recent studies continued IFX . Due to the lack of available safety data during long-term follow-up in an RCT, the CYSIF trial , AE and SAE results reported in the original study were used in the meta-analysis .
Switching Between The Two Drugs
Shifting from CsA to IFX and vice versa after the failure of the other drug seems to be an obvious therapeutic method, although the risk of toxicity is supposed to increase in these cases. Deciding the order of the therapies should also be considered because of the different pharmacokinetic characteristics of the drugs. Only one study examined the outcomes of CsA and IFX treatment after the failure of the other drug in severe, steroid-refractory UC and achieved colectomy free remission in one third of the patients with the salvage therapy.
Chaparro et al examined the efficacy and safety of IFX after CsA failure in patients with steroid refractory UC in a retrospective review. They found that after the first IFX infusion, 13% of the 47 patients achieved remission, and 74% partial response. Of the 35 patients who received the third IFX infusion, 60% achieved remission, and 37% partial response. 30% underwent colectomy. They concluded that IFX might avoid colectomy in two-thirds of patients with corticosteroid- refractory UC after failure of CsA. However, the rate of adverse events was 23%.
Due to the potentially high rate of short- and long-term complications, second line medical therapy however should be considered very cautious.
Read Also: Ulcerative Colitis And Canker Sores