Information Sources And Searches
Guidelines, systematic reviews, reports, online documents, and books were searched as long as they met the inclusion criteria. A combined search of the Embase and Medline databases was conducted via OVID . Available systematic reviews22, 23 were used to search for the original publications. In addition, numerous databases and websites were searched, including:
Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin < 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
When You Need More Treatment
If your wound doesnât heal in about a month or becomes an infection that spreads to the bone, you may need other treatments. These can include surgery and hyperbolic oxygen therapy, which involves breathing pure oxygen in a special room in order to help your body heal.
If your ulcer develops gangrene and your tissue dies, your doctor may have to amputate that area of your body.
Recommended Reading: Is Garlic Good For Ulcerative Colitis
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Treatments For Pressure Ulcers
Treatments for pressure ulcers depend on how severe they are.
For some people, they’re an inconvenience that needs basic nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning.
Ways to stop pressure ulcers getting worse and help them heal include:
- applying dressings that speed up the healing process and may help to relieve pressure
- moving and regularly changing your position
- using specially designed static foam mattresses or cushions, or dynamic mattresses and cushions that have a pump to provide a constant flow of air
- eating a healthy, balanced diet
- a procedure to clean the wound and remove damaged tissue
Surgery to remove damaged tissue and close the wound is sometimes used in the most serious cases.
Read more about the treatments for pressure ulcers.
Don’t Miss: What Are The Symptoms Of Having A Stomach Ulcer
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.
How Can Pressure Ulcers Be Treated
It is important to watch out for early signs of pressure ulcers and to contact your doctor if you notice any changes to the skin. Ulcers are best managed early on, and your doctor will assess whether your pressure ulcer can be managed at home, if you need a referral to a wound specialist or if you require treatment at hospital.
Use healthdirects Service Finder tool to locate your nearest GP or nurse clinic.
Wound dressings can enhance healing. Your healthcare team will select the most appropriate treatment and dressing, depending on your specific pressure ulcer. There are 6 classes of dressings:
- film dressings
- foam dressings
- alginate absorbent fibre dressings
Depending on the type of pressure ulcer, a bandage may also be applied to keep the dressing in place or support the injured area.
To promote healing and recovery, it is important to eat a balanced diet that includes protein, carbohydrates, fats and sufficient fluids.
Other treatments may include antibiotics if the ulcer becomes infected, or debridement a procedure used to clean the wound and remove any damaged tissue.
You May Like: Mouth Ulcer Vitamin B Complex
Can Bedsores Be Prevented
Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas. Other methods of preventing bedsores and preventing existing sores from getting worse include:
- Turning and repositioning every 2 hours
- Sitting upright and straight in a wheelchair, changing position every 15 minutes
- Providing soft padding in wheelchairs and beds to reduce pressure
- Providing good skin care by keeping the skin clean and dry
- Providing good nutrition because without enough calories, vitamins, minerals, fluids, and protein, bed sores cant heal, no matter how well you care for the sore
Failure Of Reactive Hyperaemia
In patients with a failure of reactive hyperaemia, the tissues are no longer able to recover from ischaemic episodes, and pressure ulcer prevention is probably most difficult in this group. Failure of reactive hyperaemia can occur in very sick and dying patients in whom there is insufficient peripheral blood pressure to refill capillary beds emptied by compression. Clinically, this presents as white patches in pressure areas which do not change colour rapidly to the red of reactive hyperaemia, as they would in a healthy person. Rather, the white patches remain for many minutes before slowly returning directly to a more normal skin colour with little or no reactive hyperaemia being observable. Similar effects can be seen in critical care patients who are on high doses of inotropes, such as adrenaline.
Since individuals in the same diagnostic category can have either a normal or pathological circulatory response to repeated loading , this may well explain why some patients are more prone to pressure ulceration than others with the same diagnosis .
Read Also: What Is Moderate Ulcerative Colitis
How Are Pressure Sores Diagnosed
Your doctor will do a physical exam to look at the sores. They will examine the size and depth of the sore and look to see if blood or fluid is oozing from the sore. Your doctor will check to see if your sore has a bad smell. They also will check for additional sores.
