How To Treat Pressure Ulcer
When Pressure ulcers are in the early stages, people may be able to treat them at home. Frequently changing positions can help the ulcers heal and keep new ones from forming.
Pressure ulcers can be prevented by periodically repositioning yourself to avoid stress on the skin. Other strategies include taking good care of the skin, maintaining good nutrition and fluid intake, quitting smoking, managing stress, and exercising daily.
MaxioCel, an advanced wound dressing product, provides faster healing to patients suffering from chronic wounds, such as pressure ulcers, diabetic foot ulcers, venous leg ulcers, cavity wounds, and skin abrasions to name some.
MaxioCel range of advanced chitosan dressings has the potential to address this gap and be a real game-changer. With a range of MaxioCel products, millions of patients who need advanced wound care products are being treated every year. MaxioCel with its 360-degree care combined hemostatic, pain management, and scar improvement properties, fulfills a large gap in the market.
Juwariah Khan
Recommended Reading: Best Treatment For Stomach Ulcers
Pressure Ulcer Of Unspecified Site Stage 4
- 2016201720182019202020212022Billable/Specific Code
- L89.94 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.94 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.94 other international versions of ICD-10 L89.94 may differ.
- Healing pressure ulcer of unspecified site, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, unspecified site
- Applicable To annotations, or
Read Also: How To Use Aloe Vera Gel For Ulcerative Colitis
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- Sepsis may occur when the body overreacts to a serious infection, such as an infection stemming from a stage 4 bedsore. The immune system gets overstimulated and attacks healthy body parts. Severe cases of sepsis can lead to septic shock, which occurs when blood pressure drops due to an infection. Septic shock can be deadly as major organs may shut down.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a wrongful death if a nursing home patient dies from an untreated bedsore.
You May Like: Foods To Avoid With Bleeding Ulcer
L895 Pressure Ulcer Of Ankle
Pressure ulcer of unspecified ankle
Pressure ulcer of right ankle
Postoperative And Rehabilitation Care
Postoperative care of patients who have undergone reconstructive surgery is of utmost significance as these ulcers have high rates of recurrence. A study done on characteristics of recurrent pressure ulcers showed that patients who underwent reconstructive surgery and developed post-operative, had an 11% to 19% chance of recurrence. Those without any postoperative complications had recurrence as high as 61%.
When medical staff shift patients from the operating table to their air-fluid beds, they must avoid excessive shearing, and stretch on skin flaps. For the first four weeks, patients are positioned flat on their support surfaces, after which they can place themselves in a semi-sitting position. The patient starts to sit for 10 minutes only after six weeks of the surgical procedure. After these sitting periods, the flap should be examined for discoloration and wound edge separation. Over two weeks, the sitting periods will increase to 2 hours in 10-minute increments. Patients will also learn to lift for 10 seconds every 10 minutes to relieve pressure. Meticulous skincare is necessary.
Recommended Reading: Snack Ideas For Ulcerative Colitis
Don’t Miss: How Do You Get Ulcers In Your Mouth
How To Measure A Sacral Wound
Learn about how to stage and treat this type of ulcer. The scale assesses levels of sensory perception, moisture, activity, mobility, nutrition, and friction.
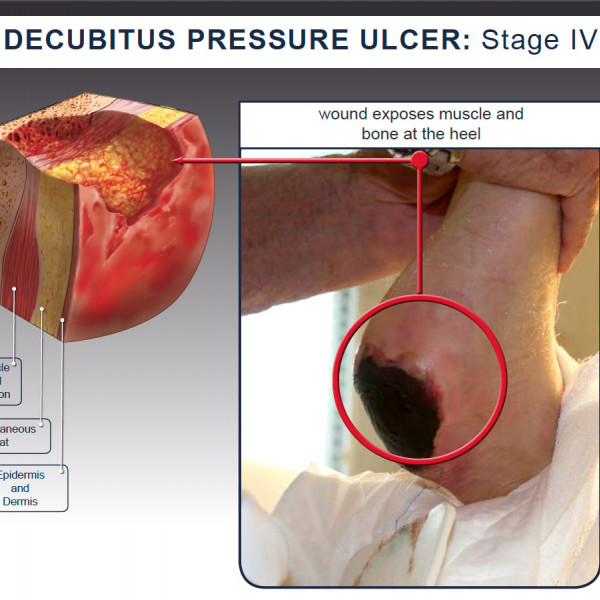
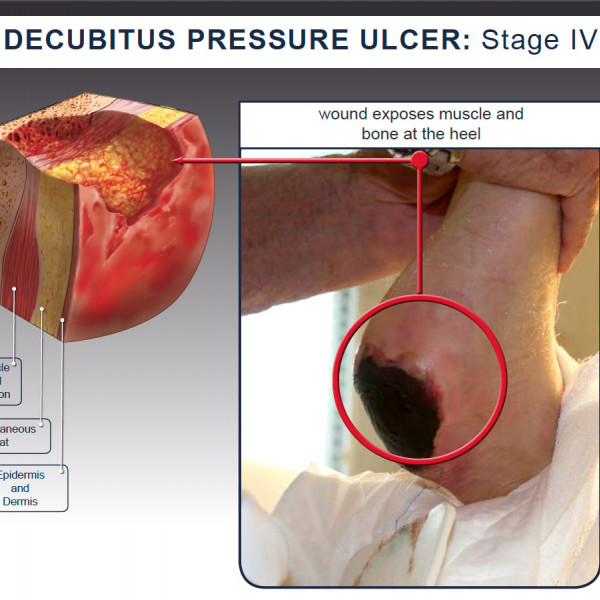
Pressure Ulcer Stage Iv Pressure Ulcer Classifications
Enhancing Healthcare Team Outcomes
The main goal is to prevent a decubitus ulcer by decreasing the pressure acting on the affected site. This goal requires an interprofessional team, including primary care providers, wound care specialists, surgeons, specialty-trained wound nurses, physical therapists, and nurses aides. Nurses provide care, monitor patients, and notify the team of issues. Nurses aides are often responsible for turning and repositioning patients. Air-fluidized or foam mattresses should be used, frequent postural changes, provision of adequate nutrition, and treatment of any underlying systemic illnesses. Debridement should take place to remove dead tissue that serves as the optimum medium for the growth of bacteria. Hydrogels or hydrocolloid dressing should be used, which aid in wound healing. Tissue cultures are necessary, so the most directed antibiotic can be administered, which can involve the pharmacist and the latest antibiogram data. The patient should be kept pain-free by giving analgesics. They should try to increase physical activity if possible, which a nurse’s aide, medical assistant, or rehab nurse can facilitate. Frequent follow-ups are an absolute necessity and a team approach to patient education and management involving the wound care nurse and wound care clinician will lead to the best results. These interprofessional activities can help drive better outcomes for patients with decubitus ulcers.
Don’t Miss: How To Get Rid Of Stomach Ulcer Pain
Pressure Ulcer And Non
Pressure ulcer and non-pressure chronic ulcer diagnostic codes are located in ICD-10-CM chapter 12, Disease of the skin and subcutaneous tissue. The concept of laterality is pertinant, and should be included in the clinical documentation for skin ulcers.ICD-10-CM codes for Pressure ulcers, located in Category L89, are combination codes that identify the site, stage, and the laterality of the ulcer. Possible stages are 1-4 and unstageable.