Testing may help to diagnose pressure sores or their complications. These tests might include a blood test. Another test would be to take a sample of the tissue from the sore. This is done by scraping or cutting it from the sore. That sample is sent to the lab for examination.
Checklist For Assessing Readiness For Change
This and other end-of-chapter checklists are designed to provide toolkit users with ways to check their progress through the assessment and implementation steps discussed in the toolkit. They may be useful in ensuring that toolkit users have not skipped essential steps in pursuing their pressure ulcer prevention efforts.
1. Organizational Readiness Checklist
Don’t Miss: How To Get Rid Of Peptic Ulcer
What Is A Pressure Ulcer
A pressure ulcer, also known as pressure sore or bed sore, is a wound caused by prolonged pressure on the skin. Typical locations for pressure sores are are the heels, ankles, hips and over the tailbone. Elderly people and bed- or wheelchair-bound are at risk of developing this condition.
Symptoms may include pain in the area, red or purple skin, a break in the skin and, eventually, a wide-based sore which may get bigger over time. The diagnosis is usually easily based on the symptoms and appearance of the area of skin. Treatment involves taking steps to avoid pressure on the area, to keep the wound healthy and, if needed, to close the ulcer. If the wound is small, it may heal well, but large, complicated ulcers can take weeks to months to heal.
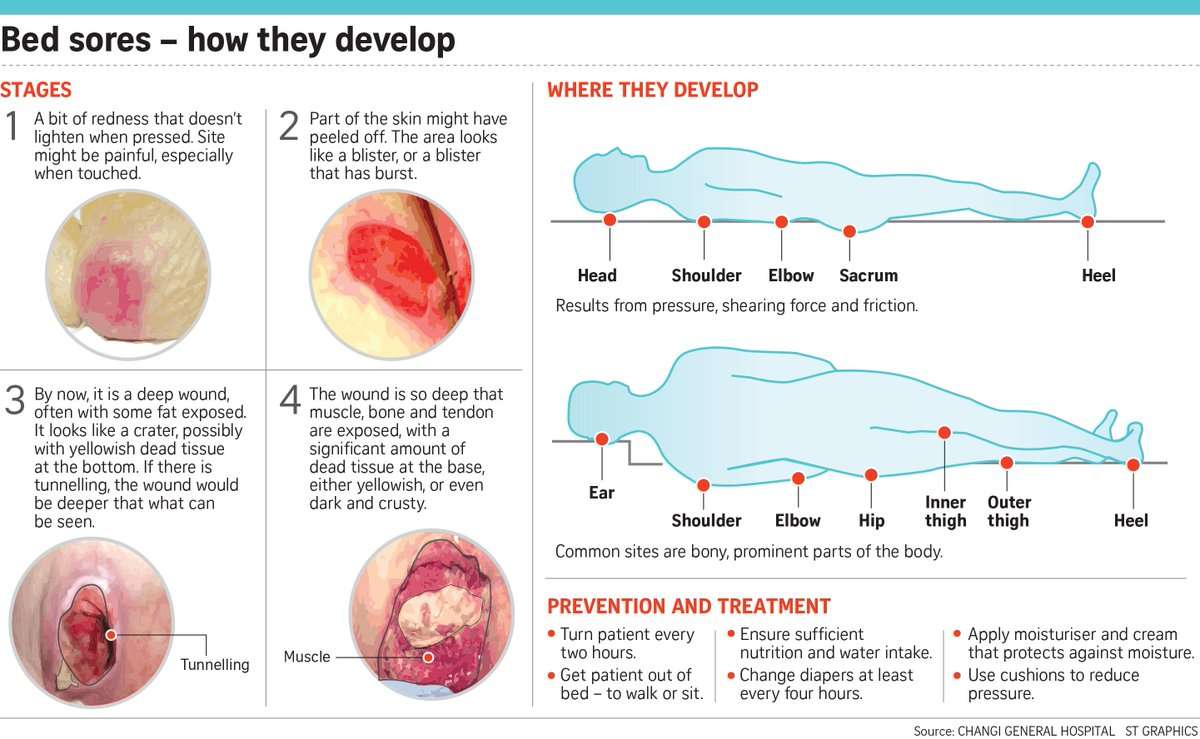
What Are The 4 Stages Of Pressure Ulcers
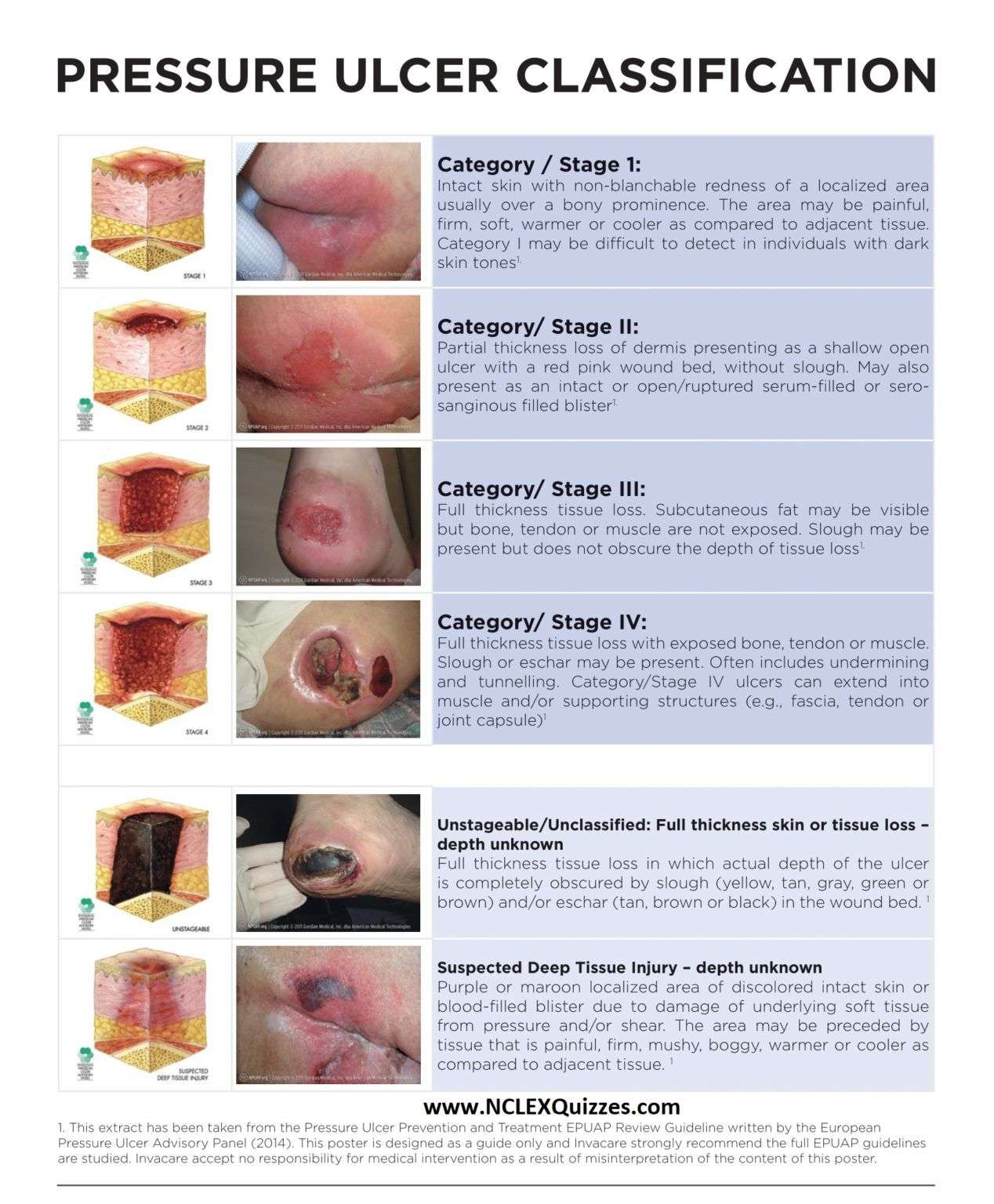
You might hear medical staff refer to pressure ulcers in stages. Stage 1 is less severe, while an ulcer can progressively increase in severity to stage 4.