Stage 1: Skin changes limited to persistent focal edemaStage 2: An abrasion, blister, and partial thickness skin loss involving the dermis and epidermisStage 3: Full thickness skin loss involving damage and necrosis of subcutaneous tissueStage 4: Necrosis of soft tissues through the underlying muscle, tendon, or bone
Unstageable: Based on clinical documentation the stage cannot be determined clinically or for ulcers documented as deep tissue injury without evidence of trauma.An instructional note in ICD-10 states to code also any associated gangrene .Non-pressure chronic ulcers are similar to pressure ulcers in that they require documentation of the site, severity, and laterality. Category L97 and L98 are for Non-pressure ulcers, and have an instructional note to code first any associated underlying condition, such as:
Associated gangreneAtherosclerosis of the lower extremitiesChronic venous hypertensionThe severity of the ulcers is described as:Limited to breakdown of skinWith fat layer exposedWith necrosis of muscleWith necrosis of bone
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Hereâs how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesnât rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you canât see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
You May Like: How To Heal Mouth Ulcers
Recommended Reading: Best Mattress For Pressure Ulcers
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
- the Cochrane Wounds Specialised Register
- the Cochrane Central Register of Controlled Trials
We also searched the following clinical trials registries:
- ClinicalTrials.gov
Searching other resources
Recommended Reading: Aloe Vera Gel For Horses Ulcers
What Do Stage 4 Bedsores Look Like
Characterized by severe tissue damage, a stage 4 bedsore is the largest and deepest of all bedsore stages. They look like reddish craters on the skin. Muscles, bones, and/or tendons may be visible at the bottom of the sore.
An infected stage 4 pressure ulcer may have a foul smell and leak pus. Additionally, the sore may be surrounded by dead tissue thats dark or yellowish in color.
What Increases The Risk Of Developing Pressure Ulcers
People who are confined to a bed or chair for example due to stroke, spinal injury or dementia are at greater risk of developing extensive pressure ulcers. Other risk factors include:
- immobility being confined to bed after an illness or surgery, or due to paralysis
- diabetes and other health conditions that can affect blood supply
Read Also: How Effective Is Humira For Ulcerative Colitis
You May Like: Over The Counter Remedies For Ulcers
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Donât Miss: Best Things To Eat With Ulcerative Colitis
Common Areas To Monitor For Bedsores
Depending upon the circumstances, bedsores will manifest on different areas of the body. For example, a person who is confined to a wheelchair will have different areas of the body affected as opposed to someone who is confined to a bed. Caregivers should monitor residents based on their mobility levels and overall health.
Recommended Reading: How Is Ulcerative Colitis Caused
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation |
|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Summary Of Main Results
We have successfully conducted a network metaanalysis of dressings and topical agents for healing pressure ulcers. Alongside the analysis we have applied a new method of GRADE assessment , which allows us to view the results in the light of our certainty in their findings. Using this approach, we found the majority of the evidence to be of low or very low certainty, and was mainly downgraded for risk of bias and imprecision . This level of uncertainty within the totality of the dataset impacts on all subsequent interpretation of its outputs.
This review includes 51 RCTs involving a total of 2964 participants, comparing 39 different dressings or topical agents for the healing of pressure ulcers. Most of the studies were in older participants, but four included participants with spinal cord injuries and one was in younger people said to be chronically ill or physically disabled. Seventeen studies included participants mainly with Stage 2 pressure ulcers and 15 mainly had Stage 3 pressure ulcers 13 studies investigated treatment of ulcers with a mean duration of less than three months.
We treated each topical agent as a separate intervention, but initially grouped dressings by class as described in the BNF 2016 . The network involved 39 studies in 2116 participants, encompassing 21 different interventions in 27 direct contrasts and these informed 210 mixed treatment contrasts.
Recommended Reading: Can Urgent Care Treat Ulcers
Deterrence And Patient Education
Patients and their family members should have a clear idea that preventing recurrence requires commitment and responsibility. They should receive education on how to manage the condition in the hospital and as well as in their homes. They should be familiar with warning signs like skin discoloration, ulceration, discharge, or a foul smell from the ulcer site and body areas with decreased or no sensation.
The patient should move or turn every 2 hours it could not be done by themselves, or they should ask someone to help them. Air or water mattress should be used in their homes too. Their food intake should be adequate and should consist of a balanced and healthy diet.
Read Also: Bland Diet Recipes For Ulcers