The 4 stages of pressure ulcers are:
|
Stage 1 |
The skin is red, but not broken. When you press the skin, it does not turn white. |
|
|
Stage 2 |
There is some damage to the outer layer of skin. The pressure ulcer looks like a shallow, open wound with a redish-pink centre. It can also look like a blister that may or may not have opened. |
|
|
Stage 3 |
There is full loss or damage of the skin. The wound looks quite deep but is still limited to the skin layers. |
|
|
Stage 4 |
There is full loss or damage of the skin it is deep and goes all the way to the underlying bone, tendon or muscle. |
Also Check: Cpt Code For Ulcerative Colitis
Symptoms Of Pressure Ulcers
The parts of the body most at risk of developing pressure ulcers are those that are not covered by a large amount of body fat and are in direct contact with a supporting surface, such as a bed or a wheelchair.
For example, if you are unable to get out of bed, you are at risk of developing pressure ulcers on your:
- shoulders or shoulder blades
- knees, ankles, heels or toes
- spine
- tail bone
If you are a wheelchair user, you are at risk of developing pressure ulcers on:
- your buttocks
- the back of your arms and legs
- the back of your hip bone
How Is A Pressure Sore Diagnosed
Your doctor or nurse will diagnose a pressure sore by examining your skin. They will establish how severe it is to determine what treatment is best for you. If they think the pressure sore is infected, they may take a swab around your skin to find out the cause of the infection.
Daily checks are needed to look for early warning signs such as red, purple or blue torn or swollen skin, especially over bony areas, or for signs of infection, such as skin warmth, swelling, cracks, calluses and wrinkles.
You May Like: How To Treat Rodent Ulcers In Cats At Home
Position Changes To Prevent Pressure Sores
If you use a wheelchair shift position within your chair about every 15 minutes. If you spend most of their time in bed change position at least once every two hours, even during the night and avoid lying directly on your hipbones.
Pillows may be used as soft buffers between your skin and the bed or chair. The head-of-bed elevation should be maintained at/or below 30 degrees. Or depending on the your medical condition, the bed should at least be elevated to the lowest degree to prevent injury. When lying on your side, a 30 degrees position should be used.
Symptoms Of Pressure Sores
Pressure sores go through 4 stages.
- Stage 1. During this stage, the area of the sore looks red. It may feel warm to the touch. It may burn, hurt, or itch. The pressure sore may look blue or purple in people who have dark skin.
- Stage 2. During this stage, the area is more damaged. The sore may be open. It may look like a cut or blister. The skin around the sore may be discolored. The sore is painful.
- Stage 3. During this stage, the sore will have a crater-like look. This is due to increased damage below the surface. This makes the wound deeper.
- Stage 4. This is the most serious stage. Skin and tissue are severely damaged. The sore becomes a large wound. Infection is possible. Youre likely able to see muscle, bones, tendons, and joints.
Infected pressure sores take a long time to heal. Also, the infection can spread to the rest of your body. Signs of infection at the site include:
- Thick, yellow, or green pus
- A bad smell coming from the sore
- Redness or skin that is warm to the touch
- Swelling around the sore
Signs that the infection has spread include:
- Fever
- Weakness
You May Like: Natural Cure For Stomach Ulcer
How Can I Tell If I Have A Pressure Sore
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
You May Like: Does Ulcer Pain Come And Go
What Are Pressure Sores
Pressure sores are sores on your skin. Theyre caused by being in a bed or wheelchair nearly all the time. Sometimes theyre called bedsores or pressure ulcers. The sores usually develop over the bony parts of your body. Those are places with little padding from fat. Sores are common on heels and hips. Other areas include the base of the spine , shoulder blades, the backs and sides of the knees, and the back of the head.
People who need to stay in bed or in a wheelchair for a long time are at greater risk of developing pressure sores. This can include people who are paralyzed and those who arent able to get up on their own. But even some people with short-term illness and injuries can get pressure sores. Sores can happen if they have to stay in bed or a wheelchair while they heal. Lastly, some chronic diseases make it hard for pressure sores to heal. Those include diabetes and hardening of the arteries.
How Pressure Sores Develop
Blood flows through the bodys tissues, including the skin. If you press your finger down on a spot your arm and then quickly remove your finger, you will see that the skin changes color for a second or so in that spot because you stopped the blood flow. The longer your finger remains, the longer the blood flow stops. This is how a pressure ulcer forms.
Someone who cannot move about in bed or on a chair is at highest risk of developing pressure ulcers wherever their body is in contact with the bed or chair, no matter how soft the mattress or cushioning may be. Although a pressure sore can occur anywhere on the body, the most common places are the:
- Coccyx
- Ears
- Heels
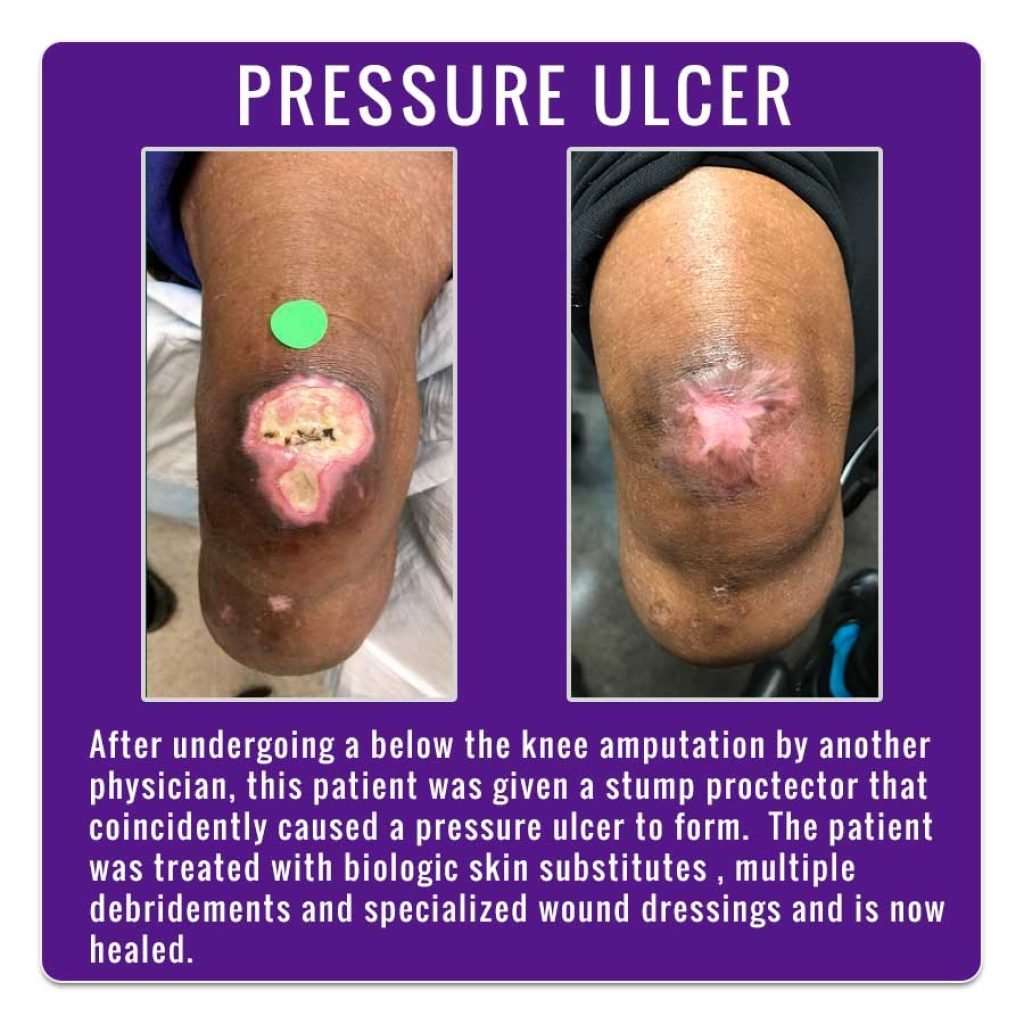
- Ankles
People who use prosthetics after a leg or arm amputation are also at risk for pressure sores if their prosthetics dont fit properly or if there is a problem with the skin that comes in contact with the device.
Read Also: How To Calm Ulcerative Colitis Flare Up